Understanding Non-Proliferative Diabetic Retinopathy: Early Detection, Symptoms, and Management
A comprehensive guide to non-proliferative diabetic retinopathy—its causes, symptoms, diagnosis, and prevention strategies for diabetic eye health.
What Is Non-Proliferative Diabetic Retinopathy?
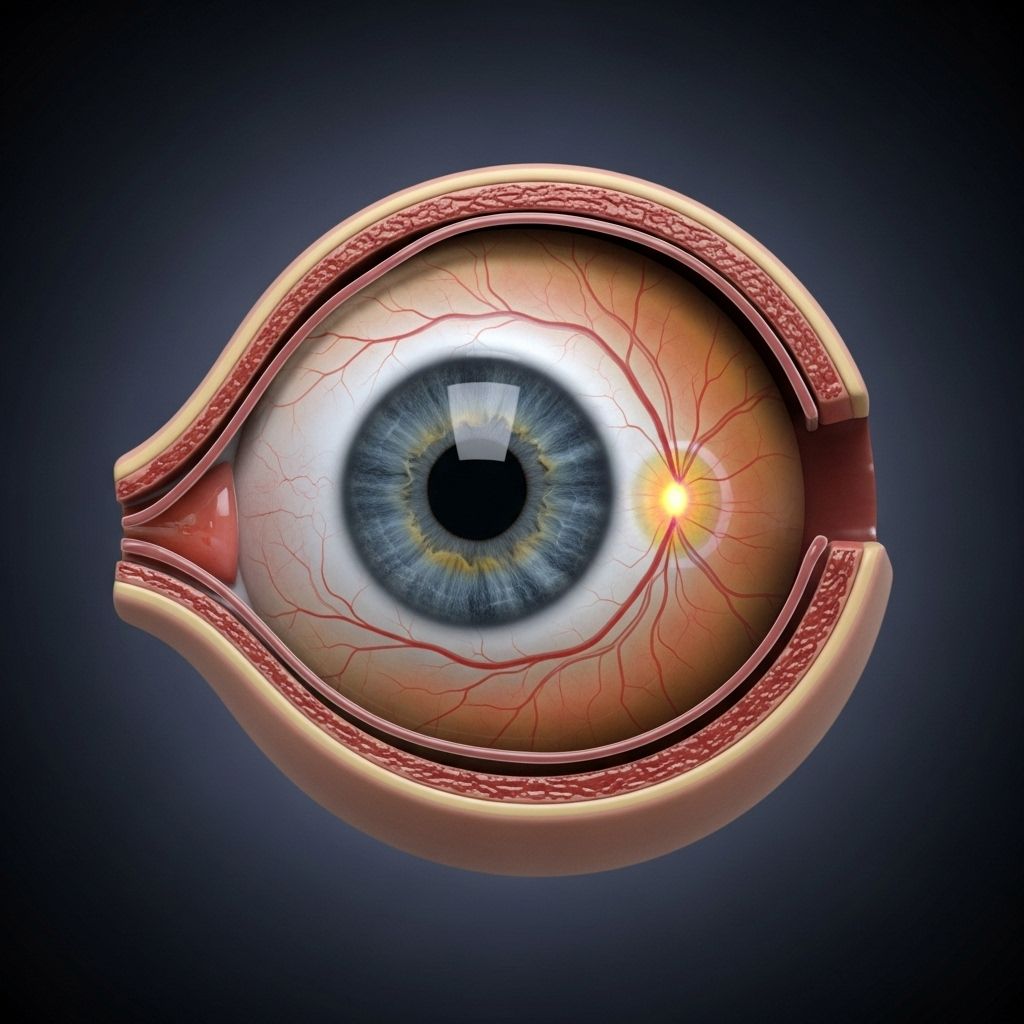
Non-proliferative diabetic retinopathy (NPDR) is the earliest stage of diabetic retinopathy, a frequent eye complication of diabetes that can threaten vision. NPDR is mainly defined by damage to the tiny blood vessels (capillaries) within the retina—the light-sensitive tissue lining the back of the eye. Over time, high blood sugar levels in diabetes erode these vessels, leading to leakage, swelling, bleeding, and other retinal changes that may result in vision problems if untreated.
- Diabetic retinopathy is a leading cause of blindness among those with diabetes, especially in working-age adults.
- NPDR usually occurs before the more serious, sight-threatening proliferative diabetic retinopathy (PDR).
- Early detection and routine monitoring are crucial because symptoms often develop slowly and may not be noticeable during initial stages.
Stages of Diabetic Retinopathy
Diabetic retinopathy progresses through distinct phases linked to the duration and control of diabetes:
| Stage | Main Characteristics | Potential Effects |
|---|---|---|
| Non-Proliferative (NPDR) | Capillary leakage, microaneurysms, small hemorrhages, retinal swelling (macular edema) | Blurry vision, slower visual processing |
| Proliferative (PDR) | New blood vessel formation (neovascularization), vitreous hemorrhage, traction retinal detachment | Severe vision loss, floaters, sudden blindness |
Understanding the Retina’s Vulnerability to Diabetes
The retina contains an intricate network of tiny blood vessels crucial for nourishing its cells. Diabetes disrupts this delicate system through persistent high blood sugar, causing:
- Capillary wall damage (making them leaky)
- Formation of microaneurysms (tiny bulges that can bleed)
- Retinal swelling from fluid leakage
- Blockage of blood flow (causing retinal tissue death in severe cases)
Because these vessels are so small and delicate, they are among the first to show signs of diabetic injury—even before other bodily symptoms appear.
Key Risk Factors for NPDR Development
- Duration of Diabetes: Risk increases the longer a person has diabetes. About 85% of people with diabetes lasting over 15 years show signs of NPDR.
- Poor Blood Sugar Control: High average blood glucose speeds the development of retinal changes.
- High Blood Pressure: Elevated blood pressure worsens vessel damage.
- High Cholesterol: Increased blood lipids contribute to vessel corrosion.
- Smoking: Tobacco harms blood vessel health and can worsen retinopathy.
- Pregnancy: Blood sugar control may fluctuate, increasing risk of progression.
Symptoms: How NPDR Affects Vision
In the earliest stages, non-proliferative diabetic retinopathy rarely causes symptoms, meaning retina damage often progresses unnoticed. As NPDR worsens, typical symptoms include:
- Blurry or decreased vision (often due to macular edema or macular ischemia)
- Distorted vision
- Floaters (dark spots or lines that drift through vision)
- Colors appear faded or less vivid
Notably, many people with advanced NPDR may have little or no noticeable vision loss, making routine eye exams essential for early identification and management.
Common Signs Doctors Look For in NPDR
- Microaneurysms: Tiny bulges in blood vessels within the retina, often seen during dilated eye exam.
- Dot and blot hemorrhages: Small spots of retinal bleeding, evident on fundus photography.
- Hard exudates: Yellowish deposits within the retina, indicating chronic leakage and swelling.
- Cotton-wool spots: Soft, fuzzy white patches signaling minor infarctions in the nerve fiber layer.
- Macular edema: Swelling and thickening in the central retina (macula), best seen with slit-lamp biomicroscopy.
Later NPDR stages can include venous dilation, intraretinal microvascular abnormalities, and increased retinal swelling.
How NPDR Is Diagnosed
Diagnosis of non-proliferative diabetic retinopathy requires a comprehensive eye examination by an ophthalmologist or optometrist, which generally includes:
- Dilated fundus examination: Allows direct visualization and assessment of retinal changes.
- Slit lamp biomicroscopy: Evaluates macular edema and retinal thickening.
- Ophthalmoscopy (indirect): Examines outer retinal areas for subtle changes.
- Fundus photography: Documents disease status and progression for comparison over time.
- Fluorescein angiography: Highlights leaking or blocked blood vessels not always visible during standard exam.
Complications: When NPDR Progresses
When NPDR is left untreated or diabetes remains poorly controlled, the condition can progress to:
- Clinically significant macular edema: Leading cause of vision loss in diabetes, resulting from fluid accumulation and swelling in the macula.
- Proliferative diabetic retinopathy (PDR): Advanced form characterized by new, fragile blood vessel growth (neovascularization) which can bleed into the eye and cause retinal detachment or severe vision loss.
- Retinal tissue death (macular ischemia): Resulting from closure of retinal blood vessels, leading to permanent deficits in visual function.
Management: Treating and Monitoring NPDR
The main goals in NPDR management are slowing disease progression and preventing complications. Recommended approaches include:
- Tight blood sugar control: Maintaining optimal A1c levels significantly reduces risk and slows retinal damage.
- Managing high blood pressure and cholesterol: Essential for protecting retinal vessels and preventing worsening of retinopathy.
- Lifestyle changes:
- Quit smoking.
- Exercise regularly.
- Adopt a balanced diet low in simple sugars and saturated fats.
- Regular eye exams: Annual or more frequent dilated eye checkups allow doctors to identify and treat changes before vision loss occurs.
- Treatment for macular edema: May involve laser therapy, injections (anti-VEGF or corticosteroids) or close observation, depending on severity.
Prevention of Diabetic Retinopathy and Progression
While NPDR can develop in almost anyone with long-term diabetes, its progression and complications are largely preventable through:
- Consistent blood sugar monitoring and medication adherence.
- Controlling blood pressure and cholesterol with lifestyle and/or medication.
- Avoiding smoking and following medical nutrition therapy.
- Scheduling regular, comprehensive eye exams—even if vision seems stable.
- Cause-specific management during high-risk periods, such as pregnancy.
Frequently Asked Questions (FAQs)
Q: What is the difference between non-proliferative and proliferative diabetic retinopathy?
A: Non-proliferative diabetic retinopathy (NPDR) is the early stage marked by leaky, damaged retinal blood vessels without abnormal new vessel growth. Proliferative diabetic retinopathy (PDR) is advanced, featuring abnormal neovascularization, bleeding, and possible retinal detachment.
Q: Who is most at risk for NPDR?
A: People with long-standing diabetes, poor blood sugar control, high blood pressure, high cholesterol, smokers, and pregnant individuals are most vulnerable.
Q: How is NPDR detected if there are no symptoms?
A: Routine dilated eye exams and retinal imaging tests (fundus photography, fluorescein angiography) are critical, as NPDR often progresses silently.
Q: Can NPDR cause permanent vision loss?
A: Unmanaged NPDR may lead to significant vision-threatening complications like macular edema and retinal tissue death. Timely diagnosis and medical management dramatically reduce the risk of permanent damage.
Q: Is there a cure for NPDR?
A: There is no cure, but effective management—including tight blood sugar, blood pressure, and cholesterol control—can halt or reverse early changes and prevent severe vision loss.
Takeaway: Key Points to Protect Your Vision
- Non-proliferative diabetic retinopathy is an early, potentially reversible diabetic eye complication.
- Regular dilated eye exams are the only reliable way to catch NPDR early and prevent major vision loss.
- Strict diabetes management, healthy lifestyle choices, and ongoing physician monitoring are vital.
- If diagnosed with NPDR, ongoing care and treatment are available to protect vision and minimize complications.
References
- https://www.merckmanuals.com/professional/eye-disorders/retinal-disorders/diabetic-retinopathy
- https://www.lifebridgehealth.org/conditions/diabetic-retinopathy
- https://www.retinaeye.com/contents/common-diseases/diabetic-retinopathy1/non-proliferative-diabetic-retinopathy
- https://www.vagelos.columbia.edu/departments-centers/ophthalmology/education/digital-reference-ophthalmology/vitreous-and-retina/retinal-vascular-diseases/nonproliferative-diabetic-retinopathy-npdr
- https://www.retinalmd.com/retina-conditions/nonproliferative-diabetic-retinopathy
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://pmc.ncbi.nlm.nih.gov/articles/PMC381138/
- https://www.cdc.gov/diabetes/diabetes-complications/diabetes-and-vision-loss.html
Read full bio of Sneha Tete












