Non-Small Cell Lung Cancer and Pleural Effusion: Signs, Management, and Treatment
Understanding the complexities of non-small cell lung cancer and pleural effusion, including symptoms, risks, management strategies, and care options.
Non-Small Cell Lung Cancer and Pleural Effusion: A Comprehensive Overview
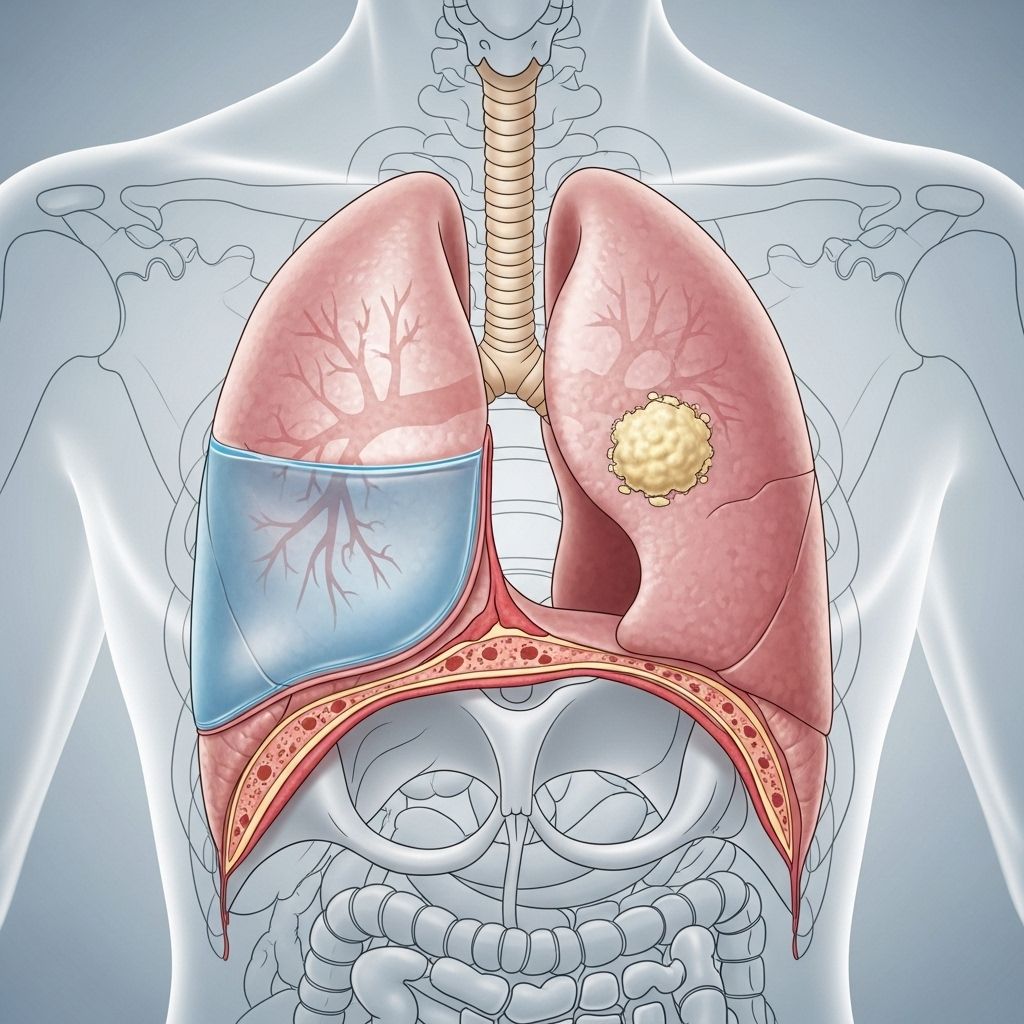
Non-small cell lung cancer (NSCLC) is the most common form of lung cancer, accounting for nearly 85% of cases. Its frequent association with pleural effusion—an abnormal accumulation of fluid between the layers of tissue lining the lungs and chest cavity—often complicates management and affects quality of life. Understanding the symptoms, risk factors, diagnostic processes, and available treatment options, including what to expect for those living with both NSCLC and pleural effusion, is essential for patients, families, and caregivers.
What Is Non-Small Cell Lung Cancer?
NSCLC forms in the tissues of the lungs, most commonly affecting individuals between the ages of 50 and 70. The condition can develop gradually, making early detection challenging. Unlike small cell lung cancer, NSCLC tends to grow and spread more slowly but is still frequently diagnosed at advanced stages due to subtle or absent early symptoms.
- Types: NSCLC includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
- Prevalence: The majority of lung cancer diagnoses are NSCLC.
- Main risk factor: Cigarette smoking remains the leading cause, with secondhand smoke, occupational exposure to carcinogens, and environmental pollution also contributing.
What Is Pleural Effusion?
Pleural effusion refers to the build-up of excess fluid between the pleura—the thin membrane covering the lungs—and the chest wall. In people with NSCLC, pleural effusion may result from direct spread of the tumor, inflammation, or blockage of lymphatic drainage.
- Common symptoms: Shortness of breath, chest discomfort, cough, and reduced exercise tolerance.
- Types:
- Transudative pleural effusion: Caused by pressure changes or decreased protein levels.
- Exudative pleural effusion: Caused by inflammation or malignancy, and more common in cancer patients.
Symptoms of NSCLC and Pleural Effusion
The symptoms of NSCLC often overlap with those of pleural effusion. Recognizing these early is crucial for timely diagnosis and management.
- Persistent cough that doesn’t improve or worsens
- Coughing up blood (hemoptysis)
- Chest pain or discomfort
- Shortness of breath and wheezing
- Hoarseness
- Loss of appetite
- Unexplained weight loss
- Fatigue and weakness
- Difficulty swallowing
- Swelling of the face and/or veins in the neck
- Reduced exercise tolerance due to fluid build-up
How Symptoms Progress
The development of a pleural effusion often indicates that NSCLC is advancing, especially for those already diagnosed with lung cancer. Fluid accumulation can worsen respiratory symptoms, making daily activities more difficult.
Risk Factors for Non-Small Cell Lung Cancer and Pleural Effusion
The likelihood of developing NSCLC and associated pleural effusion is shaped both by lifestyle and environmental exposures, as well as genetics and comorbidities.
- Cigarette smoking: Both active and passive exposure are primary risk factors.
- Exposure to workplace carcinogens: Asbestos, nickel, arsenic, vinyl chloride, and other occupational chemicals.
- Radiation exposure: Prior therapeutic radiation and environmental sources.
- Air pollution: Chronic exposure increases lung cancer risk.
- Family history of lung cancer.
- Previous infection or chronic lung disease: Conditions such as HIV increase risk.
- Advanced age: NSCLC is uncommon in younger people.
Diagnosis of NSCLC and Pleural Effusion
Because symptoms can be mistaken for other illnesses or the effects of smoking, many people are diagnosed after the cancer has advanced. Diagnostic approaches aim to confirm cancer, assess its spread, and distinguish the type of pleural effusion present.
- Imaging tests:
- Chest X-ray: Initial test to detect lung masses or fluid accumulation.
- CT scan: Provides detailed views of lungs and pleural space, useful for staging.
- PET and MRI scans: Identify metastatic spread or involvement of other organs.
- Laboratory tests:
- Bloodwork
- Analysis of pleural fluid after thoracentesis for protein content, cellular makeup, and tumor markers
- Biopsy procedures:
- Needle biopsy or surgical excision for tissue sampling
- Bronchoscopy: Visual examination and sampling of the airway and lung tissue
- Genetic testing: Determines cancer subtypes and guides therapy.
- Pleural fluid evaluation: Differentiates malignant versus benign effusion.
Diagnostic Table: Tests Used for NSCLC and Pleural Effusion
| Test | Purpose |
|---|---|
| Chest X-ray | Detects masses, fluid in pleural space |
| CT Scan | Shows location, size, and spread of tumor and effusion |
| Thoracentesis | Removes and analyzes pleural fluid |
| Biopsy | Confirms cancer diagnosis, subtype |
| Blood Tests | Detect markers, assess overall health |
Staging: Assessing How Far NSCLC Has Progressed
Staging refers to determining how extensively cancer has spread within the chest and to other areas of the body. Knowing the stage is critical for planning treatment.
- Stage I: Cancer localized to one lung
- Stage II: Cancer spread to nearby lymph nodes
- Stage III: Further spread, possible involvement of the chest wall
- Stage IV: Cancer has metastasized to distant organs or causes malignant pleural effusion
Treating NSCLC and Pleural Effusion
Treatment approaches depend on cancer type, stage, overall health, and the presence of pleural effusion.
Medical Treatments for NSCLC
- Surgery: For early-stage disease, removal of the affected lung tissue and surrounding nodes
- Radiation therapy: Kills or shrinks cancer cells locally
- Chemotherapy: Uses systemic drugs to kill cancer cells throughout the body
- Targeted therapy: Attacks specific genetic mutations found in tumor cells
- Immunotherapy: Boosts the body’s immune system to fight cancer
Managing Pleural Effusion
- Thoracentesis: Procedure to drain excess fluid and relieve symptoms
- Pleurodesis: Chemical irritation to fuse the pleura and prevent fluid recurrence
- Indwelling pleural catheter: Allows for regular drainage at home
- Treatment of underlying malignancy: Can sometimes resolve effusion
Supportive and Palliative Care
When NSCLC is advanced, symptom management and quality of life become top priorities. Palliative measures may include medications for pain, shortness of breath, and anxiety, as well as nutritional support and counseling.
Living With NSCLC and Pleural Effusion
Quality of life can be significantly affected. Fatigue, difficulty breathing, and emotional distress are common. Medical teams often include social workers, psychologists, and palliative specialists to address these issues.
- Monitor symptoms: Report any changes to your healthcare team promptly.
- Track fluid accumulation: Keep an eye on worsening breathlessness and swelling.
- Discuss advanced care planning: Consider preferences for medical interventions and supportive care.
- Engage in gentle physical activity: As tolerated, to maintain strength and mood.
- Nutrition: Seek guidance to maximize energy and reduce the risk of malnutrition.
Frequently Asked Questions (FAQs) About NSCLC and Pleural Effusion
Q: Can pleural effusion be cured in patients with NSCLC?
A: Pleural effusion caused by cancer often recurs, but treatments such as thoracentesis, pleurodesis, or placement of a pleural catheter can control symptoms and improve comfort.
Q: How can I tell if my shortness of breath is related to pleural effusion?
A: Shortness of breath from pleural effusion usually develops as fluid accumulates over time. It may worsen with physical activity or when lying down. Regular assessment by your medical team will include imaging and, if needed, drainage of the fluid.
Q: What support is available for people living with NSCLC and pleural effusion?
A: Supportive care teams address symptoms, help with emotional distress, and assist in coordinating palliative and advanced care services. Counseling and patient support groups may also provide valuable assistance.
Q: How is the underlying lung cancer treated along with pleural effusion?
A: Treatment often includes a combination of surgery (if feasible), chemotherapy, targeted therapy, and radiation. Managing the effusion involves regular drainage or preventive procedures for recurrent cases.
Q: Are there lifestyle changes that can help manage symptoms?
A: Yes. Maintaining good nutrition, engaging in appropriate exercise, monitoring fluid status, and optimizing the living environment for easy breathing can all contribute to improved well-being.
Key Takeaways for Patients and Caregivers
- NSCLC is the most frequent form of lung cancer and often leads to pleural effusion as the disease progresses.
- Early recognition of symptoms, especially breathlessness and cough, is vital for timely diagnosis and treatment.
- Diagnosis relies on multiple imaging and laboratory tests, biopsies, and fluid analysis.
- Treatment is multifaceted—including cancer-directed therapies, fluid management procedures, and supportive care.
- Living with NSCLC and pleural effusion requires ongoing adjustment, regular medical follow-up, and access to multidisciplinary support.
References
- https://www.yalemedicine.org/conditions/non-small-cell-lung-cancer
- https://ada.com/conditions/non-small-cell-lung-cancer/
- https://www.cancer.gov/types/lung/patient/non-small-cell-lung-treatment-pdq
- https://my.clevelandclinic.org/health/diseases/6203-non-small-cell-lung-cancer
- https://www.massgeneral.org/cancer-center/treatments-and-services/thoracic-cancers/lung-cancer/nsclc
- https://my.clevelandclinic.org/health/diseases/4375-lung-cancer
- https://www.mayoclinic.org/diseases-conditions/lung-cancer/symptoms-causes/syc-20374620
- https://www.dana-farber.org/cancer-care/types/non-small-cell-lung-cancer/diagnosis
Read full bio of Sneha Tete












