Myocarditis: Symptoms, Causes, Diagnosis, and Treatment
Learn about myocarditis, its causes, risk factors, symptoms, complications, recovery, and answers to frequently asked questions.
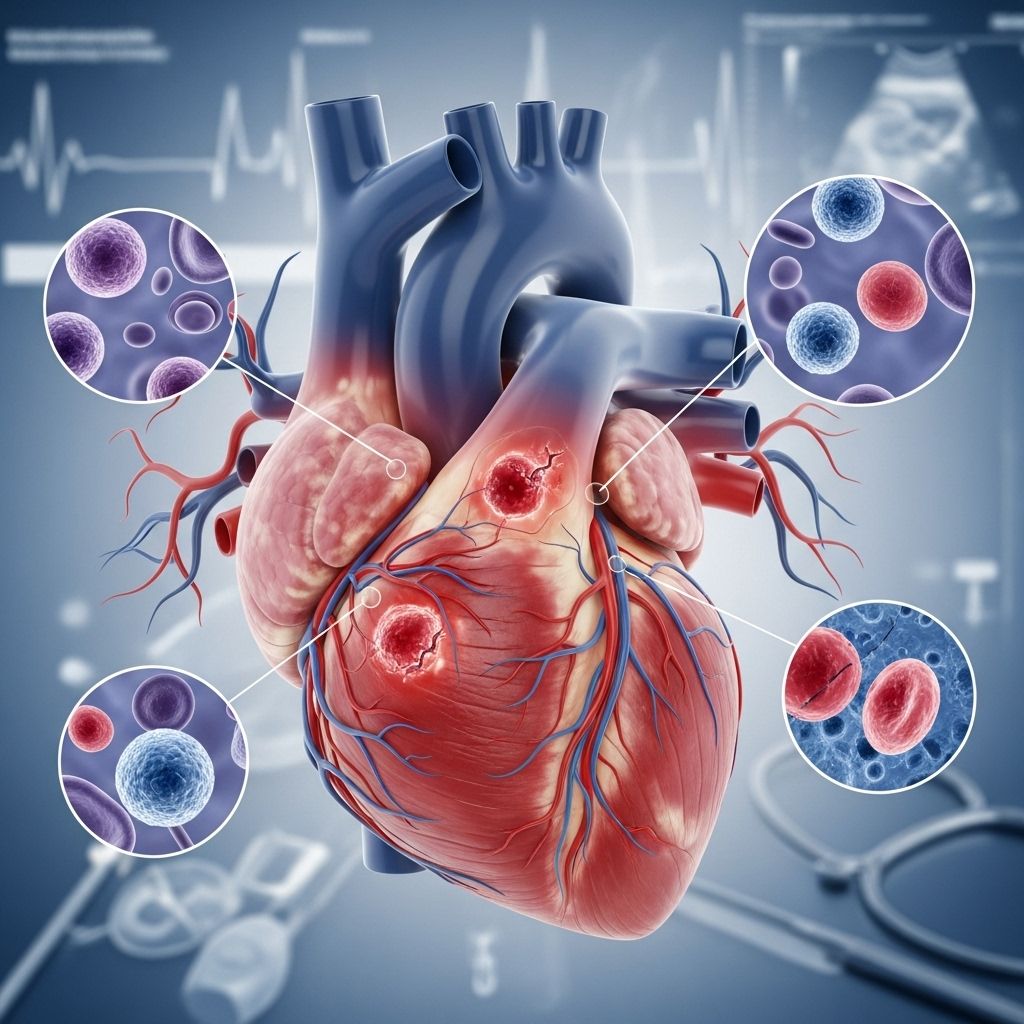
Myocarditis is a medical condition where the muscle tissue of the heart—called the myocardium—becomes inflamed. This disease affects people of all ages and can cause a range of symptoms from mild chest pain to severe heart complications. In some cases, myocarditis resolves without long-term effects, but in others, it may lead to chronic heart problems or even sudden cardiac death. Early recognition, appropriate treatment, and careful management are essential for a positive outcome.
What Is Myocarditis?
Myocarditis refers to the inflammation of the heart muscle, reducing the heart’s ability to pump blood effectively. This inflammation can result from infections, immune system reactions, or exposure to toxic substances and certain medications.
- The heart muscle (myocardium) becomes inflamed.
- May impair heart contractility and electrical conduction.
- Can be acute (sudden onset) or chronic (persistent/long-lasting).
The severity of myocarditis varies widely. Some people experience barely any symptoms, while others develop life-threatening complications.
How Common Is Myocarditis?
Myocarditis is relatively rare overall, but risk varies by age, health status, and recent infections. Its true prevalence is difficult to determine because many mild cases resolve without diagnosis, while severe ones often come to medical attention.
Symptoms and Signs of Myocarditis
Myocarditis can present with a variety of symptoms, which may develop suddenly (acutely) or progress over time. The severity and type of symptoms often depend on the degree of inflammation and underlying cause.
Common Symptoms in Adults
- Chest pain (may mimic a heart attack)
- Shortness of breath (at rest or during activity)
- Fatigue or general weakness
- Heart palpitations (rapid or irregular heartbeat)
- Swelling in the legs, ankles, or feet (edema)
- Dizziness or fainting spells
- Flu-like symptoms (headache, body aches, fever, sore throat)
Symptoms in Children
- Difficulty breathing or rapid breathing
- Chest pain
- Unexplained tiredness or lethargy
- Palpitations or fainting episodes
- Fever or irritability
Not all cases present with symptoms; some people discover they have myocarditis during routine health checks or investigations for other conditions.
When to Seek Medical Attention
If you experience unexplained chest pain, rapid or irregular heartbeat, or sudden difficulty breathing, seek emergency medical help immediately, as these can be life-threatening.
Causes of Myocarditis
There are several known causes of myocarditis. It is most frequently triggered by infections, but noninfectious causes are also recognized.
- Viral infections: The most common cause globally. Viruses such as Coxsackievirus B, adenovirus, parvovirus B19, and more recently, SARS-CoV-2 (COVID-19).
- Bacterial infections: Less common, but certain bacteria can inflame the heart muscle.
- Fungal and parasitic infections: Rare, but possible in immunocompromised individuals or those living in endemic areas.
- Immune and autoimmune diseases: Disorders causing the immune system to attack the body’s own tissues, e.g., lupus or giant-cell myocarditis.
- Medications and toxins: Certain cancer drugs, antibiotics, or exposure to heavy metals and illicit drugs can trigger myocarditis.
- Allergic or hypersensitivity reactions: Sometimes, an allergic response to a drug can cause heart inflammation.
Myocarditis and COVID-19
COVID-19, caused by coronavirus SARS-CoV-2, has increased awareness of myocarditis. While COVID-19 is primarily a respiratory illness, studies show it can impact other organs, including the heart.
- SARS-CoV-2 may infect heart muscle cells directly, especially via specific cellular receptors.
- The body’s immune response to the virus can inadvertently damage healthy heart tissue.
- Low oxygen levels (hypoxia) from severe COVID-19 may also contribute to myocarditis.
Data from large health databases shows that people with COVID-19 are roughly 16 times more likely to develop myocarditis compared to those without COVID-19 infection.
| Population | Incidence per 100,000 |
|---|---|
| People with COVID-19 | 150 |
| People without COVID-19 | 9 |
Certain pre-existing health conditions—such as hypertension, diabetes, and pre-existing heart disease—further increase risk when COVID-19 and myocarditis coincide.
Types of Myocarditis: Acute vs. Chronic
Acute myocarditis describes a sudden onset of symptoms, often resolving within a few weeks to a month after treatment. This is the most common presentation.
Chronic myocarditis refers to persistent or relapsing symptoms, sometimes caused by ongoing immune system activity or related to autoimmune diseases. This form may require longer-term management and can be more difficult to treat.
What Are the Risk Factors?
Certain factors increase the likelihood of developing myocarditis. These include:
- Recent viral infections (especially in children and young adults)
- Autoimmune diseases (e.g., lupus, rheumatoid arthritis)
- Immunosuppression (from disease or medications)
- Exposure to certain toxins or drugs
- History of allergic reactions to medications
How Is Myocarditis Diagnosed?
Doctors use a combination of clinical assessment, diagnostic tests, and imaging to confirm myocarditis and rule out other causes of symptoms.
- Medical history and physical examination: Identify symptoms, possible exposures, and risk factors.
- Blood tests: Reveal signs of inflammation, infection, or heart muscle damage (such as elevated troponin levels).
- Electrocardiogram (ECG/EKG): Measures heart electrical activity and may show arrhythmias or other abnormalities.
- Echocardiogram: Uses ultrasound to visualize heart function and detect swelling or reduced pumping ability.
- Cardiac MRI: Provides detailed pictures of heart muscle and inflammation patterns.
- Chest X-ray: May show an enlarged heart or fluid in the lungs.
- Endomyocardial biopsy: In some cases, a small sample of heart tissue is taken to confirm diagnosis under a microscope.
Treatment Options for Myocarditis
Treatment depends on the severity and underlying cause of myocarditis. The primary goals are to reduce heart inflammation, address the root cause, and manage symptoms or complications.
- Supportive care: Rest, oxygen, and heart monitoring to reduce stress on the heart.
- Medications:
- Anti-inflammatory drugs (like NSAIDs or corticosteroids, in some cases)
- Standard heart failure therapies (ACE inhibitors, beta-blockers, diuretics, etc.)
- Antivirals or antibiotics only if a specific infection is identified
- Medications to control arrhythmias
- Advanced interventions: Mechanical circulatory support (ventricular assist devices) or heart transplant in severe, nonresponsive cases
Recovery and Outlook
Recovery from myocarditis is highly individual and depends on severity, underlying cause, and how quickly it is treated. For many, symptoms resolve within a few weeks with appropriate care.
- About half of those diagnosed recover in 2–4 weeks, but some may face a longer recovery.
- Ongoing monitoring is needed, as heart function can deteriorate or improve over time.
- People are typically advised to avoid strenuous exercise for 3–6 months to reduce the risk of complications.
- Even after heart function recovers, some patients may need to remain on medications to prevent recurrence.
Possible Complications of Myocarditis
Some cases of myocarditis can cause significant and lasting heart damage, leading to serious complications including:
- Arrhythmia: Abnormal heart rhythms ranging from too fast, too slow, or irregular.
- Cardiomyopathy: Weakening of the heart muscle, leading to reduced blood pumping capability.
- Heart failure: The heart is unable to adequately supply blood to meet the body’s needs.
- Heart attack: Myocarditis can cause clots or blockages, increasing the risk of a heart attack.
- Sudden cardiac death: Especially in young adults, though rare; myocarditis has been implicated in a notable percentage of unexplained sudden deaths.
Prompt diagnosis, supportive treatment, and regular monitoring greatly reduce the risk of serious or fatal outcomes.
Can Myocarditis Happen Again?
Recurrence is possible, especially if the underlying cause remains or if there is a genetic predisposition. The risk of recurrence after an initial episode varies, generally estimated at 3–10% per year for symptomatic patients with imaging or biopsy findings. People who experienced left ventricular dysfunction should continue medication even after recovery, as stopping treatment can heighten the risk of recurrent heart failure.
Can You Prevent Myocarditis?
- Good hand hygiene and avoidance of close contact with sick individuals lower the risk of viral infections.
- Vaccinations can help prevent illnesses known to trigger myocarditis (influenza, COVID-19, etc.).
- Safe medication use—informing your doctor about drug allergies and reporting any side effects promptly.
- Avoid illicit drugs and limit alcohol, as these can harm the heart muscle.
Living With and Managing Myocarditis
- Regular follow-up with a cardiologist.
- Adhering to prescribed medications and activity restrictions.
- Monitoring for symptoms of heart failure or arrhythmia (such as weight gain, increased swelling, palpitations, or chest pain).
- Maintaining a balanced, heart-healthy diet.
Frequently Asked Questions (FAQs)
What is myocarditis?
Myocarditis is the inflammation of the myocardium—the muscular layer of the heart. This condition can impact the heart’s ability to pump blood and may lead to chest pain, shortness of breath, fatigue, or electrical conduction disturbances.
How do you know if you have myocarditis?
The only way to confirm myocarditis is through a combination of clinical assessment, blood tests, imaging, and in rare cases, biopsy. Symptoms such as unexplained chest pain, irregular heartbeats, or shortness of breath should prompt medical evaluation.
Can myocarditis happen without symptoms?
Yes. Some people, particularly in mild or early cases, may not notice symptoms. These cases are sometimes detected incidentally during workup for unrelated issues.
Is myocarditis contagious?
The heart inflammation itself is not contagious, but the underlying infectious cause (such as a virus or bacteria) can be transmitted from person to person.
Can exercise make myocarditis worse?
Yes. Physical activity can strain an inflamed heart and increase the risk of arrhythmias or other complications. Exercise restriction is typically recommended for several months following diagnosis.
How is myocarditis treated?
Most cases are treated with supportive care, medications to reduce inflammation, and management of heart function. Severe cases may need advanced therapies or procedural intervention.
Are children at risk for myocarditis?
Yes. Children can develop myocarditis, often following viral infections. Symptoms can include shortness of breath, fainting, unexplained fatigue, or fever. Prompt evaluation is critical.
Takeaway
Myocarditis is an important cause of cardiac symptoms and complications across all age groups. With early recognition, proper management, and ongoing care, most people recover well. However, being aware of the signs, risks, and when to seek medical help remains essential for the best outcomes.
References
- https://www.healthline.com/health/heart-disease/myocarditis
- https://www.ama-assn.org/public-health/chronic-diseases/what-doctors-wish-patients-knew-about-myocarditis
- https://www.mayoclinic.org/diseases-conditions/myocarditis/symptoms-causes/syc-20352539
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5814110/
- https://www.healthline.com/health/heart-disease/viral
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7199677/
- https://www.mountsinai.org/health-library/diseases-conditions/myocarditis
- https://www.cdc.gov/mmwr/volumes/70/wr/mm7035e5.htm
- https://www.bhf.org.uk/informationsupport/conditions/myocarditis
Read full bio of Sneha Tete












