Myopic Macular Degeneration: Causes, Symptoms, Treatment, and Outlook
Understand myopic macular degeneration – its causes, symptoms, progression, treatment options, and how to manage your eyesight long-term.
Myopic macular degeneration (MMD) is a progressive eye condition primarily affecting people with severe nearsightedness. This guide explores what MMD is, why it happens, how it affects vision, treatment options, and living with the condition.
What is Myopic Macular Degeneration?
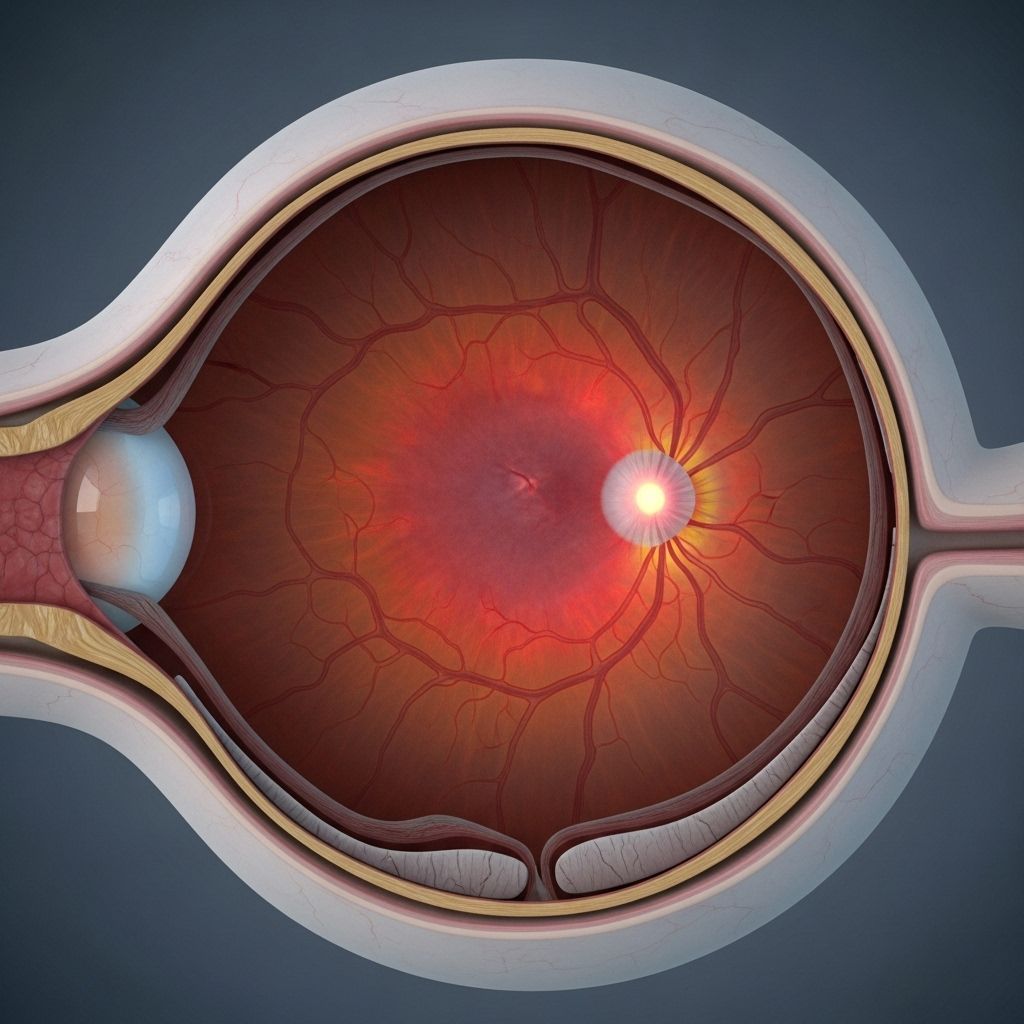
Myopic macular degeneration, also known as degenerative myopia, is a type of macular degeneration that targets individuals with high myopia. High myopia refers to extreme nearsightedness, often defined as greater than -5.00 diopters on a prescription scale . In these cases, the eyeball elongates more than normal, stretching tissues at the back of the eye and leading to progressive degeneration of the macula – the area of the retina responsible for central, detailed vision.
- Macula: Central part of the retina needed for sharp, detailed vision
- High myopia: Severe nearsightedness, often requiring strong corrective lenses
- MMD: Complication of high myopia, involving deterioration in the macula
How Does Myopia Cause Macular Degeneration?
People with myopia have an elongated eyeball. This affects the retina – the sensitive layer at the back of the eye. As the eye stretches, the retina, including the macula, thins and becomes fragile. Over time, abnormal changes can develop that result in vision loss .
Mechanisms Leading to Degeneration
- Retinal stretching: Leads to thinning and weak spots
- Photoreceptor disruption: Changes in the light-detecting cells can impair vision before visible degeneration
- Collagen abnormalities: Atypical collagen can weaken structural support, further raising risk
- Inflammation: Chronic inflammation may contribute to degenerative processes
Not everyone with high myopia develops MMD. However, those with pathological myopia, a subset involving degenerative changes, are at greater risk .
Who Gets Myopic Macular Degeneration?
MMD is seen in people with severe or pathological myopia. This is a global concern:
- Over 2 billion people have myopia worldwide
- About 4% develop high myopia
- Approximately 3% are affected by pathological myopia, raising the risk for MMD
Usually, myopia develops in childhood and stabilizes in early adulthood (ages 20–30), but complications like MMD emerge later, typically in adulthood.
Signs and Symptoms
Symptoms of MMD often develop gradually. In early stages, there may be few or no signs. As the disease progresses, people may notice increasing difficulty with tasks that require central vision.
| Common Symptoms | Description |
|---|---|
| Blurry spot or blank area in central vision | Darkened or missing area in the center of visual field |
| Distorted or wavy vision | Straight lines may appear bent due to changes in macular structure |
| Difficulty with color perception | Colors may be less vivid or harder to distinguish |
| Trouble adapting to lighting changes | Slower adaptation when moving between light and dark environments |
| Reduced visual clarity | Trouble reading, recognizing faces, or doing detailed tasks |
- Some people first notice vision distortion or a central blind spot
- Symptoms may worsen over several years
- Peripheral (side) vision usually remains intact
Complications Associated with High Myopia
People with high myopia are at increased risk for various retinal complications besides macular degeneration.
Key Complications
- Retinal atrophy: The retina thins and deteriorates, leading to permanent vision loss if the central (macular) area is affected
- Lacquer cracks: Tiny breaks in Bruch’s membrane layer between the retina and choroid, potentially leading to bleeding and further damage
- Choroidal neovascularization (CNV): New, fragile blood vessels grow under the retina, prone to leaking fluid or blood (a cause of vision loss in “wet” MMD)
- Retinal detachment: The retina can pull away from the back of the eye, causing flashes, floaters, and sudden vision loss; requires urgent treatment
‘Wet’ vs. ‘Dry’ Myopic Macular Degeneration
| Type | Description | Risk |
|---|---|---|
| Dry MMD | Gradual thinning and degeneration of retina/macular cells | Slower vision loss |
| Wet MMD | Abnormal blood vessel growth, leakage, and bleeding under the retina | Faster, often more severe vision loss |
How Does Myopic Macular Degeneration Progress?
The progression of MMD varies widely from one person to another. In general:
- Slow progression over years: Vision changes are usually gradual, especially in ‘dry’ MMD
- Accelerated loss: Sudden decline may occur if ‘wet’ MMD develops or if complications like CNV or retinal detachment happen
- Variable onset: Some people never progress to significant macular degeneration despite high myopia
A 2020 study found that over 6 years, about 1.2% of people over 40 with myopia developed MMD, with progression in about 17% of those already affected.
Diagnosing Myopic Macular Degeneration
Diagnosis relies on a combination of patient history, eye examination, and advanced imaging.
Diagnostic Methods
- Visual acuity tests: Measures the sharpness and clarity of vision
- Retinal imaging: Optical coherence tomography (OCT), fundus photography, and fluorescein angiography reveal structural changes and abnormal blood vessels
- Eye health assessment: Checking for symptoms such as distortion, blind spots, and color changes
- Patient history: Assessment of high myopia, family history, and symptom duration
Treatment Options for Myopic Macular Degeneration
There is no cure for MMD, but treatments aim to preserve vision, slow progression, and manage complications.
Available Treatments
- Anti-VEGF injections: Used for ‘wet’ MMD. These medications (like ranibizumab, bevacizumab) inhibit abnormal blood vessel growth and leakage under the macula
- Laser therapy: Sometimes used for certain retinal tears or to treat abnormal vessels (less common now due to better pharmaceuticals)
- Photodynamic therapy: Involves injecting a light-sensitive drug followed by laser activation to destroy abnormal blood vessels
- Corrective lenses: Glasses or contact lenses help correct underlying myopia but do not prevent or treat macular degeneration
- Low vision aids: Magnifiers, special glasses, and adaptive devices help maximize remaining vision for daily activities
Surgical repair may be needed for retinal detachment. Regular monitoring is crucial for timely detection and management of complications.
Prevention and Risk Reduction
While it may not be possible to prevent MMD altogether, several strategies may help delay progression or lower risks.
- Consistent eye exams: Especially for individuals with high or pathological myopia, to spot changes early
- Control of myopia progression: In children and young adults, methods such as atropine drops, special contact lenses, or orthokeratology may help slow myopia progression (and thus lower future risk)
- Protective eyewear: Reduces risk of trauma, especially in people with fragile retinas
- Healthy lifestyle: Managing cardiovascular health, quitting smoking, and eating a nutrient-rich diet may help maintain eye health
- Genetic counseling: For families with a strong history of myopia or retinal disease
Living with Myopic Macular Degeneration
MMD can significantly affect quality of life by impairing the ability to read, drive, or recognize faces. However, adaptive strategies and devices can help people maintain independence.
Coping Strategies
- Use magnifiers or electronic readers for reading and detailed tasks
- Increase lighting at home, especially for close work
- Arrange home and work environments to minimize fall risks and make navigation easier
- Seek help from low vision specialists or support groups
Medical advancements have improved outcomes, especially when ‘wet’ MMD is treated promptly. People with MMD should maintain ongoing care with an ophthalmologist.
Frequently Asked Questions (FAQs)
What causes myopic macular degeneration?
MMD is primarily caused by the excessive elongation of the eyeball in high myopia, leading to stretching and thinning of the retina and macula.
Does everyone with high myopia develop macular degeneration?
No. While high myopia increases the risk, only a minority advance to MMD, particularly those with pathological changes to the retina.
Can vision loss from myopic macular degeneration be reversed?
Lost vision from MMD is usually permanent, but prompt treatment, especially for ‘wet’ forms, can preserve remaining sight and slow decline.
What are the symptoms I should watch for?
Watch for blurry or blank spots in central vision, distortion, trouble distinguishing colors, or sudden vision changes.
How can I reduce my risk of progression?
Attend regular eye exams, use prescribed treatments promptly, protect your eyes, and manage overall health to support ocular wellness.
Key Takeaways
- Myopic macular degeneration is a serious complication in people with high myopia.
- Symptoms, when present, often progress slowly but can lead to significant visual disability.
- Timely diagnosis, regular monitoring, and new treatment options offer hope for vision preservation.
- People living with MMD can use adaptive tools and make lifestyle adjustments to maintain independence and quality of life.
- If you notice any sudden changes in vision, seek immediate advice from an eye health professional.
References
- https://www.medicalnewstoday.com/articles/myopic-macular-degeneration
- https://www.medicalnewstoday.com/articles/how-fast-does-high-myopia-macular-degeneration-progress
- https://www.mdfoundation.com.au/about-macular-disease/other-macular-conditions/myopic-macular-degeneration/
- https://www.healthline.com/health/macular-degeneration
- https://www.macularsociety.org/macular-disease/macular-conditions/myopic-macular-degeneration/
- https://www.ncbi.nlm.nih.gov/books/NBK574560/
- https://www.webmd.com/eye-health/macular-degeneration/what-is-myopic-macular-degeneration
Read full bio of medha deb












