Ocular Hypertension: Understanding Causes, Risks, and Management
Learn how elevated eye pressure affects your vision, what causes it, who is at risk, and how proper management can prevent eye health complications.
Ocular Hypertension: Causes, Symptoms, Treatment
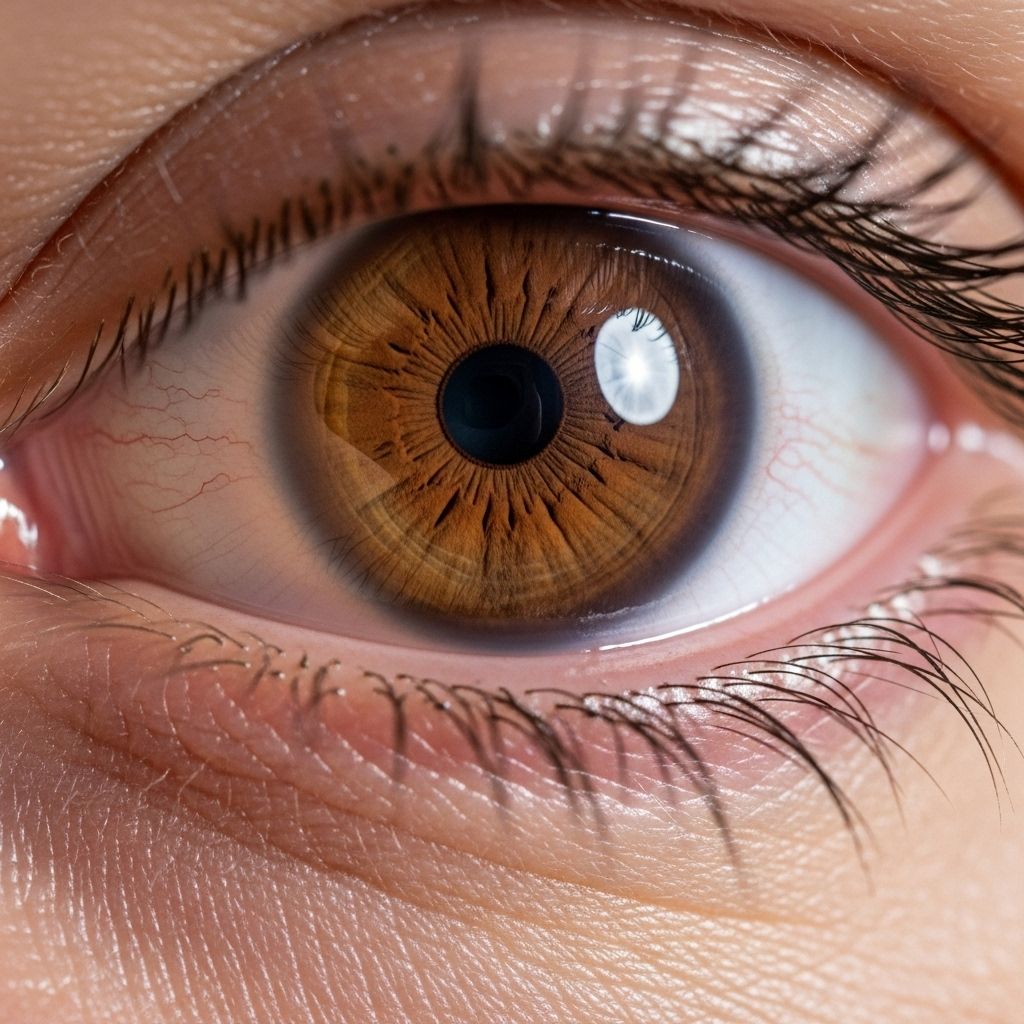
Ocular hypertension is a common condition where the pressure inside your eye—known as intraocular pressure (IOP)—is higher than normal. Unlike glaucoma, ocular hypertension does not initially cause detectable damage to the optic nerve or any noticeable vision loss. However, unchecked and unmanaged ocular hypertension can increase your risk of developing glaucoma and other vision problems, making early diagnosis and effective management crucial for long-term eye health.
What is Ocular Hypertension?
Ocular hypertension describes a state where the pressure inside the eye (IOP) consistently measures above the normal range, yet the optic nerve appears healthy, and there are no signs of visual field loss. Normal eye pressure typically ranges between 10 and 21 millimeters of mercury (mm Hg). When IOP exceeds 21 mm Hg without signs of nerve damage or visual disturbances, it’s classified as ocular hypertension.
- IOP above 21 mm Hg with healthy optic nerve and no vision loss defines ocular hypertension.
- It is distinct from glaucoma, which involves both high IOP and optic nerve damage.
- The condition is typically asymptomatic, highlighting the importance of regular eye exams for detection.
How Does Eye Pressure Work?
The eye contains a clear fluid called aqueous humor, produced by the ciliary body. This fluid circulates through the front part of the eye and drains out via a drainage system known as the trabecular meshwork. When fluid is produced and drained at equal rates, eye pressure remains balanced. Problems occur when drainage is reduced or blocked, resulting in fluid buildup and increased IOP.
- Aqueous humor: Fluid maintaining eye shape and nourishing internal structures.
- Trabecular meshwork: Main drainage area for fluid at the eye’s angle.
- When drainage is compromised, fluid accumulates, and eye pressure rises.
Causes of Ocular Hypertension
Ocular hypertension arises when the eye’s natural drainage process malfunctions, but multiple other factors can contribute to increased eye pressure:
- Reduced outflow of aqueous humor: The most common cause due to partial blockage or inefficiency of the trabecular meshwork.
- Increased production of fluid: More aqueous humor than the eye can efficiently drain elevates IOP.
- Eye injury: Trauma to the eye can damage drainage tissues or cause bleeding and swelling, increasing pressure.
- Eye medications: Corticosteroid eye drops or systemic steroids may heighten IOP in some individuals.
- Other health conditions: Diseases such as pseudoexfoliation syndrome or pigment dispersion can block outflow channels.
Risk Factors for Developing Ocular Hypertension
Certain factors can increase an individual’s likelihood of developing ocular hypertension:
- Age: Risk increases as you get older, especially after age 40.
- Family history: A family history of glaucoma or ocular hypertension raises your risk.
- Ethnicity: People of African, Afro-Caribbean, or Hispanic descent are at higher risk, particularly for subsequent glaucoma.
- Thin corneas: A thinner central corneal thickness can lead to underestimation of IOP during measurements and is a risk factor for progression to glaucoma.
- Medical conditions: Diabetes, high blood pressure, and nearsightedness (myopia) are associated with raised risk.
- Use of certain medications: Long-term use of corticosteroids can lead to increased eye pressure.
- Eye trauma: Past injuries may damage the eye’s drainage system, resulting in chronic pressure elevation.
Symptoms of Ocular Hypertension
Ocular hypertension itself typically has no symptoms. Most individuals are unaware of elevated eye pressure because it does not cause pain, discomfort, or vision changes in its early stages. As a result, people with the condition are usually diagnosed during routine comprehensive eye examinations.
- High IOP is not directly felt by the patient.
- There are no visible signs or noticeable symptoms in most cases.
- If left untreated, it can progress to glaucoma, which may cause vision loss.
Diagnosing Ocular Hypertension
Because ocular hypertension does not cause symptoms, it is commonly discovered during an eye health exam. A comprehensive eye exam for diagnosis typically includes:
- Tonometer test (Tonometry): Measures the pressure inside the eyeball in millimeters of mercury (mm Hg).
- Ophthalmoscopy: Examines the optic nerve for early signs of damage associated with glaucoma.
- Pachymetry: Measures the thickness of the cornea, as thin corneas can affect the accuracy of pressure readings.
- Visual field test (Perimetry): Checks for any loss in side (peripheral) vision, which can be an early sign of optic nerve damage.
- Gonioscopy: At times, doctors assess the angle where the cornea and iris meet to ensure the drainage angle is open and functioning normally.
Is Ocular Hypertension the Same as Glaucoma?
| Ocular Hypertension | Glaucoma |
|---|---|
| Elevated eye pressure (>21 mm Hg) without optic nerve damage or vision loss | Usually elevated eye pressure with optic nerve damage and/or visual field loss |
| No detectable vision problems; considered a risk state | Progressive, irreversible vision loss if untreated |
| Potentially reversible with treatment; requires monitoring | Requires ongoing treatment to prevent further damage |
Ocular hypertension is not glaucoma, but it is considered a major risk factor for developing primary open-angle glaucoma, the most common form of the disease.
How is Ocular Hypertension Treated?
The primary goal of treating ocular hypertension is to lower eye pressure and reduce the risk of developing glaucoma. Not every person with mildly elevated eye pressure needs immediate treatment. Instead, management decisions are based on:
- Measured IOP level
- Family and medical history
- Corneal thickness and structure of the optic nerve
- Presence of other risk factors (e.g., diabetes, ethnicity)
- Visual field testing results
If treatment is recommended, options may include:
- Medicated eye drops: These are most commonly prescribed and act to decrease IOP, either by reducing fluid production or enhancing drainage.
- Oral medications: In some cases, systemic medication may be used to lower IOP.
- Laser therapy: Procedures like laser trabeculoplasty can help improve the eye’s natural fluid drainage.
- Monitoring: For people with borderline high pressure and no other risk factors, regular monitoring and follow-up exams may be recommended before initiating medication.
It is important not to discontinue prescribed eye drops or medications without discussing with your eye care provider, as this can cause pressure levels to rise again and increase glaucoma risk.
Prevention and Long-Term Outlook
While ocular hypertension cannot always be prevented, especially if driven by genetics or unmodifiable factors, some steps can help minimize risk and support eye health:
- Attend regular comprehensive eye exams, particularly if you have known risk factors.
- Inform your eye doctor of any family history of glaucoma or past eye injuries.
- Manage systemic health conditions like diabetes and high blood pressure.
- Use corticosteroid medications only as prescribed and under medical supervision.
- Adopt an overall healthy lifestyle, including not smoking and maintaining a healthy weight.
The prognosis for ocular hypertension is generally good if detected early and monitored or treated according to medical advice. Most people do not develop vision loss if managed appropriately, but untreated cases with additional risk factors require special care.
When Should You See a Doctor?
Since ocular hypertension does not cause symptoms, regular eye exams are vital. Seek prompt medical attention if you experience:
- Sudden reduction in vision
- Eye pain, redness, or halos around lights
- Headaches or eye discomfort
These symptoms can indicate other acute eye conditions requiring urgent care.
Frequently Asked Questions (FAQs)
Q: Is ocular hypertension dangerous?
A: By itself, ocular hypertension does not harm vision. However, if left unchecked, it greatly increases your risk for developing glaucoma, which can cause permanent vision loss. Early diagnosis and appropriate management can prevent these complications.
Q: Can ocular hypertension be cured?
A: There is no cure, but it can be effectively managed. Medicated eye drops, laser procedures, or simply careful monitoring, depending on your risk factors, can keep eye pressure in a safe range and prevent optic nerve damage.
Q: Will I need to use eye drops forever?
A: Some people with ocular hypertension may need to use drops long-term, while others may only need regular monitoring. Your eye doctor will personalize your treatment based on IOP readings and any changes to your optic nerve or visual field over time.
Q: Does high blood pressure cause ocular hypertension?
A: High blood pressure may contribute to the risk, but ocular hypertension is specifically related to drainage issues in the eye or increased fluid production, not just systemic blood pressure. Managing overall health remains important for eye health.
Q: How often should I have my eyes checked?
A: Adults over 40 or those with risk factors for glaucoma should have a comprehensive eye exam every 1–2 years or as recommended by their eye care provider.
Summary
Ocular hypertension refers to elevated eye pressure with no signs of optic nerve damage or vision loss. While it does not cause symptoms, the condition increases the risk of developing glaucoma, which can lead to permanent vision impairment if not treated. Early detection, routine eye checks, and appropriate management are key to preserving vision and eye health over time.
References
- https://jamanetwork.com/journals/jamaophthalmology/fullarticle/270929
- https://www.medicalnewstoday.com/articles/ocular-hypertension
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4079553/
- https://www.healthline.com/health/eye-health/ocular-hypertension
- https://www.healthline.com/health/eye-health/eye-pressure-range
- https://www.brightfocus.org/resource/ocular-hypertension-and-glaucoma/
- https://www.health.harvard.edu/blog/who-needs-treatment-for-ocular-hypertension-202209202818
- https://www.healthlinejournal.org/index_pdf/419.pdf
Read full bio of medha deb












