Non-Small Cell Lung Cancer and Pleural Effusion: Understanding, Diagnosis, and Treatment
Explore the link between non-small cell lung cancer and pleural effusion, from symptoms to treatment and prognosis.
Non-Small Cell Lung Cancer and Pleural Effusion
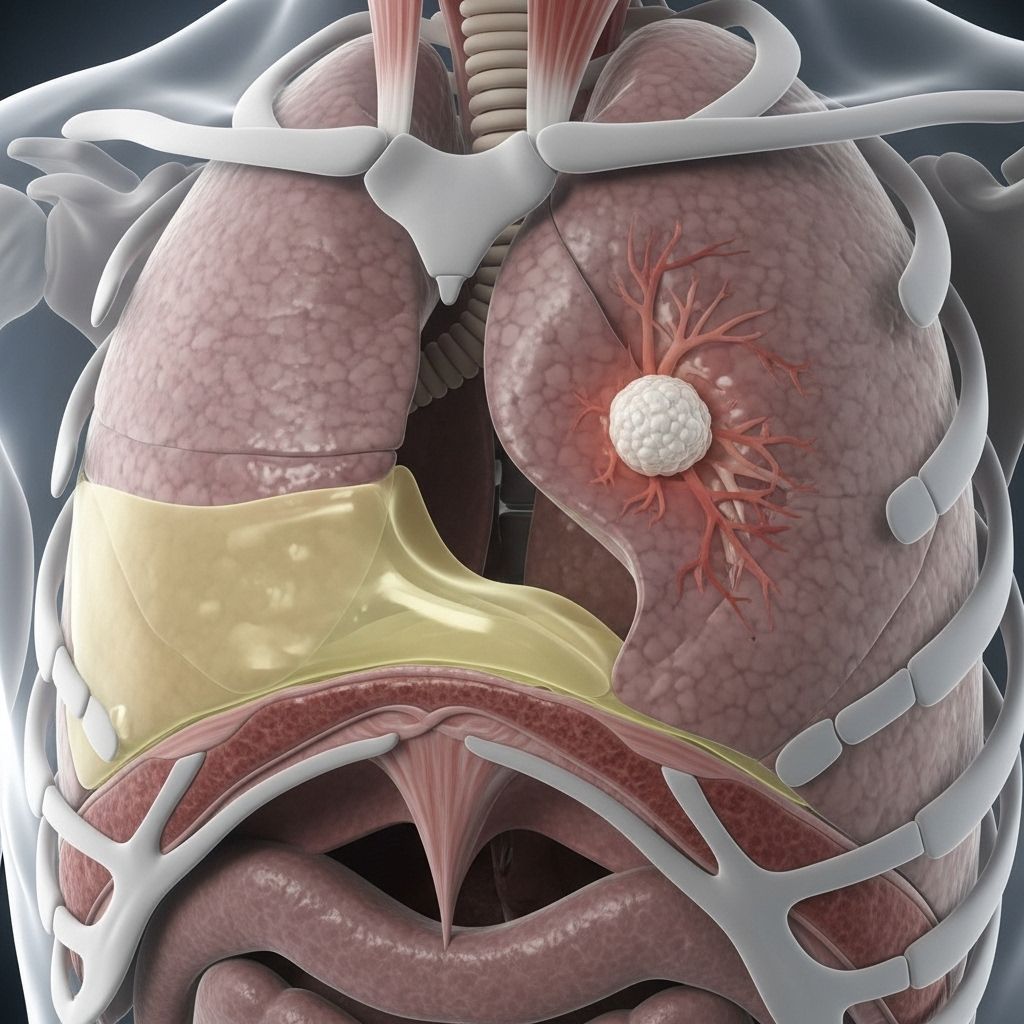
Non-small cell lung cancer (NSCLC) is the most common form of lung cancer, accounting for approximately 80–85% of all lung cancer cases. One significant complication associated with NSCLC is pleural effusion, a condition marked by a buildup of fluid around the lungs. This article explains the link between NSCLC and pleural effusion, details of diagnosis and treatment, important recent research, and what this means for patient outcomes.
What Is Pleural Effusion?
Pleural effusion refers to the abnormal accumulation of fluid in the pleural space—the thin cavity between the lungs and the chest wall, lined by a double-layered membrane called the pleura. While the pleura normally contains a small amount of fluid to cushion and lubricate the lungs during respiration, an excess can cause significant health problems.
- Pleura: Membranes surrounding the lungs and lining the chest cavity.
- Pleural fluid: A lubricating liquid found in the pleural space.
- Pleural effusion: Excess fluid buildup that may lead to symptoms and complications.
- “Water on the lungs” is a common term for pleural effusion.
Symptoms of Pleural Effusion
- Shortness of breath
- Pain during breathing or coughing
- Fever
- Dry or productive cough
- Sensation of chest heaviness or tightness
Severity and specific symptoms can vary based on the amount of fluid, the underlying cause, and whether both lungs are affected.
What Causes Pleural Effusion in NSCLC?
Pleural effusion in the context of NSCLC is often the result of cancer spreading to the pleural membranes, impairing their ability to regulate fluid. The condition can also be triggered by other factors, such as infections, heart problems, or direct injury to the chest. However, when pleural effusion is associated with cancer, it is often termed malignant pleural effusion (MPE), and it signifies a more advanced stage of disease.
Malignant Pleural Effusion and Its Implications
A malignant pleural effusion (MPE) occurs when cancer cells invade the pleural space, causing persistent and often rapid accumulation of fluid. In people with NSCLC, the presence of MPE often indicates that cancer has advanced into the surrounding tissues, placing the disease into a more serious stage—commonly stage M1a.
| Characteristic | MPE in NSCLC |
|---|---|
| Clinical significance | Indicator of cancer spread and advanced disease |
| Outlook | Generally poorer prognosis |
| Common symptoms | Dyspnea, chest pain, cough, fever |
| Proportion in lung cancer | Occurs frequently, especially in advanced cases |
Multiple studies show that MPE is associated with decreased survival odds. However, medical advances are changing how doctors approach treatment and the course of the disease.
Diagnosis: Identifying Pleural Effusion in NSCLC
Early diagnosis is crucial to ensure patients receive appropriate, timely treatment. When NSCLC patients present with symptoms indicative of pleural effusion, doctors likely initiate several diagnostic steps:
- Medical history and physical exam: Assess for shortness of breath, diminished breath sounds, and other signs.
- Imaging Studies: Most commonly, a chest X-ray can detect fluid in the lungs, while a computed tomography (CT) scan provides greater detail about effusion size and location.
- Thoracentesis: A procedure in which a needle is inserted into the pleural space to withdraw a fluid sample for analysis. Thoracentesis is essential both for diagnosis and symptom relief.
- Laboratory analysis of pleural fluid: Physicians check for cancer cells, infection, or markers of inflammation.
- Other tests: In some cases, ultrasound or additional imaging may help further characterize effusions and guide procedures.
Physical Exam Findings
- Dullness to percussion over affected lung area
- Reduced or absent breath sounds
- Reduced chest wall movement on the affected side
- Pleural friction rub, especially with large effusions
Radiological Features
- Costophrenic angle blunting on X-ray, often observed with 200–300 ml of fluid
- Larger effusions (500–2000 ml) are not uncommon
- In massive effusion, displacement of the mediastinum can be noted
- Bilateral effusions may occur, especially if there is no sign of heart enlargement
How Does Pleural Effusion Affect NSCLC Treatment?
Pleural effusion in NSCLC has historically been considered a sign of late-stage disease, often placing patients in a category where curative treatment is not possible. In the past, treatment was largely supportive and palliative. Recent research, however, suggests that some carefully selected patients may benefit from aggressive treatment, including surgery, if disease remains confined to the chest.
- Aggressive treatment: Studies published in 2019 and 2020 show improved survival in patients with NSCLC and pleural effusion, especially if cancer has not spread outside the chest (minimal disease).
- Multimodal therapy: May involve systemic therapy (like chemotherapy), local fluid control, and in selected cases, surgery.
- Patient selection: Candidates for aggressive treatments are typically those with good physical function and limited cancer spread.
Main Treatment Options for Pleural Effusion in NSCLC
- Thoracentesis: Both diagnostic and symptomatic, used to withdraw pleural fluid and provide relief.
- Tube thoracostomy: Placement of a chest tube to allow ongoing drainage, typically used for larger or persistent effusions.
- Indwelling pleural catheter: Catheters inserted for repeated or continuous drainage, suitable for patients with recurring effusions.
- Pleurodesis: A chemical agent is introduced into the pleural space to cause the pleural layers to adhere, preventing future fluid accumulation.
- Shunt placement: Surgical insertion of a tube to route fluid to another part of the body.
- Chemotherapy: Effective for managing both the primary cancer and secondary effusion in certain cases.
Role of Surgery
Historically, patients with pleural effusion were not considered surgical candidates. Yet, emerging studies indicate that after initial systemic therapy, surgery may benefit certain patients whose disease is strictly confined to the chest. In select cases, procedures such as lobectomy or pneumonectomy, sometimes combined with mediastinal dissection and after systemic therapy, have yielded improved survival rates.
| Treatment Approach | Details |
|---|---|
| Thoracentesis | Drains excess fluid, used for both symptom relief and diagnosis |
| Tube Thoracostomy | Chest tube insertion for continuous fluid drainage |
| Pleural Catheter | Indwelling device for outpatient management of recurrent effusion |
| Pleurodesis | Chemical procedure to adhere pleural layers, preventing fluid buildup |
| Chemotherapy | Systemic therapy targeting both cancer and effusion |
| Surgery (in select cases) | Lobectomy, pneumonectomy, with or without mediastinal dissection after response to initial therapy |
Outlook for Patients with NSCLC and Pleural Effusion
The development of pleural effusion, particularly malignant pleural effusion, is widely regarded as a marker of advanced or metastatic disease. This has traditionally meant a worse prognosis for patients. Median survival for those with malignant pleural effusion can range from three to 12 months, with the lowest survival seen in lung cancer patients.
However, new research has challenged these expectations. With aggressive and multidisciplinary treatment, some patients—especially those with minimal disease beyond the lungs and good performance status—can experience better outcomes and prolonged survival compared to earlier predictions.
- Aggressive Treatment Results: Studies found that surgery, after systemic therapy, resulted in higher 5-year survival rates for carefully chosen patients.
- Personalized Care: The specific prognosis and treatment options depend heavily on individual circumstances, the exact spread and nature of the cancer, and the patient’s general health.
- Further Research Needed: While promising, aggressive approaches are suitable for only a small subset of patients, and ongoing studies seek to refine the best methods for care.
Frequently Asked Questions About NSCLC and Pleural Effusion
Q: What is the main difference between pleural effusion and malignant pleural effusion?
A: Pleural effusion is simply the buildup of fluid around the lungs from any cause, such as infection or heart failure. Malignant pleural effusion means the fluid build-up is due to cancer cells spreading into the pleural space, most often indicating advanced disease.
Q: Is pleural effusion always a late-stage sign in NSCLC?
A: Most often, especially when malignant cells are present, pleural effusion in NSCLC is an indication of late-stage (stage IV/M1a) cancer. However, if the cancer hasn’t spread beyond the chest, new therapies—including surgery in select cases—may extend survival.
Q: How is pleural effusion managed in people who are not surgical candidates?
A: Symptom relief through pleural fluid drainage (via thoracentesis or catheter), and disease control with chemotherapy or targeted therapy are the primary modalities for patients who aren’t candidates for curative surgery.
Q: Can pleural effusion come back after treatment?
A: Yes, pleural effusion often recurs, especially in cancer. Indwelling pleural catheters or pleurodesis can be used as longer-term solutions to prevent repetitive fluid accumulation.
Q: Should all patients with NSCLC and pleural effusion undergo aggressive treatment?
A: No. The choice depends on the extent of disease, patient health, performance status, and individual preferences. Aggressive treatments are considered for highly selected patients with minimal extra-thoracic spread and good general condition.
Key Takeaways
- Pleural effusion is a common complication in people with non-small cell lung cancer and may signal advanced disease.
- Symptoms include shortness of breath, chest pain, cough, and fever.
- Diagnosis relies on a combination of clinical evaluation, imaging, and analysis of pleural fluid.
- Mainstays of treatment include fluid drainage, catheters, and in select patients, surgery and aggressive combination therapies.
- Recent studies suggest that some people with limited disease may have improved outlook with more aggressive management, but individualized care is crucial.
If you or a loved one is facing NSCLC with pleural effusion, consult an oncology team to discuss personalized options based on the latest research and your unique health situation.
References
- https://www.healthline.com/health/lung-cancer/non-small-cell-lung-cancer-pleural-effusion
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6409261/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4261269/
- https://my.clevelandclinic.org/health/diseases/17373-pleural-effusion
- https://www.cancerresearchuk.org/about-cancer/coping/physically/breathing-problems/fluid-on-lungs-pleural-effusion
- https://cancer.ca/en/treatments/side-effects/fluid-buildup-on-the-lung-pleural-effusion
- https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq
- https://www.rwjbh.org/treatment-care/cancer/types-of-cancer/lung-thoracic-cancer/pleural-cancer/
- https://www.macmillan.org.uk/cancer-information-and-support/impacts-of-cancer/pleural-effusion
- https://www.mayoclinic.org/diseases-conditions/lung-cancer/symptoms-causes/syc-20374620
Read full bio of medha deb












