Normal Retina vs. Diabetic Retinopathy: A Comprehensive Guide to Diabetes-Related Eye Health
Understanding the visual differences, risk factors, symptoms, and treatments for diabetic retinopathy and protecting vision in diabetes.
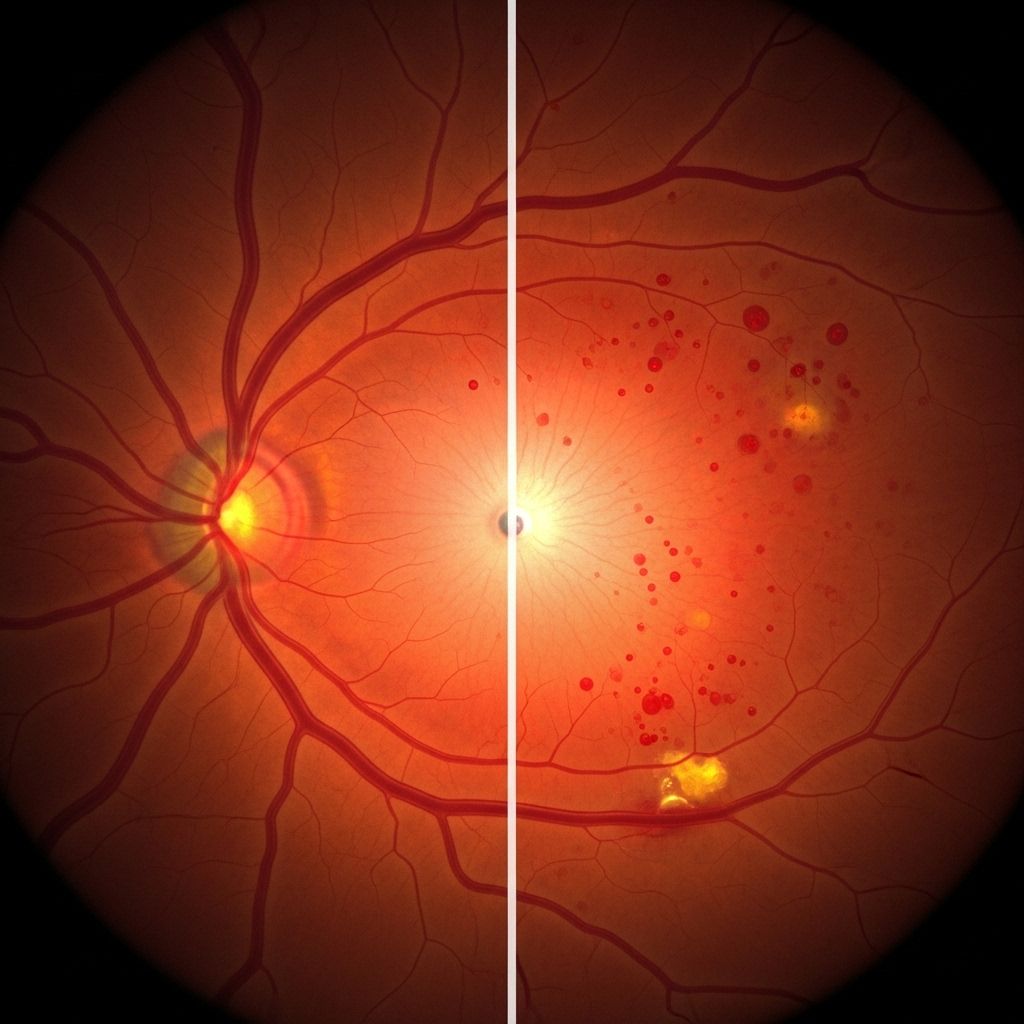
Normal Retina vs. Diabetic Retinopathy: A Comprehensive Guide
The retina is a crucial component of eye health, transforming incoming light into nerve signals that form our vision. Diabetes, however, poses significant risks to this delicate tissue—most notably through diabetic retinopathy, a leading cause of blindness in adults. Understanding how diabetic retinopathy develops, its impact on vision, preventive strategies, and treatment options is essential for anyone with diabetes or concerned about eye health.
What Is the Retina?
The retina is a thin layer of tissue lining the back of the eye. It contains photoreceptor cells that detect light, converting it into electrical signals sent to the brain via the optic nerve for image processing. A healthy retina ensures clear, sharp vision and effective color perception.
- Location: Lines the inner back surface of the eye.
- Function: Detects light and transmits visual information to the brain.
- Key Structures: Contains blood vessels, photoreceptors (rods & cones), and nerve fibers.
Diabetes and Its Effects on the Retina
Diabetes affects the body’s ability to regulate blood sugar. Over time, persistently high blood glucose damages blood vessels throughout the body, including those nourishing the retina. This damage can lead to diabetic retinopathy, the most common cause of vision loss in people with diabetes.
- Retinal Blood Vessel Damage: Elevated sugar weakens and damages small retinal vessels.
- Progressive Changes: Blocked vessels, leaking fluid, and abnormal new vessel growth can occur.
- Complications: Scarring, loss of retinal function, and potential blindness.
What Is Diabetic Retinopathy?
Diabetic retinopathy is a specific eye condition caused by diabetes-related damage to the blood vessels in the retina. It can affect both Type 1 and Type 2 diabetes patients. Early stages may not show symptoms, but as the condition worsens, vision can deteriorate.
| Feature | Normal Retina | Diabetic Retinopathy |
|---|---|---|
| Blood Vessels | Healthy, intact, no leakage | Damaged; may leak blood/fluid and develop abnormal new vessels |
| Vision | Clear and sharp | Blurred, loss of central or peripheral vision |
| Symptoms | None | Floaters, dark spots, decreased visual acuity, trouble seeing colors |
| Risk Factors | None (in context of diabetes) | Long duration of diabetes, poor glucose control, high blood pressure |
How Diabetic Retinopathy Develops
Diabetic retinopathy progresses through distinct stages, with increasing severity as more retinal blood vessels are affected:
- Mild Nonproliferative Retinopathy: Microaneurysms (tiny bulges in retinal vessels) begin to appear.
- Moderate Nonproliferative Retinopathy: Blood vessels may swell and distort, impeding blood flow.
- Severe Nonproliferative Retinopathy: Many vessels are blocked, depriving the retina of necessary nutrients; the retina signals for new vessel growth.
- Proliferative Diabetic Retinopathy: The most advanced stage. Fragile new blood vessels grow on the retina and the gel-like vitreous, prone to leaking and bleeding. Scar tissue can lead to retinal detachment and severe vision loss.
Symptoms of Diabetic Retinopathy
Early diabetic retinopathy often presents no symptoms. As the condition progresses, individuals might experience:
- Floaters or dark spots in vision
- Difficulty seeing at night (night blindness)
- Blurry or fluctuating vision
- Trouble distinguishing colors
- Sudden or gradual loss of vision
Symptoms generally affect both eyes, but may vary in severity.
Key Risk Factors
Several risk factors increase the likelihood of developing diabetic retinopathy:
- Duration of diabetes (the longer you have it, the greater the risk)
- Poor blood sugar (glucose) control
- High blood pressure (hypertension)
- High cholesterol levels
- Smoking
- Pregnancy (retinopathy can worsen rapidly)
Impact of Diabetic Retinopathy on Vision
Diabetic retinopathy can cause several significant complications which may result in permanent vision loss:
- Macular Edema: Fluid leaks into the macula—the part of the retina responsible for sharp central vision—causing swelling and blurred vision.
- Retinal Detachment: Scar tissue from abnormal vessel growth pulls the retina away from the back of the eye.
- Neovascular Glaucoma: New blood vessels may grow on the iris and block normal fluid drainage, increasing eye pressure and risking optic nerve damage.
Other Diabetes-Related Eye Conditions
Alongside diabetic retinopathy, diabetes increases risk for other eye diseases:
- Cataracts: Diabetics are 2 to 5 times more likely to develop cataracts—clouding of the eye’s lens, often at a younger age.
- Open-angle Glaucoma: Diabetes nearly doubles the risk of glaucoma, which can lead to optic nerve damage and blindness.
Diagnosis: Detecting Diabetic Retinopathy
Timely diagnosis is crucial. Diabetic retinopathy can be detected before symptoms arise using specialized eye exams:
- Comprehensive Dilated Eye Exam: Eye drops are used to widen (dilate) the pupils, allowing the doctor to examine the retina and identify early changes.
- Photographic Retinal Imaging: Detailed images help monitor the disease’s progression and guide treatment.
- Optical Coherence Tomography (OCT): Provides cross-sectional images to assess retinal swelling.
Prevention Strategies
Preventing or delaying diabetic retinopathy begins with diabetes management:
- Maintain consistent blood glucose levels through diet, medication, or insulin therapy.
- Regularly monitor blood pressure and cholesterol—keep within healthy ranges.
- Lead a healthy lifestyle: exercise, avoid smoking, manage stress.
- Schedule annual comprehensive eye exams.
- If pregnant, consult with your eye care professional for additional screening.
Treatment Options for Diabetic Retinopathy
While diabetic retinopathy cannot be fully cured, advances in treatment can halt or slow progression and often preserve vision:
- Laser Treatment (Photocoagulation): Seals leaking vessels and prevents new vessel growth.
- Anti-VEGF Injections: Medications injected into the eye to reduce swelling and inhibit abnormal blood vessel formation.
- Vitrectomy: Surgical removal of blood or scar tissue from the vitreous gel to restore vision.
- Steroid Injections: Reduce retinal inflammation.
Prompt initiation of these treatments following detection can significantly limit vision loss and maintain quality of life.
Living with Diabetic Retinopathy
- Stay up to date with diabetes management to prevent progression.
- Educate yourself regarding treatment advances—consult with your healthcare provider about new options.
- Commit to regular eye checkups, especially if you notice symptoms such as floaters, blurriness, or unexplained vision changes.
Frequently Asked Questions (FAQ)
What is the difference between a normal retina and a retina affected by diabetic retinopathy?
A normal retina has healthy blood vessels with no leakage, swelling, or abnormal growth, enabling clear vision. Diabetic retinopathy damages these vessels, causing leaks, hemorrhages, and the growth of fragile, irregular new vessels—leading to vision problems and potentially blindness.
Are there early warning signs of diabetic retinopathy?
There are typically no symptoms in early stages. Regular dilated eye exams detect changes before noticeable vision loss.
How is diabetic retinopathy treated?
Treatments include laser therapy, anti-VEGF eye injections, surgical vitrectomy, and medication for swelling. Effective blood sugar, blood pressure, and cholesterol control are also essential.
Can diabetic retinopathy be cured?
No. The condition can be managed but not reversed once advanced. Early intervention preserves remaining vision.
If I have diabetes, how often should I get my eyes checked?
At least once a year, or more frequently if you have existing retinopathy or other eye symptoms.
Key Takeaways for Diabetes and Eye Health
- Diabetic retinopathy is preventable and treatable if caught early.
- Control diabetes: Managing blood sugar, pressure, and cholesterol dramatically lowers risk.
- Annual eye exams are vital for early detection—even before symptoms appear.
- Advanced treatments can help preserve vision in those affected.
- Educate yourself and consult with healthcare professionals for personalized care plans.
References & Resources
- National Eye Institute: Diabetic Retinopathy Overview
- MedlinePlus: Diabetes and Eye Disease
- Cleveland Clinic: Diabetes-Related Retinopathy Treatments
- Healthline: Diabetic Retinopathy Symptoms and Diagnosis
References
- https://medlineplus.gov/ency/article/001212.htm
- https://www.healthline.com/health/type-2-diabetes/retinopathy
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://www.healthline.com/health/eye-health/diabetic-retinopathy-oct
- https://www.healthline.com/health/video/type-2-diabetes
- https://www.healthline.com/health/video/diabetes-nutrition-101
- https://my.clevelandclinic.org/health/diseases/7104-diabetes
- https://www.medicalnewstoday.com/articles/323729
Read full bio of Sneha Tete












