Myopericarditis: Symptoms, Causes, Diagnosis, Treatment, and Outlook
Learn about myopericarditis, a dual heart condition involving inflammation of both the myocardium and pericardium, its symptoms, diagnosis, complications, and treatments.
Understanding Myopericarditis
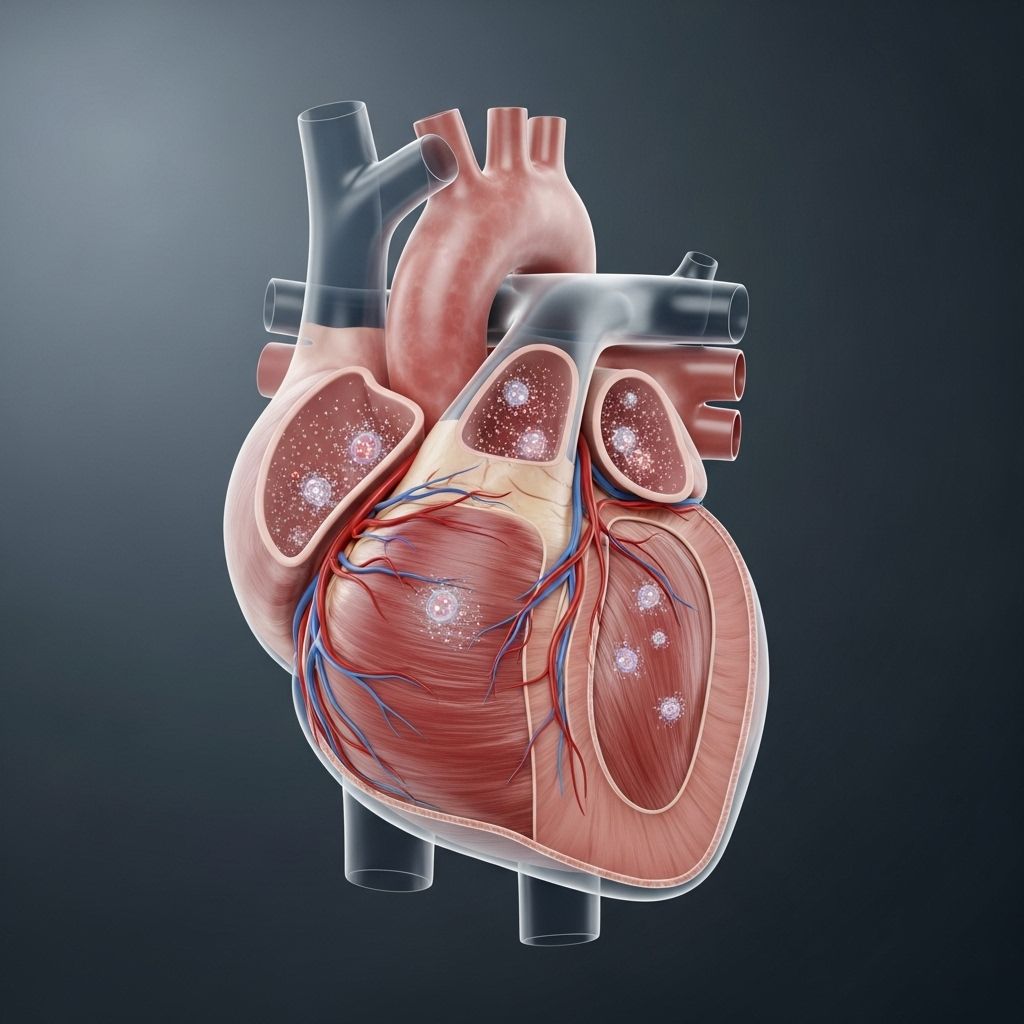
Myopericarditis is a medical term describing the simultaneous inflammation and irritation of both the myocardium (the heart muscle’s thickest layer) and the pericardium (the thin protective sac surrounding the heart). Most often, this condition results from a viral infection, but bacterial, autoimmune, and other causes are also possible. Myopericarditis is considered distinct from isolated myocarditis (muscle only) or pericarditis (sac only), as it affects both structures, often creating unique clinical challenges and symptoms.
Why Is Myopericarditis Important?
- Simultaneous involvement of heart muscle and the protective sac makes symptoms, potential complications, and required treatments more complex than in either isolated myocarditis or pericarditis.
- Early recognition and proper management are critical to avoid serious consequences such as heart failure or dangerous arrhythmias.
What Is Myopericarditis?
Myopericarditis commonly develops as a complication of pericarditis, which is inflammation confined to the pericardium. In these cases, the inflammation spreads deeper, affecting the myocardium and giving rise to more serious heart symptoms. If only the pericardium is affected, the condition is called pericarditis. If the heart muscle itself is involved, but not the pericardium, it’s called myocarditis.
Related Conditions
- Myocarditis: Inflammation of the heart muscle proper, often caused by viruses.
- Pericarditis: Inflammation and irritation of the sac around the heart, also usually viral in origin.
- Perimyocarditis: Inflammation primarily affecting both the pericardium and the underlying myocardium, closely related to myopericarditis.
Symptoms of Myopericarditis
Symptoms can range from mild to severe, depending on the extent of inflammation and the structures involved. Common symptoms include:
- Chest pain (sharp or stabbing; may worsen with deep breathing or lying down)
- Fatigue
- Shortness of breath, especially with exertion
- Palpitations (irregular, rapid, or pounding heartbeat)
- Fever, chills, or flu-like symptoms (if infection is present)
- Swelling in legs, ankles, or abdomen (when heart failure develops)
Some individuals may experience only mild chest discomfort, while others may suffer symptoms severe enough to limit physical activity and daily functioning.
When to Seek Medical Attention
- New, sudden, or unexplained chest pain should be evaluated by a healthcare provider right away.
- Severe shortness of breath, fainting, or rapid heart rate may indicate life-threatening complications and require emergency care.
Causes and Risk Factors
Myopericarditis most commonly arises following a viral infection. Other triggers include:
- Bacteria (rare: tuberculosis, Lyme disease, etc.)
- Autoimmune disorders (systemic lupus, rheumatoid arthritis, etc.)
- Medications and toxins (certain drugs, cancer treatments)
- Post-vaccine reaction (very rare cases following mRNA or Novavax COVID-19 vaccines, predominantly in young males)
Certain factors increase risk:
- Previous viral illness
- Chronic autoimmune disease
- Family history of heart disease
Although anyone can develop myopericarditis, it’s most frequently recognized in adolescents and young adults, possibly due to patterns of viral exposure and immune response.
Table: Common Causes of Myopericarditis
| Cause | Example | Notes |
|---|---|---|
| Viral Infection | Coxsackievirus, Influenza, COVID-19 | Most prevalent cause worldwide |
| Bacteria | Tuberculosis, Lyme disease | Rare; requires specific targeted therapy |
| Autoimmune | Lupus, Sjögren’s syndrome | Often chronic; may recur |
| Medications/Toxins | Doxorubicin, radiation | Typically in context of cancer treatment |
| Vaccination | mRNA COVID-19 vaccines | Very rare adverse event; usually mild and resolves |
Potential Complications of Myopericarditis
If diagnosed early and treated appropriately, serious complications are often avoidable. However, more severe or untreated myopericarditis can result in:
- Pericardial effusion: Accumulation of fluid in the pericardial sac, sometimes leading to cardiac tamponade (compression of the heart which is a medical emergency)
- Heart failure: Weakening of heart muscle function due to prolonged inflammation and scarring, can severely impair daily life, may be fatal if untreated
- Constrictive pericarditis: Chronic scarring, resulting in stiff, non-compliant pericardium that restricts normal heart function
- Arrhythmias: Irregular heartbeats due to scarring or damage to muscle and conduction tissue; severe types can be life-threatening.
Prompt diagnosis and close medical follow-up reduce the risk of these outcomes.
How Is Myopericarditis Diagnosed?
Diagnosis involves a combination of physical examination, laboratory tests, and cardiac imaging. Important diagnostic steps include:
- Physical examination: Listening for friction rubs, abnormal heart sounds, and checking for signs of heart failure.
- Blood tests: Inflammatory markers such as C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and white blood cell count are often elevated. Cardiac enzymes such as troponin may be increased when muscle damage occurs.
- Electrocardiogram (ECG): Can reveal rhythm disturbances or changes typical of pericarditis and myocarditis.
- Chest X-ray: May show enlarged heart shadow or signs of fluid accumulation.
- Echocardiogram: Evaluates heart structure and function, though may appear normal in milder cases.
- Cardiac Magnetic Resonance Imaging (CMR): Highly useful for showing inflammation in both the myocardium and pericardium, and for assessing impact on heart pumping capability.
- Endomyocardial biopsy: Reserved for cases where the diagnosis remains uncertain after noninvasive tests, or when specific tissue pathology is needed.
Timely diagnosis enables effective treatment and monitoring to prevent progression and complications.
Treatment Options for Myopericarditis
Treatment for myopericarditis focuses on reducing inflammation, managing symptoms, and preventing complications. Most mild cases resolve with anti-inflammatory therapy, while more severe or persistent cases require additional interventions.
Primary Treatment Strategies
- Nonsteroidal anti-inflammatory drugs (NSAIDs): First-line treatment for pain and inflammation.
- Colchicine: Often prescribed alongside NSAIDs to further curb inflammation and reduce recurrence risk.
- Corticosteroids: Used in cases resistant to NSAIDs or colchicine, especially when autoimmune processes are suspected.
- Managing underlying cause: Specific antibiotics for bacterial infections, immune-modulating therapies for autoimmune origins.
- Monitoring and supportive care: Hospitalization for severe cases involving heart failure or arrhythmias; close follow-up for medication adjustment and further testing.
Additional Support
- Physical activity restriction: Avoid strenuous exercise or competitive sports until inflammation fully resolves.
- Heart failure management: May require additional medications or, rarely, surgical interventions or implanted devices (such as pacemakers or defibrillators).
Most individuals recover completely with prompt treatment, though ongoing monitoring is required.
Prognosis and Outlook
The prognosis for myopericarditis depends on the underlying cause, severity, and how quickly treatment is started. Most cases are mild and resolve with no lasting damage, particularly those following viral infections.
- Full recovery: Common in mild cases expertly managed early, especially in young healthy individuals.
- Chronic complications: Rare, but possible if untreated or if initial damage is severe.
- Quality of life: Generally high after recovery, though monitoring continues for recurrence or late-onset complications.
Severe cases, particularly those progressing to heart failure or causing persistent arrhythmias, may require long-term therapy and cardiac monitoring.
Frequently Asked Questions (FAQs)
Q: Is myopericarditis the same as myocarditis or pericarditis?
A: No. Myopericarditis refers to simultaneous inflammation of both pericardium and myocardium. Myocarditis and pericarditis affect only one area.
Q: How serious is myopericarditis?
A: Most cases are mild and resolve with medical treatment. Severe cases can lead to heart failure or arrhythmias, which require prompt management.
Q: Is myopericarditis contagious?
A: Myopericarditis itself is not contagious, but it often results from viral infections that may be spread person-to-person.
Q: Can exercise make myopericarditis worse?
A: Yes—strenuous activity may worsen inflammation and cause complications. Physical activity should be restricted until full recovery is confirmed.
Q: Are COVID-19 vaccines linked to myopericarditis?
A: Cases have been reported very rarely, mostly in young males within a week after vaccination. Symptoms usually resolve quickly, and the overall risk is extremely low compared to the benefits of vaccination.
Q: What is the long-term outlook for people with myopericarditis?
A: The prognosis depends on severity and cause. Most recover fully with early treatment; ongoing monitoring may be needed for recurrence or complications.
Key Takeaways
- Myopericarditis is an uncommon but important condition involving both the heart muscle and its surrounding sac.
- Symptoms are variable but chest pain, fatigue, and abnormal heart rhythms are common.
- Early diagnosis and proper management are crucial to avoid serious complications.
- Most people experience full recovery with anti-inflammatory therapy and supportive care.
Summary Table: Myopericarditis at a Glance
| Aspect | Details |
|---|---|
| Definition | Simultaneous inflammation of myocardium and pericardium |
| Main Causes | Viruses, autoimmune diseases, drugs, rare vaccine reaction |
| Major Symptoms | Chest pain, fatigue, palpitations, shortness of breath |
| Complications | Heart failure, arrhythmias, pericardial effusion |
| Diagnosis | Blood tests, ECG, imaging (MRI, echo), biopsies in select cases |
| Treatment | NSAIDs, colchicine, corticosteroids, treat underlying cause |
| Prognosis | Often excellent if mild; severe cases need close monitoring |
References
This article synthesizes information from Healthline, CDC, AHA, StatPearls, and clinical guidelines from major cardiology organizations to deliver an accurate overview of myopericarditis.
References
- https://www.healthline.com/health/heart/myopericarditis
- https://www.cdc.gov/vaccines/covid-19/clinical-considerations/myocarditis.html
- https://www.ncbi.nlm.nih.gov/books/NBK441847/
- https://www.healthline.com/health/heart-disease/myocarditis
- https://www.ncbi.nlm.nih.gov/books/NBK534776/
- https://www.ahajournals.org/doi/10.1161/CIRCHEARTFAILURE.120.007405
- https://www.mayoclinic.org/diseases-conditions/myocarditis/symptoms-causes/syc-20352539
Read full bio of medha deb












