Understanding Noncompaction Cardiomyopathy: Symptoms, Diagnosis, and Management
Get a comprehensive overview of noncompaction cardiomyopathy, including causes, symptoms, diagnosis methods, treatment options, and long-term outlook.
Understanding Noncompaction Cardiomyopathy (LVNC)
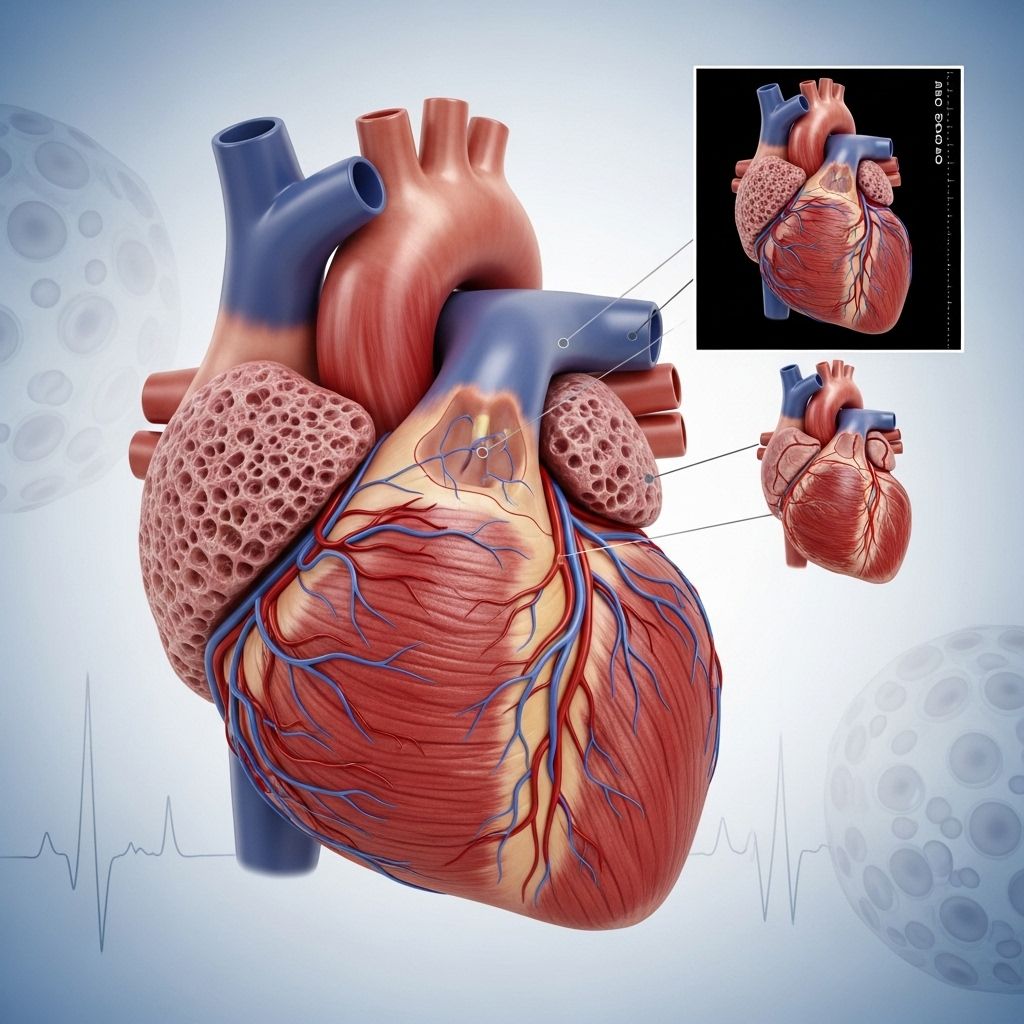
Noncompaction cardiomyopathy, often referred to as left ventricular noncompaction cardiomyopathy (LVNC), is a structural abnormality of the heart muscle that develops before birth. Although rare, it is being recognized more often due to improvements in heart imaging technologies. This disorder can affect how well the heart pumps blood and may lead to various symptoms and complications later in life.
What is Noncompaction Cardiomyopathy?
Noncompaction cardiomyopathy is a disorder primarily affecting the left ventricle—the main pumping chamber of the heart. In LVNC, the heart muscle does not develop its typical solid, compact structure. Instead, it forms with deep grooves and a spongy appearance, resulting in areas known as noncompacted myocardium. This abnormal muscle structure can impair the heart’s ability to pump blood effectively and may disrupt its electrical conduction system.
- Genetic Disorder: LVNC is often genetic and can run in families.
- Developmental Issue: The failure of the heart muscle to properly compact occurs in the womb, sometimes due to specific genetic mutations.
- Variable Expression: Symptoms and effects can range from severe in infancy to subtle or absent in adulthood.
Causes and Risk Factors
The primary cause of noncompaction cardiomyopathy is believed to be genetic, involving mutations that affect how the heart muscle develops during embryonic life.
- Genetic Mutations: Variations in genes involved in heart muscle development.
- Family History: Having a relative with cardiomyopathy increases risk.
- Other Conditions: Sometimes associated with other congenital heart conditions or neuromuscular disorders.
In some cases, noncompaction may be discovered incidentally during family screening or routine evaluations for athletes, as improved imaging tools reveal previously undiagnosed cases.
Symptoms of Noncompaction Cardiomyopathy
Symptoms of LVNC depend on the severity and location of noncompacted muscle and may appear at any age.
- Shortness of breath during exertion or even at rest
- Fatigue
- Dizziness or lightheadedness
- Fainting (syncope)
- Palpitations or noticeable irregular heartbeats (arrhythmias)
- Chest pain
- Swelling of ankles and feet (edema)
- Blood clots or risk of stroke
It is important to note that some individuals with LVNC may never develop symptoms, while others may begin showing signs in infancy or early childhood.
Potential Complications
Noncompaction cardiomyopathy can increase the risk of several heart-related complications:
- Heart Failure: Reduced heart muscle function can progress to chronic heart failure.
- Arrhythmias: Abnormal electrical conduction can cause dangerous heart rhythm disturbances.
- Blood Clots: Stagnation of blood can lead to clot formation, increasing stroke risk.
How is Noncompaction Cardiomyopathy Diagnosed?
Early and accurate diagnosis of LVNC is critical. The process usually starts with a thorough review of symptoms, family medical history, and a physical examination. If noncompaction is suspected, referral to a cardiologist is advised.
Diagnostic Tests
- Electrocardiogram (EKG): Records electrical activity and helps detect arrhythmias.
- Echocardiogram (Echo): Uses ultrasound to assess heart structure and pumping ability, revealing the typical spongy appearance of noncompacted muscle.
- Cardiac CT or MRI: Provides detailed images of the heart’s anatomy and structure, confirming the diagnosis.
In some cases, doctors may refer patients or their families to a geneticist for further evaluation and potential genetic counseling.
Family and Athlete Screening
Sometimes, asymptomatic individuals are diagnosed during family screenings or organized athlete evaluations, owing to increased awareness and advanced imaging methods.
Treatment Options for Noncompaction Cardiomyopathy
Although there is no cure for LVNC, effective management focuses on treating symptoms, preventing complications, and supporting heart function. Treatment plans are individualized and overseen by a cardiologist experienced in heart muscle disorders.
Common Treatments
- Medications:
- Manage blood pressure
- Regulate heart rhythm
- Improve heart pumping strength
- Prevent blood clots
- Reduce fluid buildup (diuretics)
- Implanted Devices: Such as pacemakers or implantable cardioverter-defibrillators (ICDs), to manage arrhythmias and reduce sudden death risk.
- Cardiac Assist Devices: Mechanical ventricular assist devices (VADs) may support heart pumping in severe cases.
- Heart Transplant: Reserved for those with end-stage heart failure and no other treatment options.
Living with Noncompaction Cardiomyopathy
People diagnosed with LVNC require regular checkups with a cardiologist, even if they do not have symptoms. Monitoring helps detect changes early and tailor treatment as needed. Some individuals never experience serious health issues, while others may require substantial medical support throughout their lives.
Prognosis and Outlook
The outlook for noncompaction cardiomyopathy varies significantly from person to person. It depends on factors such as the degree and location of noncompacted muscle, overall heart function, and any associated health conditions.
| Prognostic Factor | Impact on Outlook |
|---|---|
| Extent of Noncompaction | Widespread or mid/basal involvement is linked to higher risks than isolated apical noncompaction. |
| Heart Function (Ejection Fraction) | Lower ejection fraction is associated with a greater risk of heart failure and adverse outcomes. |
| Symptom Status | Asymptomatic patients may have a better prognosis, though monitoring is essential. |
| Age at Diagnosis | Infants/children diagnosed early may have a greater risk for severe outcomes or need for transplant. |
A 2021 study showed that adults with good cardiac function and noncompaction limited to the apex had similar life expectancy to the general population. However, people diagnosed in childhood or those with more extensive involvement may face higher risks in the first decade following diagnosis. Close follow-up can help detect complications early and improve long-term health.
Frequently Asked Questions (FAQ)
What is left ventricular noncompaction cardiomyopathy (LVNC)?
LVNC is a rare structural abnormality of the heart muscle, most commonly affecting the lower left chamber. Affected heart muscle has a spongy texture instead of a smooth and solid one, impairing blood pumping and sometimes heart rhythm.
Is LVNC inherited?
Many cases of LVNC are inherited due to genetic mutations that interfere with normal heart muscle development during fetal growth. Family history of cardiomyopathy or sudden cardiac death may indicate genetic risk. Genetic counseling and screening are recommended for families of affected individuals.
Can someone have LVNC and never have symptoms?
Yes, some people with LVNC remain asymptomatic, while others develop significant symptoms or complications. Regular monitoring is important for all diagnosed individuals, regardless of current symptoms.
What makes LVNC different from other cardiomyopathies?
Unlike other forms of cardiomyopathy, LVNC is defined by the unique structural appearance of the heart muscle and is thought to arise from abnormal development in utero. Some researchers debate whether it is a distinct disorder or a pattern of heart remodeling seen in other conditions.
How often should individuals with LVNC see a doctor?
Regular checkups with a cardiologist are essential—typically at least annually, or more often if symptoms or complications arise. Cardiac imaging and possibly rhythm monitoring will be used for ongoing assessment.
When to See a Doctor
If you have a family history of cardiomyopathy, sudden unexplained death, or experience symptoms such as unexplained fainting, palpitations, or severe shortness of breath, it is important to see a doctor for evaluation. Early diagnosis allows for better management and improved outcomes.
Key Takeaways
- LVNC is a developmental heart muscle disorder, typically genetic in origin.
- It can present as early as infancy or remain silent into adulthood.
- Symptoms may include heart failure, arrhythmias, and risk of stroke, but many people live normal, healthy lives.
- Diagnosis relies on imaging, family history, and sometimes genetic testing.
- Treatment is tailored to symptom management, arrhythmia prevention, and heart failure support.
Resources and Support
If you or a family member has been diagnosed with noncompaction cardiomyopathy, seek expert care from a cardiologist experienced in the condition. Genetic counseling may help families understand their risk and screening needs. Support groups and patient advocacy organizations can also provide information and community.
References
- Content synthesized and rephrased from authoritative sources including Healthline and MedlinePlus Genetics.
References
- https://www.healthline.com/health/heart-disease/noncompaction-cardiomyopathy
- https://www.ahajournals.org/doi/10.1161/JAHA.119.015563
- https://medlineplus.gov/genetics/condition/left-ventricular-noncompaction/
- https://www.healthline.com/health/heart-disease/cardiomyopathy
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8226207/
- https://www.ncbi.nlm.nih.gov/books/NBK537025/
- https://www.ahajournals.org/doi/10.1161/JAHA.120.018815
- https://academic.oup.com/eurheartj/article/32/12/1446/501502
Read full bio of Sneha Tete












