Necrotizing Pancreatitis: Causes, Symptoms, Diagnosis, and Treatment
Understand necrotizing pancreatitis, its underlying causes, crucial symptoms, diagnostic approaches, and the latest treatment strategies.
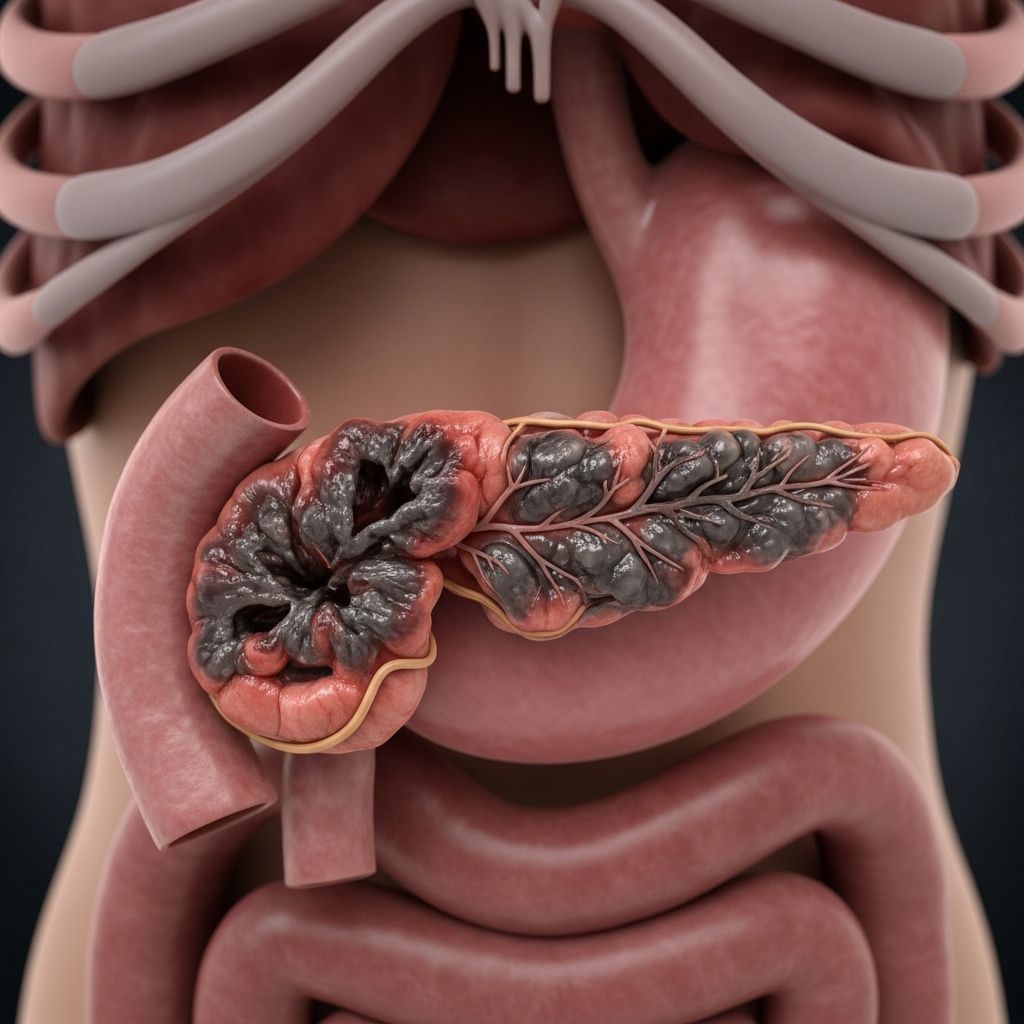
Necrotizing pancreatitis is a severe and potentially life-threatening complication of acute pancreatitis, characterized by the death (necrosis) of pancreas tissue due to inflammation and inadequate blood supply. This condition often leads to further issues if dead tissue becomes infected or causes organ dysfunction.
What is Necrotizing Pancreatitis?
Necrosis refers to permanent tissue death from lack of blood flow, injury, or severe inflammation. In necrotizing pancreatitis, sections of the pancreas die after a major inflammatory event. The pancreas—an organ behind the stomach—normally secretes digestive enzymes into the small intestine. When inflammation occurs, these enzymes leak into pancreatic tissue, resulting in significant tissue damage.
- Necrotizing pancreatitis is a complication of acute pancreatitis.
- Tissue death can lead to infection or development of walled-off necrosis (a fluid and debris collection), further increasing risk.
How Common Is Necrotizing Pancreatitis?
Necrotizing pancreatitis develops in approximately 20% of acute pancreatitis cases. In the United States, acute pancreatitis results in about 275,000 hospitalizations per year.
Causes of Necrotizing Pancreatitis
Necrotizing pancreatitis nearly always develops as a result of severe acute pancreatitis. Various underlying causes promote the inflammation and subsequent tissue death:
- Gallstones: Block pancreatic ducts, triggering inflammation.
- Alcohol misuse: Heavy and chronic alcohol intake is a leading risk factor.
- Pancreatic trauma: Injury or surgical procedures can damage the pancreas.
- High calcium/cholesterol levels: Metabolic issues can precipitate attacks.
- Pancreatic tumors or cysts: Obstruct ducts or damage tissue.
- Genetic & autoimmune conditions: Rarely, inherited or immune-mediated disorders target pancreatic tissue.
The sequence leading from acute pancreatitis to necrosis typically includes severe inflammation followed by impaired blood flow (ischemia), culminating in tissue death.
Symptoms of Necrotizing Pancreatitis
Initially, symptoms reflect those of acute pancreatitis. As this progresses, necrotizing pancreatitis develops more severe and critical manifestations. The most common symptoms are:
- Severe abdominal pain: Frequently starts in the upper abdomen, radiating to the back.
- Swollen belly and tenderness.
- Fever and chills: Indicate possible infection of necrotic tissue.
- Nausea & vomiting: Often persistent.
- Dehydration: Due to fluid loss from vomiting and inflammation.
- Low blood pressure: Severe disease may lead to shock.
- Rapid heart rate (tachycardia).
- Shortness of breath: Reflects systemic complications.
- Jaundice (yellowing of skin/eyes): Implies biliary obstruction.
Worsening symptoms—such as persistent high fever, chills, or increased pain—may signal that necrotic tissue has become infected, raising the risk for severe illness or organ failure.
Complications of Necrotizing Pancreatitis
- Infected necrosis: Bacteria may invade dead tissues, leading to severe sepsis.
- Pancreatic abscesses: Localized collections of pus can form
- Walled-off necrosis (WON): A delayed complication marked by fluid and necrotic debris enveloped by fibrous tissue, often occurring weeks after onset.
- Multi-organ failure: Severe systemic inflammation may impair other organs (kidney, lungs, heart).
Long-term Effects
- Chronic pancreatic insufficiency (difficulty digesting food)
- Diabetes (due to loss of insulin-producing cells)
- Repeated infections or abscesses
Diagnosis of Necrotizing Pancreatitis
Early diagnosis is essential for effective treatment. The process generally involves:
- Medical history and exam: Doctors assess symptom patterns, pain location, and risk factors (gallstones, alcohol use).
- Blood tests: Check levels of pancreatic enzymes (amylase, lipase), electrolytes (sodium, potassium), glucose, and triglycerides.
- Imaging studies:
- Abdominal ultrasound: Detect gallstones or abnormal fluid
- CT scan: Visualizes dead pancreatic tissue, complications, and extent of necrosis
- MRI: Further assesses tissue death and involvement
- Biopsy of pancreatic tissue (if indicated): To confirm infection in necrotic areas.
| Test | Purpose |
|---|---|
| Abdominal Ultrasound | Detect gallstones, fluid buildup, initial assessment |
| CT Scan | Identify tissue necrosis, quantify severity, detect complications |
| MRI | Detailed imaging of soft tissues, necrotic areas |
| Blood Tests | Assess enzyme levels, electrolyte disturbances |
| Biopsy | Confirm infection in dead tissue |
Treatment for Necrotizing Pancreatitis
Treatment typically proceeds in two main phases: addressing the initial pancreatitis and then managing the necrosis (including any infection or complications).
Initial Supportive Care
- IV fluids: Maintain blood volume and pancreatic perfusion.
- Pain control: Analgesics to manage severe pain.
- Nausea prevention: Medications to control vomiting.
- Rest: Limiting activity to reduce inflammation.
- Nutritional support:
- Oral feeding if symptoms are mild
- Nasogastric or nasojejunal feeding for severe cases (liquid nutrition via tube to stomach or small intestine)
Addressing Necrosis & Complications
- Antibiotics: Reserved for confirmed or highly suspected infection. Routine use is not recommended for sterile necrosis.
- Interventional procedures: If infected necrosis, abscess, or walled-off necrosis develops, patients may need:
- Image-guided drainage of infected fluid collections
- Endoscopic interventions (using a scope to remove fluid or dead tissue)
- Surgical removal (debridement) of dead tissue, often minimally invasive
Recovery and Prognosis
Recovery depends on the extent of necrosis, presence of infection, and timely treatment. Hospitalization is often required, and some patients may need intensive care support. Nutritional rehabilitation and gradual return to normal diet occur as symptoms improve. Complete healing can take weeks to months, and long-term monitoring for complications is needed.
Prevention Tips
- Treat gallstones promptly
- Reduce or eliminate alcohol consumption
- Manage cholesterol and calcium levels
- Address underlying autoimmune or hereditary conditions
Frequently Asked Questions (FAQs)
Q: What distinguishes necrotizing pancreatitis from acute pancreatitis?
A: Necrotizing pancreatitis is a severe complication of acute pancreatitis where parts of the pancreas die due to inflammation and lack of blood supply. It carries higher risk of infection and systemic complications.
Q: How soon do signs of necrosis appear?
A: It often takes a few days after the onset of acute pancreatitis for necrosis (pancreatic tissue death) to develop and become evident on imaging studies.
Q: Is surgery always required for necrotizing pancreatitis?
A: No, most cases are managed with supportive care and nutritional support. Surgery or drainage is only needed if infected necrosis or other major complications develop.
Q: What is walled-off necrosis?
A: Walled-off necrosis is a late complication, occurring about 4 weeks after initial pancreatitis, involving the encapsulation of dead tissue and fluid by a wall of fibrous tissue. This collection may cause pain, fever, or go unnoticed.
Q: What are the long-term outcomes?
A: With successful treatment, patients may recover fully, but some have recurring digestive issues or develop diabetes if much pancreas tissue was lost. Close follow-up is needed.
Summary Table: Key Features of Necrotizing Pancreatitis
| Aspect | Details |
|---|---|
| Definition | Death of pancreas tissue due to severe inflammation and lack of blood flow |
| Primary Causes | Gallstones, alcohol misuse, trauma, metabolic diseases, tumors |
| Main Symptoms | Severe abdominal pain, nausea, fever, vomiting, swollen belly |
| Diagnosis | Blood tests, imaging (CT, MRI, ultrasound), biopsy |
| Treatment | IV fluids, pain relief, nutritional support, antibiotics for infection, possible surgery |
| Long-term Outlook | Variable; depends on severity, infection risk, promptness of care |
When to Seek Medical Attention
Any sudden, severe abdominal pain—especially if accompanied by nausea, vomiting, fever, rapid heartbeat, or jaundice—should prompt urgent medical evaluation. Early intervention greatly improves outcomes in necrotizing pancreatitis.
References
- https://www.medicalnewstoday.com/articles/321804
- https://www.webmd.com/digestive-disorders/what-to-know-about-necrotizing-pancreatitis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5565044/
- https://www.cincinnatichildrens.org/health/n/necrotizing-pancreatitis
- https://my.clevelandclinic.org/health/diseases/necrotizing-pancreatitis
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/n/necrotizing-pancreatitis.html
- https://www.mayoclinic.org/diseases-conditions/pancreatitis/symptoms-causes/syc-20360227
- https://my.clevelandclinic.org/health/diseases/8103-pancreatitis
Read full bio of Sneha Tete












