Myocarditis vs. Pericarditis: Understanding Inflammatory Heart Conditions
Learn the key differences, symptoms, causes, and treatment approaches for myocarditis and pericarditis, two closely related but distinct inflammatory heart conditions.
Myocarditis vs. Pericarditis: What’s the Difference Between These Inflammatory Heart Conditions?
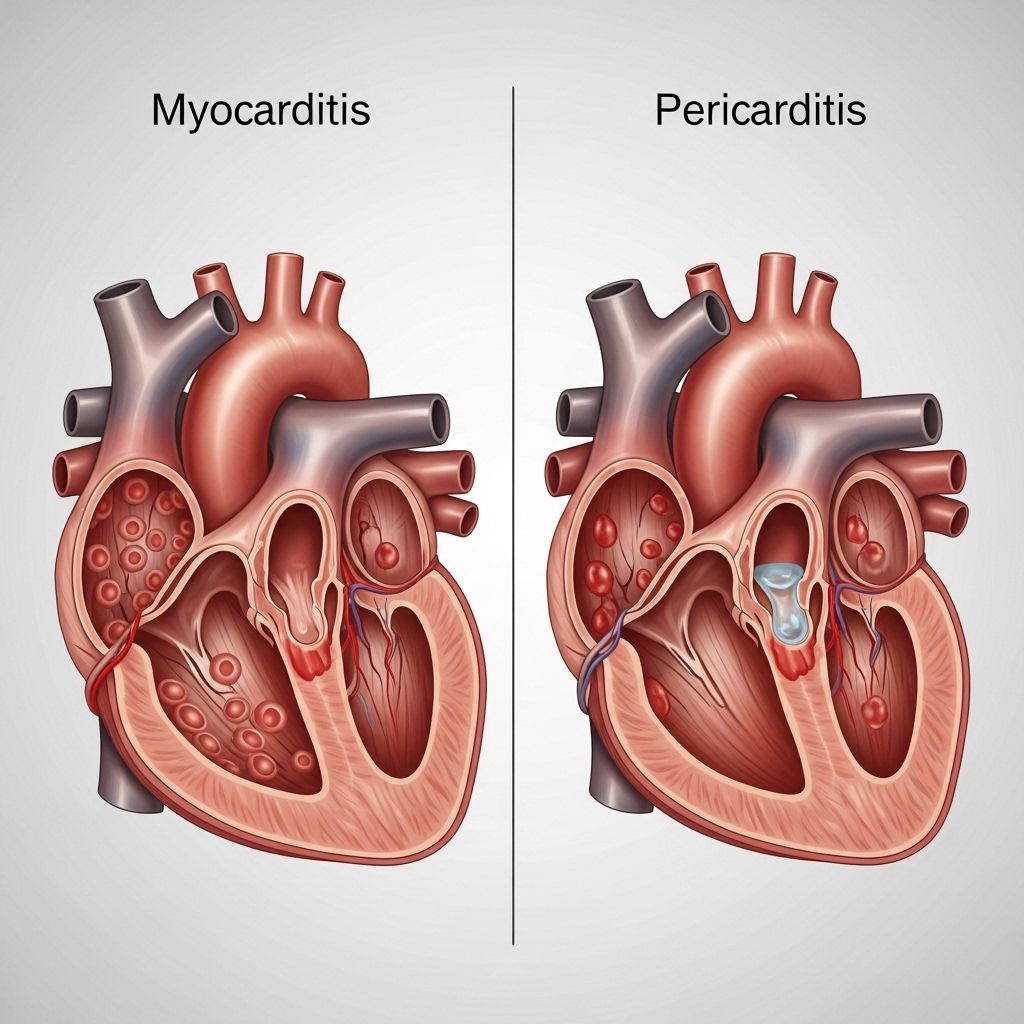
Myocarditis and pericarditis are two inflammatory heart conditions that, while closely related and sometimes overlapping, affect different parts of the heart and often manifest with similar symptoms. Understanding their distinctions and similarities is crucial for timely diagnosis, effective treatment, and improved heart health outcomes.
Overview: What Are Myocarditis and Pericarditis?
Myocarditis refers to inflammation of the heart muscle itself (the myocardium), the thick muscular layer responsible for pumping blood throughout the body.
Pericarditis is inflammation of the pericardium, the thin, sac-like membrane that surrounds the heart and provides physical protection and lubrication.
- Myocarditis primarily interferes with the heart’s pumping ability and may reduce blood supply to organs.
- Pericarditis primarily affects the outer lining, which can lead to fluid accumulation and pressure around the heart.
Though these conditions are distinct, it is possible to experience both simultaneously—a condition known as myopericarditis or perimyocarditis.
Causes: How Do Myocarditis and Pericarditis Develop?
The causes of myocarditis and pericarditis are often similar, with viral infections being the most common source for both.
| Cause | Myocarditis | Pericarditis |
|---|---|---|
| Viral infections | Common | Common |
| Bacterial infections | Possible | Possible |
| Fungal/protozoal infections | Rare | Possible |
| Autoimmune/rheumatologic diseases | Possible | Possible |
| Allergic/hypersensitivity reactions | Possible | Possible |
| Drug toxicity | Possible | Rare |
| Kidney failure | Rare | Possible |
| Chest trauma/heart surgery | Rare | Possible |
| Post-pericardiotomy syndrome | Rare | Possible |
| Radiation to chest | Rare | Possible |
| Kawasaki disease (children) | Possible | Possible |
| Vaccination (incl. COVID-19 mRNA vaccines) | Rare | Rare |
| Other inflammatory conditions | Possible | Possible |
Key points:
- Viruses remain the most frequent cause worldwide (e.g. enteroviruses, adenovirus, SARS-CoV-2).
- Autoimmune conditions and certain medications can trigger both diseases.
- Rare associations have been linked to vaccines, including mRNA COVID-19 vaccines.
- Physical trauma to the chest or the aftermath of surgery may cause pericarditis in particular.
Symptoms: Recognizing Each Condition
Myocarditis and pericarditis present with overlapping symptoms, making diagnosis challenging without further evaluation.
Common Symptoms of Both
- Chest pain (often sharp, stabbing, or pressure-like)
- Fever
- Fatigue and overall malaise
- Shortness of breath
- Heart palpitations (irregular heartbeats)
- Rapid pulse
- Low blood pressure (in severe cases)
- Nausea or vomiting
- Dizziness or fainting
- Abdominal pain
Specific Features and Differences
| Feature | Myocarditis | Pericarditis |
|---|---|---|
| Chest Pain | Dull or pressure-like; may worsen with physical activity | Sharp, stabbing; worsens with deep breathing, coughing, or lying down; may improve when sitting up |
| Shortness of breath | Common, often with exertion | Can occur, especially if fluid collects around the heart |
| Palpitations | Common, especially with arrhythmias | Possible |
| Edema (swelling) | Possible, in severe or chronic cases | Less common |
| Pain relief when sitting up/leaning forward | Rare | Characteristic |
| Back/shoulder pain | Occasional | Possible, especially under shoulder blades |
| Dry cough, sore throat | Possible, depending on cause | Possible |
| Recurrent symptoms | Rare, unless ongoing inflammation | Possible (acute, recurrent, or chronic forms) |
The symptoms can rapidly appear and sometimes mimic those of other cardiac conditions such as a heart attack, especially with pericarditis.
Diagnosis: How Are These Conditions Detected?
Physicians typically use a combination of patient history, physical examination, and diagnostic tests to differentiate myocarditis from pericarditis.
- Physical exam: Listening for friction rub (indicative of pericarditis), or abnormal heart sounds.
- Electrocardiogram (ECG): Reveals characteristic patterns related to inflammation or arrhythmias.
- Echocardiogram: Uses ultrasound waves to assess heart muscle function and detect fluid around the heart.
- Blood tests: Checked for markers of inflammation, infection, and cardiac enzymes (to detect heart muscle injury).
- Cardiac MRI: Very helpful for visualizing inflammation in the myocardium or pericardium.
- Chest X-ray: May show heart enlargement or fluid accumulation.
- Biopsy: Rare, but can confirm myocarditis if diagnosis remains unclear or the case is severe.
Types and Courses: Acute and Chronic Presentations
Pericarditis can be acute, recurrent, incessant, or chronic:
- Acute: Lasts less than three weeks; symptoms develop quickly.
- Recurrent: Recurs after four to six weeks with no symptoms in between.
- Incessant: Lasts 4–6 weeks but not more than three months, without resolution of symptoms.
- Chronic constrictive: Lasts more than three months; can cause gradual progression of symptoms due to persistent inflammation or scarring.
Myocarditis may range from mild and self-limiting to severe and rapidly progressive, sometimes leading to heart failure or dangerous arrhythmias if extensive damage occurs.
Complications: What Are the Risks?
- Heart failure: Most common in severe or untreated myocarditis; less common in pericarditis unless there is significant fluid or scarring.
- Arrhythmias: Both conditions can disrupt normal heart rhythm.
- Pericardial effusion: Fluid buildup around the heart, more typical of pericarditis.
- Cardiac tamponade: Life-threatening compression due to fluid, a rare severe complication of pericarditis.
Treatment: How Are Myocarditis and Pericarditis Managed?
The treatment for myocarditis and pericarditis depends on severity, underlying cause, and risk of complications. These conditions often improve with prompt treatment.
General Approaches
- Rest: Essential for recovery and reducing cardiac stress.
- Anti-inflammatory medications: Such as NSAIDs (ibuprofen) are typically first-line for pericarditis, used cautiously in myocarditis.
- Colchicine: May be prescribed for persistent or recurrent pericarditis.
- Corticosteroids: Sometimes used if symptoms do not respond to standard anti-inflammatory drugs or if underlying autoimmune disease is present.
- Treat underlying cause: Such as antibiotics for bacterial infection, antiviral drugs, or immunosuppressants for autoimmune conditions.
- Heart medications: Beta-blockers, diuretics, or ACE inhibitors may be used for heart failure or arrhythmia management.
- Hospitalization: Required for severe cases, persistent chest pain, arrhythmias, or if complications like heart failure develop.
Most people fully recover, especially when cause is viral and treated early. Some rare cases may require advanced treatments like immunoglobulin therapy or devices such as pacemakers.
Emergency Warning Signs
Seek immediate medical attention if you experience:
- Severe or worsening chest pain
- Difficulty breathing, fainting, or unexplained dizziness
- Rapid or irregular heartbeat
- Swelling of legs, abdomen, or new onset fatigue
Prompt intervention can be critical in preventing complications.
Prevention and Outlook
Many cases of myocarditis and pericarditis are difficult to prevent because they are linked to common viral infections or autoimmune triggers. Still, individuals can reduce risk by:
- Practicing good hygiene to minimize infections
- Managing chronic health conditions (like autoimmune diseases)
- Avoiding known medications or toxic exposures that have previously caused a reaction
- Staying up to date with vaccinations as recommended by your doctor
The prognosis for myocarditis and pericarditis is usually favorable with appropriate treatment, though recurrence is possible, especially for pericarditis. Long-term cardiac monitoring may be required in severe or complex cases.
What Is Myopericarditis?
Myopericarditis describes inflammation affecting both the myocardium and the pericardium simultaneously. Symptoms can be a blend of both chest pain types, breathlessness, palpitations, and fatigue. Treatment resembles that for myocarditis and pericarditis individually, but close monitoring is necessary because of potentially increased risk for complications like heart failure or pericardial effusion.
Frequently Asked Questions (FAQs)
Q: How can you tell the difference between pericarditis and a heart attack?
While both can cause chest pain, pericarditis classically causes sharp pain that worsens with deep breathing or lying down and improves when you lean forward. Heart attack pain is more often crushing or pressure-like and does not change with position or breathing. Only a doctor, using ECG and imaging, can reliably distinguish between the two in an emergency situation.
Q: Is myocarditis or pericarditis more dangerous?
Both can be serious, but myocarditis is generally considered more dangerous since it directly affects the heart’s pumping muscle and can lead to heart failure or life-threatening arrhythmias. However, severe pericarditis can also be life-threatening if complications like cardiac tamponade develop.
Q: Does COVID-19 increase the risk of myocarditis or pericarditis?
Yes. Both conditions are more common following SARS-CoV-2 infection, especially myocarditis. Rarely, both have been reported after COVID-19 mRNA vaccination, but the risk from the infection itself is higher than from vaccines.
Q: Can children get myocarditis or pericarditis?
Yes. Children and adolescents can develop either condition, particularly after viral illness or as complications of diseases like Kawasaki disease. Prompt medical attention is required due to potential for severe complications.
Q: What is the long-term outlook after recovery?
Most people recover fully with proper diagnosis and treatment. Some may experience recurrent episodes or require ongoing cardiac monitoring, especially if heart function was significantly affected during the acute illness.
Key Takeaways
- Myocarditis affects the heart muscle; Pericarditis affects the heart’s outer membrane.
- Symptoms often overlap: chest pain, fever, fatigue, palpitations, and shortness of breath.
- Main causes are viral infections, but trauma, autoimmune conditions, and medications also play a role.
- Most cases resolve with prompt, proper treatment. Severe complications are rare but possible.
- Any new chest pain or unexplained symptoms require immediate medical evaluation.
References
- https://www.myocarditisfoundation.org/myocarditis-vs-pericarditis-myopericarditis/
- https://www.healthline.com/health/heart-health/myocarditis-vs-pericarditis
- https://www.topdoctors.co.uk/medical-articles/pericarditis-and-myocarditis-what-s-the-difference/
- https://www.myocarditisfoundation.org/how-to-recognize-acute-pericarditis-vs-a-heart-attack/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3555652/
- https://www.childrenshospital.org/conditions/myocarditis-pericarditis
- https://my.clevelandclinic.org/health/diseases/17353-pericarditis
- https://thecurbsiders.com/curbsiders-podcast/431-myocarditis-and-pericarditis
Read full bio of medha deb












