Necrotizing Pancreatitis: Causes, Symptoms, Treatment, and Prognosis
Understanding the severe complication of acute pancreatitis, its risk factors, symptoms, diagnosis, treatment strategies, and long-term outlook.
Necrotizing pancreatitis is a severe and potentially life-threatening complication of acute pancreatitis. In this article, you’ll learn how necrotizing pancreatitis develops, its risk factors, key symptoms, diagnosis methods, treatment options, prognosis, and prevention strategies, based on clinically reviewed information.
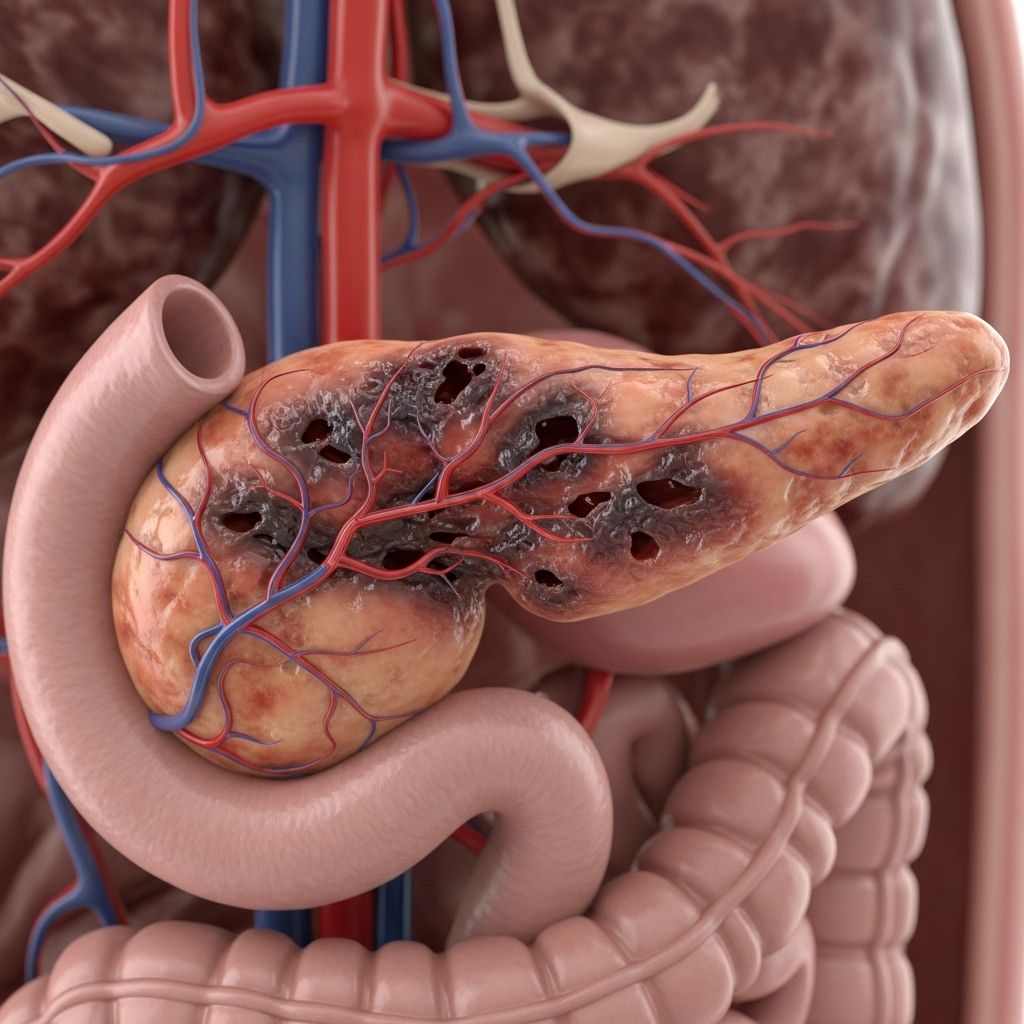
What Is Necrotizing Pancreatitis?
Necrotizing pancreatitis occurs when inflammation in the pancreas leads to the death (necrosis) of pancreatic tissue. This dead tissue is highly susceptible to infection, which can result in serious health complications and requires urgent medical attention.
The pancreas is a gland located behind your stomach that produces digestive enzymes and hormones such as insulin. In healthy individuals, these enzymes travel from the pancreas to the small intestine, aiding digestion. However, when the pancreas is inflamed—usually due to an acute attack—these enzymes may begin to digest the pancreatic tissue itself, leading to necrosis.
Causes of Necrotizing Pancreatitis
This dangerous complication can arise from a number of factors. The most common include:
- Acute pancreatitis left untreated or improperly treated — Necrotizing pancreatitis often develops when standard acute pancreatitis isn’t managed appropriately.
- Excessive alcohol consumption — Alcohol abuse is a leading cause.
- Gallstones — These can block the pancreatic duct, leading to inflammation.
- Pancreatic injury — Trauma can damage pancreatic tissue.
- Certain medications — Some drugs may trigger inflammation in the pancreas.
- High cholesterol — Elevated blood lipids can contribute to pancreatitis.
- High blood calcium — Hypercalcemia may increase risk.
- Autoimmune diseases — Conditions such as lupus.
- Pancreatic tumor — Both benign and malignant growths can obstruct the pancreas.
Occasionally, chronic pancreatitis (persistent long-term inflammation) may also predispose individuals to necrotizing pancreatitis, though this is rare.
Symptoms of Necrotizing Pancreatitis
The signs of necrotizing pancreatitis can be severe and may develop rapidly or gradually. The primary symptom is abdominal pain, which can be intense, wrap around to the back, and persist for several days.
- Abdominal pain (front, near the stomach, or radiating to back)
- Pain worsening after eating
- Swollen or tender abdomen
- Fever
- Nausea
- Vomiting
- Dehydration
- Rapid heart rate
- Low blood pressure
Patients may also experience fatigue, dizziness, and overall feeling unwell. Severe infection of necrotic pancreatic tissue can cause life-threatening complications if not addressed promptly.
How Is Necrotizing Pancreatitis Diagnosed?
Diagnosing this condition involves a combination of reviewing medical history, assessing symptoms, performing a physical examination, and using laboratory and imaging studies.
Diagnostic Procedures
- Imaging Studies
- Abdominal Ultrasound: Detects swelling or abnormalities in the pancreas.
- CT Scan: Provides detailed cross-sectional images to differentiate healthy from dead pancreatic tissue.
- MRI Scan: Offers high-resolution imaging for complex cases.
- Blood Tests
- Pancreatic enzyme levels (amylase, lipase)
- Electrolytes (sodium, potassium, glucose)
- Lipid profile (cholesterol, triglycerides)
- Biopsy
A fine needle aspiration may be required to determine if the dead tissue is infected. This is performed by extracting a small sample of pancreatic tissue for analysis.
Depending on the severity, additional tests may be ordered to assess organ function and screen for complications.
Treatment Strategies for Necrotizing Pancreatitis
Managing necrotizing pancreatitis involves treating acute pancreatitis itself as well as addressing necrotic tissue (dead areas of the pancreas).
1. Stabilizing Acute Pancreatitis
- Rest and IV Fluids: Hospitalization is often necessary for fluid resuscitation and rest.
- Pain Management: Painkillers help to control abdominal discomfort.
- Anti-nausea Medication: Medications may be needed to prevent vomiting and related symptoms.
- Nutrition Support: In severe cases, nutrition may be delivered via a nasogastric tube, providing the pancreas with rest from enzyme production.
2. Addressing Dead Pancreatic Tissue
- Antibiotics: Necessary only if the dead tissue is infected—prophylactic use is not recommended for sterile necrosis.
- Removal of Necrotic Tissue:
- Catheter Drainage: Minimally invasive approach to remove infection and necrotic debris.
- Endoscopic Necrosectomy: Uses an endoscope to extract dead tissue.
- Open Surgery: Required if less invasive means are inadequate or symptoms persist. Open necrosectomy carries risks such as bleeding and further infection and is reserved for severe cases.
- Postponing Other Procedures: Any other scheduled surgery will likely be delayed until pancreatitis is under control.
Summary Table: Treatment Approaches
| Treatment Modalities | Purpose | Notes |
|---|---|---|
| IV Fluids | Hydration & Stabilization | Essential, prevents shock |
| Painkillers | Symptom Relief | May be strong analgesics |
| Nasogastric Feeding | Nutritional Support | Bypasses pancreatic enzyme release |
| Antibiotics | Combat Infection | Only if necrosis is infected |
| Catheter/Endoscopic Removal | Debridement | Preferred for localized or mild cases |
| Open Surgery | Extensive Necrosectomy | Reserved for severe, unresponsive cases |
Outlook and Prognosis
The prognosis for necrotizing pancreatitis depends on the extent of pancreatic damage, speed and quality of intervention, and whether infection occurs. Prompt, appropriate treatment greatly improves chances of recovery.
- Mild to moderate cases: With timely care, most patients recover and return to normal health.
- Severe cases or delayed treatment: Risk of organ failure, sepsis, and death increases.
- Recovery time: Generally ranges from several weeks to months, depending on severity.
Complications such as diabetes or ongoing digestive problems may arise if large areas of the pancreas are damaged or removed.
Prevention Tips
Although not all cases are preventable, the risk of developing necrotizing pancreatitis can be minimized.
- Avoid excess alcohol consumption
- Manage gallstones by seeking prompt treatment for abdominal pain or jaundice
- Control cholesterol and calcium levels through regular checkups
- Inform your doctor about medications that may affect the pancreas
- Monitor and treat underlying autoimmune and pancreatic diseases
- Seek medical attention immediately for severe abdominal pain
Frequently Asked Questions (FAQs)
Q: How dangerous is necrotizing pancreatitis?
A: It is very dangerous. The risk of death increases significantly if infection takes hold or if large areas of the pancreas die. Hospitalization and close monitoring are mandatory.
Q: Can necrotizing pancreatitis be cured?
A: With early and appropriate medical intervention, most patients survive, but some may have long-term complications like digestive problems.
Q: What are the signs I should seek emergency care for possible pancreatitis?
A: Seek emergency attention for severe, persistent abdominal pain (especially if it wraps to the back), fever, vomiting, or unexplained rapid heart rate or low blood pressure.
Q: Will I need surgery if I develop necrotizing pancreatitis?
A: Not always. Surgery is only necessary if minimally invasive procedures cannot clear infection or necrosis, or if symptoms are intractable.
Q: Can necrotizing pancreatitis be prevented?
A: Some risk factors such as alcohol use and gallstones are modifiable. Managing these and seeking immediate medical care for abdominal pain can reduce the chance of progression to necrotizing pancreatitis.
Key Takeaways
- Necrotizing pancreatitis is a serious complication of acute pancreatitis where part of the pancreatic tissue dies and may become infected.
- Symptoms include severe abdominal pain, fever, vomiting, and dehydration.
- Diagnosis is done via physical exam, imaging (ultrasound, CT, MRI), and blood tests.
- Treatment requires hospital-based care, fluid resuscitation, nutritional support, antibiotics (for infection), and surgical removal of necrotic tissue if necessary.
- Prognosis depends on the severity and speed of intervention.
When to Seek Medical Help
Immediate medical attention is vital if you or someone you know is exhibiting signs of severe pancreatitis. Do not delay if you experience intense abdominal pain, fever, vomiting, or other concerning symptoms. Timely intervention can prevent the progression to necrotizing pancreatitis and save lives.
References
- https://www.medicalnewstoday.com/articles/321804
- https://www.healthline.com/health/digestive-health/necrotizing-pancreatitis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5565044/
- https://www.ccjm.org/content/84/8/639
- https://my.clevelandclinic.org/health/diseases/necrotizing-pancreatitis
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/n/necrotizing-pancreatitis.html
- https://my.clevelandclinic.org/health/diseases/8103-pancreatitis
- https://www.healthdirect.gov.au/pancreatitis
- https://www.cincinnatichildrens.org/health/n/necrotizing-pancreatitis
Read full bio of Sneha Tete












