Neovascularization in Diabetic Retinopathy: Key Facts and Care
Learn how neovascularization marks the advanced stages of diabetic retinopathy, its causes, symptoms, major risks, and current treatment and prevention strategies.
Neovascularization in Diabetic Retinopathy: What You Should Know
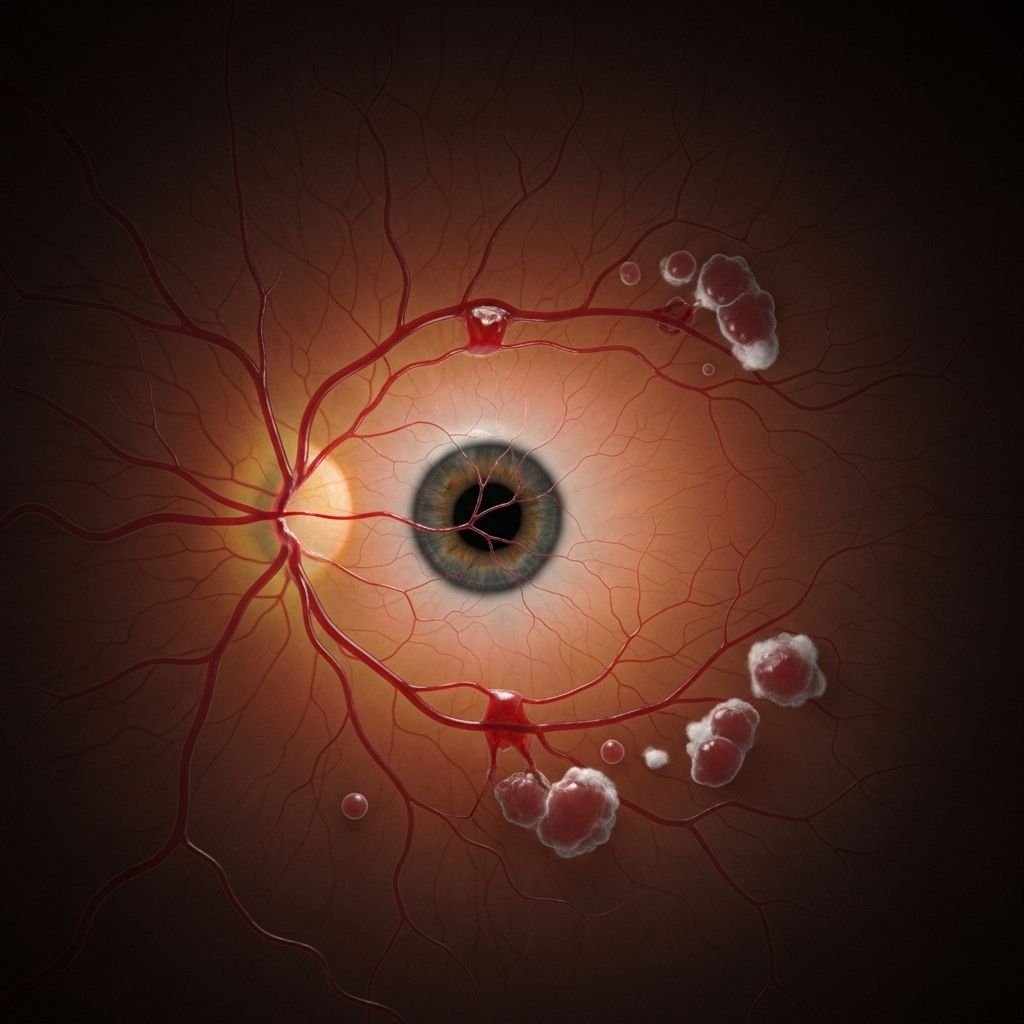
Neovascularization refers to the growth of new, often abnormal, blood vessels in the eye. In people with diabetes, it marks the most advanced stage of diabetic retinopathy—a serious condition that can result in permanent vision loss. This article explains how neovascularization develops in diabetic retinopathy, its causes, symptoms, risk factors, treatment options, and essential steps for prevention.
Understanding Neovascularization and Diabetic Retinopathy
In medical terms, neovascularization describes the formation of new blood vessels in tissues where they do not normally occur. In the context of diabetic retinopathy, it is the body’s response to damage and insufficient blood flow in the retina, the light-sensitive layer of the eye that sends visual signals to the brain.
Diabetic retinopathy is a common complication of diabetes. Over time, high blood sugar can break down or block tiny blood vessels in the retina, resulting in tissue hypoxia (low oxygen) and eventual vision problems. As compensation, the retina releases chemical signals—such as vascular endothelial growth factor (VEGF)—that encourage the growth of new vessels. Unfortunately, these new vessels are fragile and prone to leaking or bleeding into the eye, further worsening vision.
Stages of Diabetic Retinopathy: When Does Neovascularization Occur?
Diabetic retinopathy progresses through several stages, culminating in a phase characterized by neovascularization.
- Nonproliferative Diabetic Retinopathy (NPDR): Early stage. Blood vessels in the retina become weak, leaking blood or fluid. Often there are no symptoms.
- Proliferative Diabetic Retinopathy (PDR): Advanced stage. Neovascularization occurs—new, abnormal blood vessels grow on the retina or the optic nerve. This marks a dangerous turning point, as the new vessels can bleed, scar, and contribute to severe complications.
Neovascularization is the defining feature of proliferative diabetic retinopathy, which is associated with a higher risk of vision loss and blindness if left untreated.
What Causes Neovascularization in Diabetic Retinopathy?
The root cause of neovascularization is chronic damage to the retinal blood vessels from high blood sugar levels (hyperglycemia). Here’s how the process unfolds:
- Blood vessel injury: Persistent hyperglycemia damages retinal blood vessels, making them leaky and dysfunctional.
- Ischemia and hypoxia: Damaged vessels struggle to deliver enough oxygen and nutrients to the retina, which senses the shortage.
- VEGF release: In response, the retina produces more vascular endothelial growth factor (VEGF), a protein that stimulates new blood vessel formation.
- Abnormal vessel growth: The resulting new blood vessels grow in atypical locations. They are thin-walled, easily ruptured, and may block areas where normal eye fluid drains, leading to increased eye pressure.
These fragile vessels present a double threat: they are likely to rupture and cause bleeding, and can also lead to scarring, which threatens the structural integrity of the retina itself.
Symptoms: How Does Neovascularization Affect Vision?
Proliferative diabetic retinopathy, marked by neovascularization, often brings noticeable changes in vision. Early detection is key, so recognizing these symptoms is essential:
- Blurred vision
- Seeing floaters (spots or dark shapes drifting across your visual field)
- Difficulty seeing at night (night blindness)
- Distortion or waviness in central vision
- Sudden loss of vision in one or both eyes
- Black or gray spots in central vision
- Colors appearing washed out or faded
- Blank or dark areas in the field of vision
Because symptoms may not be obvious in the earliest stages, people with diabetes may not realize their eyes are being affected until significant damage has occurred.
Risk Factors for Diabetic Retinopathy and Neovascularization
Anyone with diabetes (type 1 or type 2) is at risk, but certain factors increase the likelihood of developing severe retinopathy and neovascularization:
- Poorly controlled blood sugar (high A1c levels)
- Long duration of diabetes
- Use of insulin
- High blood pressure (hypertension)
- Male sex
Regular screening and optimal diabetes management are critical, even in the absence of vision symptoms.
Complications: Why Is Neovascularization Dangerous?
Neovascularization in diabetic retinopathy is associated with a range of serious eye complications:
- Vitreous Hemorrhage: New vessels rupture, leaking blood into the gel-like center of the eye (vitreous), causing sudden vision loss or floaters.
- Traction Retinal Detachment: Scar tissue forms along with new vessels, pulling the retina away from the back of the eye. This can lead to permanent vision loss.
- Neovascular Glaucoma: Abnormal vessels can grow on the iris or in the drainage angle, blocking fluid outflow, increasing intraocular pressure, and damaging the optic nerve.
According to some studies, up to 25% of diabetes-related vision loss cases are caused by proliferative diabetic retinopathy.
Diagnosis: How Is Neovascularization Detected?
Diagnosing neovascularization and diabetic retinopathy relies on specialized eye exams and imaging techniques:
- Dilated Eye Exam: An ophthalmologist uses eye drops to widen the pupil and view the retina for signs of abnormal vessel growth or bleeding.
- Optical Coherence Tomography (OCT): Non-invasive scan producing high-resolution cross-sectional images of the retina to detect swelling or new vessels.
- Fluorescein Angiography: A special dye is injected into the bloodstream, and photographs are taken as it circulates through the retina, highlighting abnormal vessels and areas of leakage.
Regular eye screenings are essential for anyone with diabetes, even if no vision changes are present.
Treatment Options for Neovascularization in Diabetic Retinopathy
Early intervention provides the best chance of saving vision. Treatment strategies aim to stop abnormal vessel growth, prevent bleeding, and stabilize or improve vision. Current therapies include:
- Anti-VEGF Injections: Medications injected directly into the eye block VEGF, reducing new vessel growth and leakage. Examples include ranibizumab and aflibercept.
- Laser Photocoagulation: High-energy laser light is used to seal leaking blood vessels or destroy abnormal areas of retinal tissue, reducing the stimulus for neovascularization.
- Vitrectomy Surgery: Performed if there is bleeding into the vitreous or scar tissue threatening the retina, this surgical procedure removes blood and scar tissue, sometimes combined with laser treatment.
- Corticosteroid Injections: Less commonly, steroids can be injected into the eye to reduce inflammation and swelling.
Your ophthalmologist may recommend a combination of these treatments depending on the severity and extent of the disease. Timely treatment can help prevent severe vision loss and complications.
Prevention and Self-Care
While advanced diabetic retinopathy can be treated, prevention remains the cornerstone of protecting your vision. Here are critical steps:
- Maintain Target Blood Sugar Levels: Keep glucose within recommended ranges according to your diabetes care plan.
- Control Blood Pressure and Lipids: Manage hypertension and high cholesterol through diet, medication, and lifestyle.
- Follow a Balanced Diabetic Diet: Adhere to nutrition plans designed to stabilize blood sugar and promote eye health.
- Exercise Regularly: Engage in physical activity as cleared by your doctor to promote overall vascular health.
- Attend Regular Eye Exams: Get a comprehensive dilated eye exam at least once a year, or more often as recommended by your eye doctor.
- Report Vision Changes Promptly: Notify your healthcare provider immediately if you notice any changes to your vision.
Prevention strategies can slow or even halt the onset and progression of diabetic eye disease.
Frequently Asked Questions (FAQs)
1. What is neovascularization in diabetic retinopathy?
Neovascularization is the abnormal growth of new blood vessels in the retina. In diabetes, it occurs as a late-stage response to persistent damage and insufficient oxygen delivery to the retina, often signaling the advanced form called proliferative diabetic retinopathy.
2. How does neovascularization cause vision loss?
The new blood vessels are weak and prone to leaking blood or fluid into or onto the retina, leading to visual disturbances, scarring, retinal detachment, and sometimes permanent blindness.
3. Who is most at risk for developing neovascularization?
Anyone with diabetes can develop diabetic retinopathy, but the risk is greater with poor blood sugar control, long-standing diabetes, use of insulin, high blood pressure, and being male.
4. Can neovascularization be cured?
There is no cure, but with early detection and modern treatments such as anti-VEGF injections and laser therapy, the progression can be slowed or halted, and vision may stabilize or improve.
5. What are the first signs of proliferative diabetic retinopathy?
Early signs include blurred vision, floaters, difficulty seeing at night, or sudden vision loss. Regular eye exams are crucial for timely detection, as early stages can be asymptomatic.
Key Takeaways
- Neovascularization signals advanced diabetic retinopathy and requires prompt treatment to preserve vision.
- It results from long-term damage to retinal blood vessels due to uncontrolled diabetes.
- Symptoms may include vision changes, floaters, and even sudden vision loss.
- Early intervention with anti-VEGF therapy, laser photocoagulation, and surgery is effective in managing progression.
- Prevention through blood sugar, blood pressure control, and regular eye screening is the most effective defense.
References
- MedicalNewsToday. “What is neovascularization in diabetic retinopathy?”
- Healthline. “Neovascularization in Diabetes Retinopathy: What You Should Know”
References
- https://www.medicalnewstoday.com/articles/neovascularization-diabetic-retinopathy
- https://www.healthline.com/health/diabetes/neovascularization-diabetic-retinopathy
- https://www.centerwellpharmacy.com/articles/treating-diabetic-retinopathy.html
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
- https://optometricmanagement.com/issues/2020/november/zoom-out-on-diabetes/
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://www.naturaleyecare.com/blog/diabetic-retinopathy-the-four-stages/
- https://www.froedtert.com/eye-institute/common-eye-disorders/diabetic-retinopathy
Read full bio of Sneha Tete












