Occipital Neuralgia: Symptoms, Diagnosis, Causes, and Treatments
A comprehensive guide to understanding, diagnosing, and treating occipital neuralgia—an often-misdiagnosed cause of head and neck pain.
Occipital Neuralgia
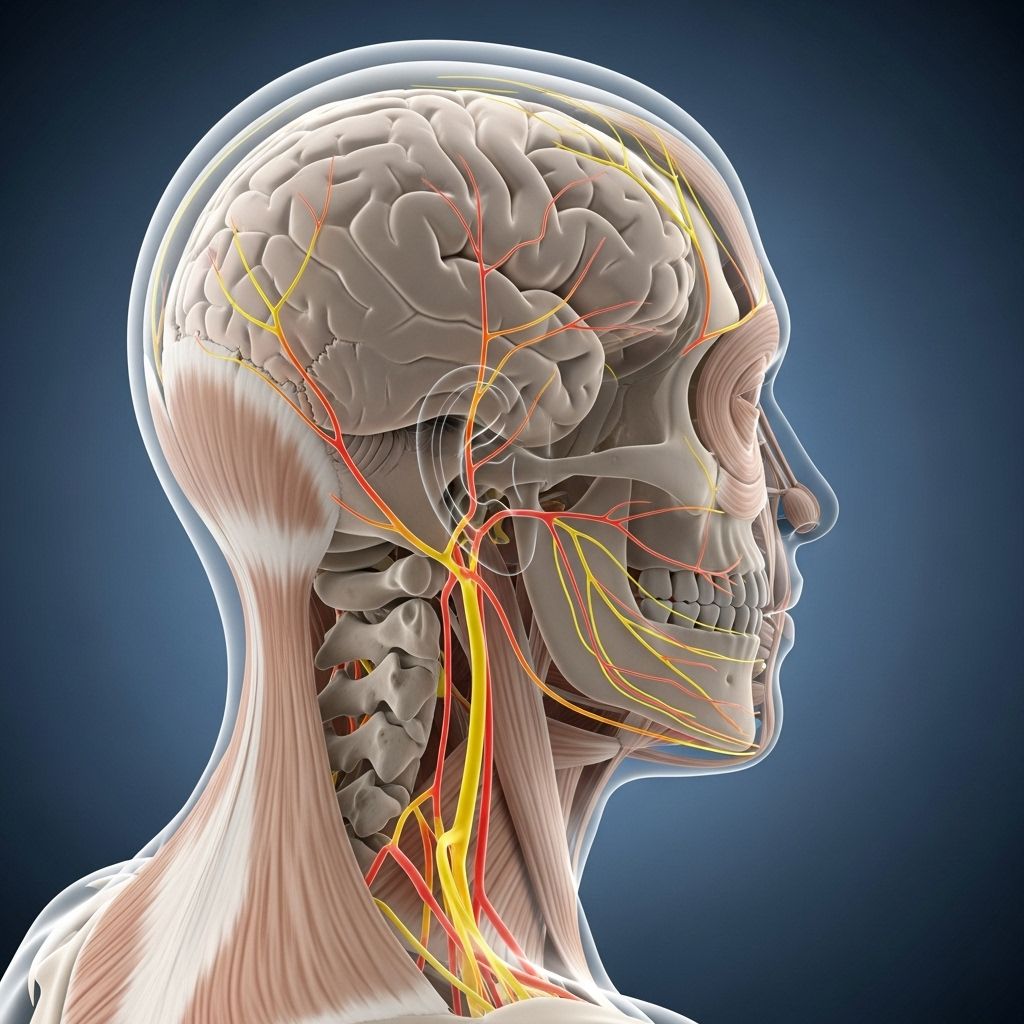
Occipital neuralgia is a distinct neurological condition characterized by sudden, severe pain originating at the base of the skull, radiating to the scalp, commonly mistaken for other types of headaches. This pain results from irritation or injury to the occipital nerves, which travel from the neck up through the scalp. While not life-threatening, occipital neuralgia can significantly affect quality of life if not accurately diagnosed and managed.
What is Occipital Neuralgia?
Occipital neuralgia is a chronic headache disorder caused by dysfunction or injury to the occipital nerves. These nerves—primarily the greater, lesser, and third occipital nerves—originate in the cervical spine (upper neck) and provide sensation to the posterior scalp. When these nerves are compressed, inflamed, or irritated, distinctive neuralgic pain develops.
- Commonly presents as sharp, shooting, or electric-shock-like pain in the upper neck, back of the head, or behind the ears.
- May be accompanied by burning, aching, throbbing pain, or a sensation of tightness in the scalp.
- Pain is often unilateral but can affect both sides.
Understanding the Occipital Nerves
The occipital nerves play a pivotal role in transmitting sensory information from the upper neck and scalp to the brain. There are three main occipital nerves:
- Greater occipital nerve: The largest, running up the back of the head to the scalp.
- Lesser occipital nerve: Travels along the side of the head, above the ear.
- Third occipital nerve: A smaller branch, innervating the lower scalp and upper neck.
Any irritation or entrapment of these nerves can lead to the symptoms of occipital neuralgia.
Symptoms of Occipital Neuralgia
Symptoms of occipital neuralgia often mimic those of migraines or tension headaches but have distinguishing features:
- Severe, shooting, or stabbing pain—usually starting at the base of the skull and radiating upward and outward over the scalp.
- Paroxysmal pain attacks that may last seconds to minutes but recur frequently.
- Sensitivity of the scalp, particularly over the course of the affected nerves. Even light touch, such as brushing the hair, can trigger pain.
- Pain on one or both sides of the head; sometimes the pain is bilateral.
- Occasional associated symptoms: pain behind the eyes, photophobia (light sensitivity), and aching or throbbing background pain between attacks.
Between pain attacks, some individuals may experience scalp tenderness, skin tingling (paresthesia), numbness, or a ‘pins and needles’ sensation in the affected area.
Causes of Occipital Neuralgia
The etiology of occipital neuralgia is diverse. Most cases involve irritation or compression of the occipital nerves. Possible mechanisms include:
- Muscle tightness or spasm in the neck, which may compress the nerves.
- Head, neck, or back injury (including whiplash injury).
- Cervical disc degeneration or arthritis, causing inflammation near the nerve roots.
- Tumors, cysts, or vascular abnormalities impinging on the nerves.
- Structural abnormalities such as bone overgrowth or thickened ligaments.
- Other conditions like diabetes, infections, or gout, which may predispose nerves to inflammation or injury.
- In many cases, no clear cause is identified, and the condition is termed idiopathic.
Risk Factors and Triggers
Though occipital neuralgia can affect anyone, certain factors increase susceptibility:
- Recent or historical neck trauma or strain.
- Poor posture (e.g., hunching over computers or mobile devices for prolonged periods).
- Chronic muscle tension or whiplash injury.
- Degenerative spinal diseases such as osteoarthritis.
- Previous head or neck surgery.
Triggers that may precipitate an episode of pain include:
- Sudden neck movement or prolonged awkward neck postures.
- Physical activity—especially activities involving repetitive head/neck motion.
- Touching or brushing the scalp or hair.
- Stress or muscle fatigue.
Diagnosis of Occipital Neuralgia
Diagnosis can be challenging, as symptoms often overlap with those of other headache disorders. The process typically involves:
- Detailed medical history—especially focusing on headache characteristics, distribution, and triggers.
- Physical examination—particularly identifying tenderness over the occipital nerves or aggravation of pain by neck movements.
- Neurological evaluation to rule out other causes of head/neck pain.
- Occipital nerve block—injection of anesthetic near the affected nerve. Relief of pain after the block supports the diagnosis.
Imaging (MRI or CT of the head and neck) may be recommended to exclude structural problems (like tumors, vascular abnormalities, or disk degeneration) if an underlying cause is suspected, or if symptoms are atypical.
Treatment Options for Occipital Neuralgia
The primary goal of treatment for occipital neuralgia is pain relief and resolution of the underlying cause, if identifiable. The treatment protocol is typically guided by symptom severity, patient preferences, and the response to initial therapies. Treatment options can be grouped into conservative, interventional, and surgical approaches.
Conservative (Non-Surgical) Therapies
- Medications:
- Non-steroidal anti-inflammatory drugs (NSAIDs): Over-the-counter options like ibuprofen or naproxen help reduce inflammation and pain.
- Muscle relaxants: May help ease neck muscle tension.
- Antidepressants (tricyclic, especially amitriptyline): Used for their nerve-pain modulating properties, not for mood disorders.
- Anti-seizure medications: Drugs such as gabapentin or carbamazepine target neuropathic pain.
- Home care and adjunct therapies:
- Applying heat to the neck and scalp helps relax tense muscles and relieve pain.
- Massage therapy reduces muscle tightness that may be compressing the occipital nerves.
- Physical therapy involves neck-strengthening and stretching exercises, improving posture and decreasing nerve irritation.
- Rest in a quiet, dark room during acute pain episodes.
Interventional Therapies
- Occipital Nerve Block: A key diagnostic and therapeutic step, where a local anesthetic (sometimes combined with a steroid) is injected around the occipital nerves. Relief can be rapid but may be temporary. Repeat injections may be required.
- Botox Injections (Botulinum toxin): Offer relief for some individuals, especially if other medications are ineffective.
- Other techniques: Pulsed radiofrequency ablation or cryotherapy may be considered in resistant cases, working by disrupting nerve conduction.
Surgical and Advanced Treatments
- Occipital Nerve Stimulation: Implantation of a device delivers electrical impulses to the occipital nerves, interrupting pain signals for chronic or intractable sufferers.
- Microvascular Decompression: Involves adjusting or moving blood vessels that may be compressing the affected nerves.
- Occipital Release Surgery: Surgical decompression by releasing the nerve from the surrounding soft tissues.
- Spinal Cord Stimulation: Electrodes are placed near the spinal cord to modulate pain transmission from the head and neck.
- Ganglionectomy: Surgical removal of nerve clusters at the upper spine level in rare, refractory cases.
Surgery is considered only after all other therapeutic options have been exhausted and is generally rare.
Living with Occipital Neuralgia
Though the pain caused by occipital neuralgia can be severe, the condition is not life threatening. Most patients recover with a combination of medical treatment, lifestyle changes, and physical therapy. For chronic or recurrent cases, working with a multidisciplinary team—including neurologists, pain specialists, and physical therapists—helps optimize pain management.
- Maintaining good posture and ergonomics at work and at home reduces muscle tension in the neck.
- Regular stretches and strengthening exercises for neck and upper back muscles promote long-term relief.
- Stress reduction techniques, including mindfulness, yoga, or biofeedback, can help decrease pain flare-ups.
When to See a Doctor
If you have severe, persistent, or recurring head and neck pain—especially if you experience sharp, electric shock-like pain that does not respond to standard headache remedies—it is important to seek evaluation by a healthcare provider. Prompt diagnosis helps rule out other potentially serious conditions and initiates appropriate treatment.
Frequently Asked Questions (FAQs)
Q: What conditions can mimic occipital neuralgia?
A: Occipital neuralgia is often confused with migraines, cluster headaches, or tension-type headaches because many symptoms overlap. A distinctive feature of occipital neuralgia is the sharp, shooting pain starting at the neck base, often triggered by pressing on the occipital nerve area.
Q: How is occipital neuralgia diagnosed?
A: Diagnosis largely relies on a careful review of symptoms and physical examination. Relief of pain after an occipital nerve block confirms the diagnosis. Imaging may be ordered to exclude tumors, vascular anomalies, or spine disease in atypical cases.
Q: Will occipital neuralgia go away on its own?
A: For some, symptoms may resolve with conservative care like rest, heat, and muscle relaxation. However, untreated cases may persist or recur, requiring medical interventions for lasting relief.
Q: Are there any complications of occipital neuralgia?
A: Occipital neuralgia is not dangerous or fatal, but chronic pain can impact sleep, mood, and work. Rarely, if caused by another disorder (like a tumor or aneurysm), serious complications could arise if the underlying cause is not addressed.
Q: Can lifestyle changes help prevent recurrences?
A: Yes. Preventing neck strain, maintaining good posture, using ergonomic workstations, keeping muscles flexible and strong, and minimizing stress can reduce recurrences.
Summary Table: Overview of Occipital Neuralgia
| Aspect | Details |
|---|---|
| Definition | Nerve pain from irritation or compression of occipital nerves causing head/neck pain |
| Symptoms | Shooting/stabbing pain from base of skull up scalp, scalp tenderness, episodic attacks |
| Causes | Trauma, arthritis, muscle spasm, nerve compression, sometimes unknown |
| Diagnosis | Clinical history, nerve block, physical exam, imaging (if needed) |
| Treatments | Medications, nerve block, physical therapy, surgery for refractory cases |
| Prognosis | Usually good with treatment; chronic cases may need ongoing care |
Key Takeaways
- Occipital neuralgia is the result of irritation or injury to occipital nerves, and presents uniquely compared to migraines or tension headaches.
- It is treatable, often without surgery, using medications, nerve blocks, physical therapy, and lifestyle changes.
- Diagnosis is confirmed by nerve block and clinical evaluation; imaging may be required for complex cases.
- Most individuals recover or successfully manage symptoms with a combination of treatments.
References
- https://www.uchealth.com/en/conditions/occipital-neuralgia
- https://www.medicalnewstoday.com/articles/320143
- https://blog.ochsner.org/articles/how-to-treat-occipital-neuralgia-a-common-and-underdiagnosed-headache/
- https://www.webmd.com/migraines-headaches/occipital-neuralgia-symptoms-causes-treatments
- https://my.clevelandclinic.org/health/diseases/23072-occipital-neuralgia
- https://www.health.harvard.edu/pain/occipital-neuralgia-symptoms-and-treatments
- https://www.aans.org/patients/conditions-treatments/occipital-neuralgia/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4810328/
- https://www.baltimoreperipheralnervepain.com/video/occipital-neuralgia-relief-with-peripheral-nerve-surgery.cfm
Read full bio of Sneha Tete












