Necrotizing Soft Tissue Infection: Causes, Symptoms, and Treatment
Learn about necrotizing soft tissue infection, a rare but serious condition, its symptoms, diagnosis, risk factors, complications, and essential treatment strategies.
Necrotizing Soft Tissue Infection
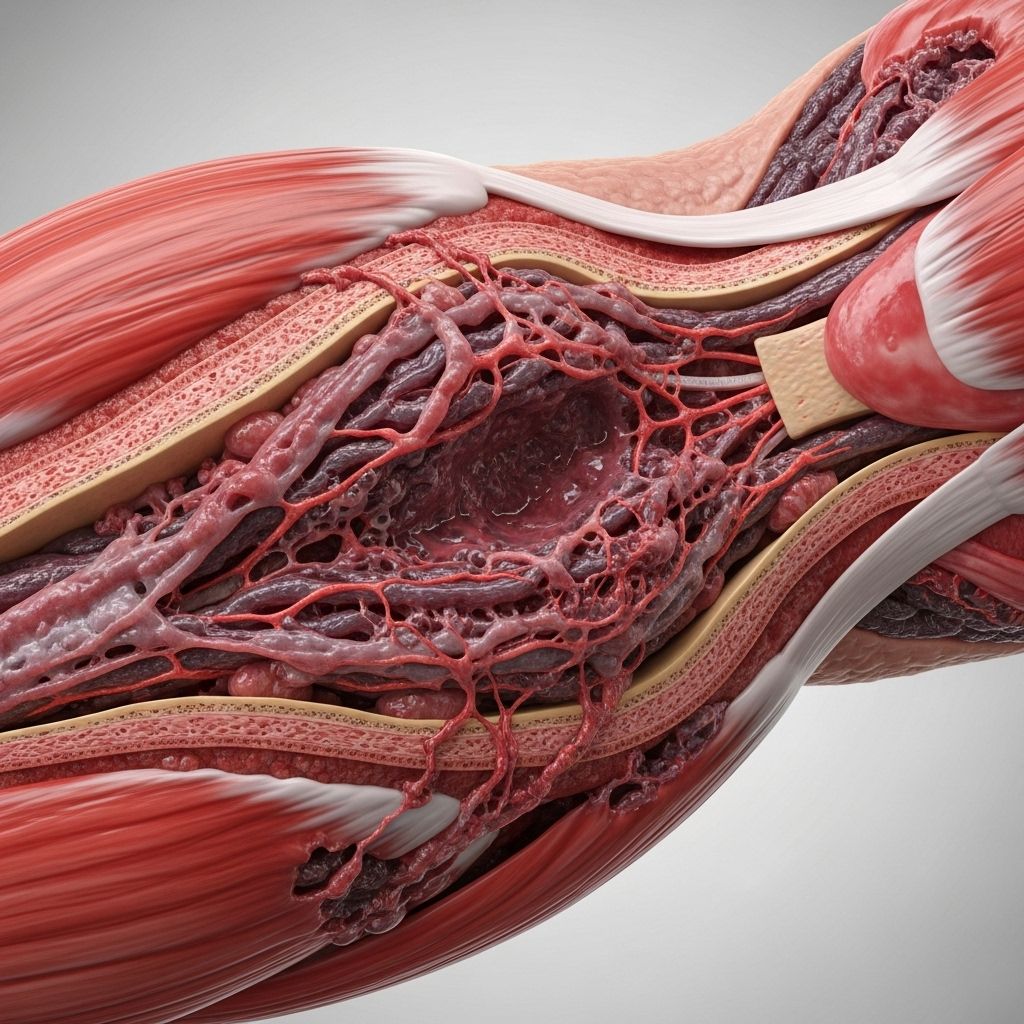
Necrotizing soft tissue infection (NSTI) is a rare, severe, and rapidly progressing bacterial infection that can destroy skin, muscle, and underlying tissue. Prompt recognition and emergency treatment are crucial, as the condition can quickly become fatal if not addressed.
What Is Necrotizing Soft Tissue Infection?
Necrotizing soft tissue infection refers to a group of infections that cause tissue death (necrosis) in the skin, underlying fat, fascia, and sometimes muscle. When bacteria enter through a break in the skin, they release toxins that damage tissue and disrupt blood flow, causing rapid destruction of the affected area. NSTI is sometimes referred to as “flesh-eating disease” or necrotizing fasciitis when deeper tissues such as the fascia are involved.
Why Is NSTI So Dangerous?
The biggest danger of NSTI is how quickly it advances. Tissue destruction and systemic toxicity can progress within hours, leading to shock, organ failure, and death if not diagnosed and treated urgently. Even with optimal intervention, NSTI carries a high risk of lasting complications and mortality.
Causes
Necrotizing soft tissue infections are most commonly caused by bacteria, often a mix of different types (polymicrobial), but sometimes by a single species. The infection usually starts when bacteria enter through a minor cut, scrape, insect bite, surgical wound, or other breach in the skin.
- Group A Streptococcus (Streptococcus pyogenes): often known as “flesh-eating bacteria”.
- Staphylococcus aureus (including MRSA).
- Clostridium species.
- Escherichia coli (E. coli).
- Aeromonas hydrophila, Klebsiella, and others.
These bacteria produce toxins that directly destroy tissue and impair the body’s immune response. In rare cases, fungal infections can also cause similar soft tissue destruction, especially in immunocompromised individuals.
How Do You Get NSTI?
The vast majority of cases follow an opening in the skin, such as:
- Minor cut or abrasion
- Puncture wound
- Surgical incision
- Burn
- Animal or insect bite
Many cases have no obvious entry point, highlighting the stealthy nature of this infection.
Risk Factors
While NSTI can occur in healthy individuals, certain risk factors increase susceptibility:
- Diabetes
- Weakened immune system (HIV, steroid use, chemotherapy, chronic illness)
- Chronic skin disease or ulcers
- Recent surgery or trauma
- Peripheral vascular disease
- Obesity
- Alcohol or substance use disorder
Despite these, NSTI can occasionally develop in completely healthy people following a seemingly minor injury.
Symptoms
Early symptoms of necrotizing soft tissue infection can be misleading because they may resemble minor skin or muscle injuries. Rapid worsening and the intensity of pain compared to the visible skin changes are key warning signs.
Common Symptoms
- Severe pain—often out of proportion to the apparent injury
- Swelling and redness that spread quickly
- Painful, red, or swollen area that may start as a lump or bump
- Skin that turns dark (dusky) or develops blisters
- Rapidly enlarging bruise or patch of discoloration
- Areas of skin turning black (tissue death)
General and Systemic Symptoms
- Fever and chills
- Fatigue
- Weakness
- Vomiting or nausea
- Dizziness
- Feeling severely ill
- Confusion or decreased alertness (if infection progresses to shock)
In the late stages, the affected skin may break open and ooze fluid. If left untreated, septic shock (a life-threatening whole-body reaction to infection) can develop, characterized by low blood pressure, confusion, and organ failure.
Diagnosis
Diagnosis of necrotizing soft tissue infection can be challenging, especially in early stages when skin changes are subtle. A high index of suspicion is required if symptoms progress rapidly or pain is severe and out of proportion to physical findings.
Steps in Diagnosis
- Clinical assessment of pain, rate of progression, and symptoms
- Physical examination for swelling, skin discoloration, blistering, and crepitus (a crackling feeling under the skin indicating gas production)
- Laboratory tests (inflammatory markers, white cell count, blood cultures)
- Imaging tests (X-ray, ultrasound, MRI, or CT scan) may show gas in tissue, swelling, or tissue destruction
- Surgical exploration (opening the affected area) may be needed to confirm diagnosis and determine the extent of tissue involvement
Prompt diagnosis and immediate action are critical for patient survival, as delays significantly increase the risk of severe complications and death.
Complications
Necrotizing soft tissue infection is a medical emergency. Without rapid treatment, NSTI can lead to:
- Sepsis (severe systemic infection)
- Shock (dangerously low blood pressure and organ failure)
- Extensive tissue loss (sometimes requiring amputation)
- Multi-organ failure
- Death: Mortality rates range from 25% to 35% in recent studies—even higher if not treated early
- Scarring and deformity: Reconstructive surgery is often required for survivors
Treatment
An aggressive, multidisciplinary approach to treatment is necessary for the best possible outcome. Treatment typically involves:
- Emergency surgery: Immediate and repeated surgical removal (debridement) of all dead tissue to control the spread of infection
- Strong intravenous (IV) antibiotics: Delivered directly into the veins, covering a broad range of bacteria. Antibiotic selection is based on the types of bacteria suspected or identified.
- Supportive care: Including IV fluids, medications to support blood pressure, and other measures as needed for organ support
- Wound care: Specialized wound management with frequent dressing changes and tissue hygiene is essential
- Pain management and other supportive therapies to stabilize bodily functions
Surgical Procedures
- Repeated debridements may be necessary, as the infection often extends beyond what is visible
- In some cases, amputation of a limb may be required to save a person’s life
- Reconstructive surgery: Skin grafts and plastic surgery procedures are often needed to cover large wounds after the infection is controlled
Infection Control in Hospital Settings
To prevent spread and reduce secondary infections, hospitals adhere to strict protocols including:
- Hand hygiene by healthcare workers and visitors
- Use of protective gowns, gloves, and masks
- Wound isolation when appropriate
Recovery and Outlook
Even with prompt treatment, necrotizing soft tissue infections can leave survivors with significant disabilities due to tissue loss, scarring, and the need for further surgeries. Full recovery often requires:
- Extended hospitalization (weeks to months)
- Physical rehabilitation for loss of tissue, muscle, or limbs
- Ongoing wound care and skin grafting
Long-term follow-up is vital to manage complications, psychological impact, and optimize functional recovery. Emotional and psychological support are important, as the trauma of the disease and recovery process can be severe for patients and families.
Prevention
- Practice good hygiene and keep wounds clean
- Promptly treat even small cuts, scrapes, or bites with cleansing and proper care
- Watch for signs of infection after injury or surgery and seek care if symptoms worsen
- People with diabetes or compromised immunity should be especially cautious
Frequently Asked Questions (FAQs)
Q: What makes NSTI different from other skin infections?
A: NSTI spreads much more rapidly and involves deeper tissues than typical skin infections, with a high risk of life-threatening complications and tissue destruction.
Q: Is necrotizing fasciitis the same as necrotizing soft tissue infection?
A: Necrotizing fasciitis is a specific type of necrotizing soft tissue infection, involving the fascia (a deep layer of tissue); NSTI is a broader term including infections of skin, fat, muscle, and fascia.
Q: How can I recognize early signs of NSTI?
A: Watch for severe or rapidly worsening pain, swelling, and skin changes after any skin injury, especially if the pain seems disproportionate to the appearance of the wound.
Q: Can NSTI be prevented?
A: While not all cases are preventable, prompt care for wounds and seeking medical attention for unusual or worsening symptoms are key preventive strategies.
Q: What is the prognosis for necrotizing soft tissue infection?
A: With rapid diagnosis and treatment, many patients survive. However, mortality rates remain high, ranging from 25% to 35% even with optimal care. Survivors may require long-term rehabilitation for tissue loss and scarring.
Additional Resources
- CDC: Necrotizing Fasciitis (Flesh-eating Bacteria)
- MedlinePlus: Necrotizing Soft Tissue Infection
- American Burn Association
Summary Table: Key Features of Necrotizing Soft Tissue Infection
| Aspect | Description |
|---|---|
| Cause | Bacterial infection (mainly group A Streptococcus, Staph aureus, others) |
| Entry | Wounds, surgery, cuts, bites, sometimes unknown |
| Symptoms | Severe pain, swelling, redness, rapid skin changes, fever, tissue death |
| Diagnosis | Clinical exam, imaging, surgical exploration, lab tests |
| Treatment | Urgent surgery, IV antibiotics, supportive care |
| Complications | Tissue loss, sepsis, multi-organ failure, death |
| Prevention | Good hygiene, timely wound care, monitor for infection |
References
- https://healthcare.utah.edu/burn-center/conditions-treatment/necrotizing-soft-tissue
- https://medlineplus.gov/ency/article/001443.htm
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4199388/
- https://www.healthline.com/health/necrotizing-soft-tissue-infection
- https://www.aafp.org/pubs/afp/issues/2003/0715/p323.html
- https://my.clevelandclinic.org/health/diseases/23103-necrotizing-fasciitis
- https://www.ncbi.nlm.nih.gov/books/NBK430756/
- https://www.merckmanuals.com/professional/dermatologic-disorders/bacterial-skin-infections/necrotizing-soft-tissue-infection
Read full bio of medha deb












