Myocardial Fibrosis: Causes, Symptoms, Diagnosis, and Management
Explore the complexities of myocardial fibrosis, its causes, signs, diagnosis, treatments, and long-term outlook.
Everything You Need to Know About Myocardial Fibrosis
Medically reviewed by cardiovascular specialists. Authored by expert health journalists.
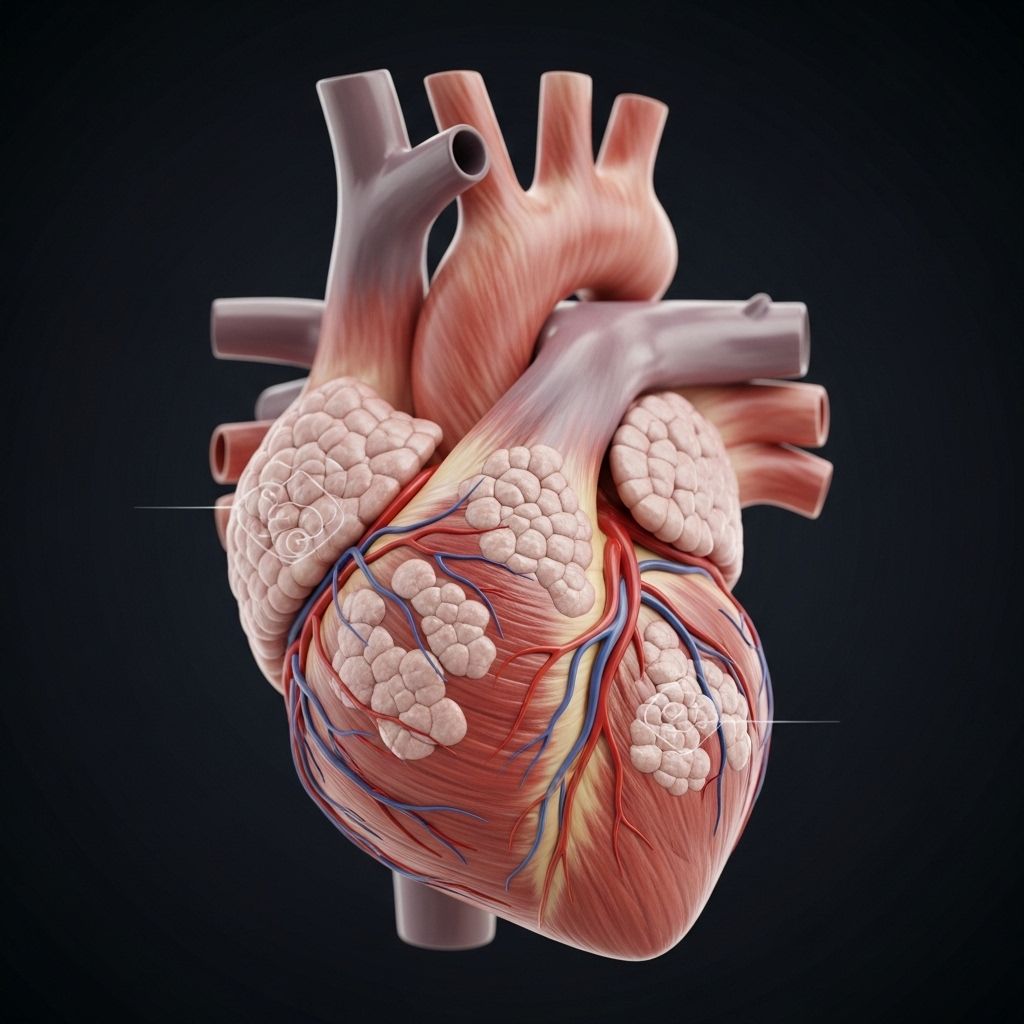
Myocardial fibrosis is a heart condition characterized by the accumulation of scar tissue in the heart muscle. While this process is sometimes the body’s way to heal after injury, it can also disrupt normal heart function, leading to major health issues such as heart failure. In this comprehensive guide, you’ll discover the mechanisms, causes, symptoms, diagnostic approaches, and the latest treatment perspectives on myocardial fibrosis.
What is Myocardial Fibrosis?
Myocardial fibrosis refers to scarring of the heart muscle (myocardium) that results from either acute (sudden) or chronic (long-term) injury to the heart. ‘Fibrosis’ means scar tissue formation, and ‘myocardial’ refers to the heart’s muscular wall. Scar tissue lacks the elasticity and contractility of healthy cardiac muscle, impacting the heart’s ability to pump efficiently.
- Scar tissue replaces normal heart muscle cells after injury.
- Unlike healthy muscle, scar tissue cannot contract or conduct electrical signals properly.
- Significant fibrosis can contribute to heart failure and increases the risk of life-threatening arrhythmias.
Types of Myocardial Fibrosis
There are several forms of myocardial fibrosis, categorized by their causes and patterns of tissue scarring:
- Replacement (focal) fibrosis: Scar tissue forms at a specific site of cell death, such as after a heart attack.
- Interstitial (diffuse) fibrosis: More widespread, with scarring distributed between viable muscle fibers, often resulting from chronic stress or systemic conditions.
- Reactive fibrosis: The heart reacts to a persistent abnormal load, like chronic high blood pressure, by developing protective scar tissue.
Common Symptoms of Myocardial Fibrosis
Because the development of myocardial fibrosis is often gradual, symptoms might not appear until the condition has advanced or until the heart’s ability to function is significantly impaired. Common symptoms include:
- Shortness of breath, especially during exertion or while lying flat.
- Fatigue or decreased ability to exercise.
- Chest pain (angina), especially after physical activity.
- Heart palpitations—feelings of rapid, pounding, or irregular heartbeat.
- Swelling in the legs, ankles, or feet (edema).
- Occasionally, fainting spells (syncope) or sudden dizziness.
Sometimes, mild fibrosis may not cause noticeable symptoms but can still carry a risk for heart rhythm disturbances and long-term heart function decline.
Causes and Risk Factors for Myocardial Fibrosis
Myocardial fibrosis represents the final common pathway of many cardiac and systemic conditions. The major causes and contributors are:
Myocardial Infarction (Heart Attack)
The most prevalent cause is a heart attack (myocardial infarction). When blood supply to a portion of the heart muscle is blocked, muscle cells die and scar tissue forms in their place. According to the Centers for Disease Control and Prevention (CDC), about 805,000 people in the United States have a heart attack each year. The more severe the heart attack, the greater the area of fibrosis.
Pressure Overload
Conditions that increase pressure inside the heart force the muscle to work harder, eventually causing reactive fibrosis. Key causes include:
- High blood pressure (hypertension)
- Aortic stenosis (narrowing of the aortic valve)
- Pulmonary arterial hypertension
- Pulmonary valve stenosis
Volume Overload
When the heart is overloaded with excess blood volume (often due to leaky heart valves or heart failure), this can also trigger fibrosis:
- Aortic regurgitation: Blood leaks backward through the aortic valve.
- Mitral regurgitation: Blood leaks backward through the mitral valve.
- Chronic heart failure: Increases pressure and volume inside the heart chambers.
Genetic and Inherited Conditions
Certain genetic disorders predispose individuals to heart muscle damage and subsequent fibrosis. These include:
- Hypertrophic cardiomyopathy: A condition characterized by thickened heart muscle.
- Fabry disease: A rare genetic disorder affecting fat metabolism, including the heart.
- Pompé disease: A metabolic condition causing buildup of a complex sugar (glycogen) in organs, including the heart.
Toxicity and Medications
- Chemotherapy drugs can sometimes damage heart tissues, leading to scarring.
- Environmental chemicals that disrupt hormone levels (such as BPA, as shown in animal studies) may also contribute to fibrosis.
Inflammation
- Infectious causes, such as certain viruses or bacterial infections, can lead to myocarditis, which can heal with scar formation.
- Sarcoidosis: An inflammatory disease that can involve the heart and cause patchy fibrosis.
How is Myocardial Fibrosis Diagnosed?
Diagnosing myocardial fibrosis requires a combination of clinical evaluation, risk factor assessment, and advanced imaging or laboratory techniques. Many cases are discovered incidentally, while investigating symptoms suggestive of heart failure or following a previous heart attack.
- Medical history review: Assessment of prior heart attacks, valve disease, family history, and risk factors for hypertension or genetic heart diseases.
- Physical examination: Checking for signs of heart failure such as swelling, rapid heartbeat, or abnormal heart sounds.
- Electrocardiogram (ECG): May detect arrhythmias or previous silent heart injury.
- Echocardiogram (ultrasound of the heart): Evaluates the size, thickness, pumping ability, and motion of the heart muscle.
- Cardiac MRI: Allows direct visualization and quantification of scar tissue in the heart walls. This is the most sensitive imaging test for detecting myocardial fibrosis.
- Biopsy: In rare cases, a heart tissue sample may be taken to analyze the extent and type of fibrosis directly.
- Blood tests: May detect markers associated with heart muscle stress or injury.
| Diagnostic Tool | Role in Diagnosing Fibrosis |
|---|---|
| Electrocardiogram | Detects arrhythmias and indirect signs of injury |
| Echocardiogram | Reveals heart structure and function; suggests areas of muscle weakness |
| Cardiac MRI | Directly images fibrosis for precise measurement |
| Heart Biopsy | Confirms diagnosis and rules out other causes |
Current Treatment Strategies for Myocardial Fibrosis
Treating myocardial fibrosis requires addressing its underlying cause whenever possible. While there is currently no cure that reverses existing scar tissue, treatments aim to prevent more fibrosis, improve heart function, and manage symptoms.
Treating the Underlying Cause
Many therapies are tailored to treat the primary disease leading to fibrosis:
- For heart attack survivors, controlling cholesterol and blood pressure helps reduce further risk.
- People with valve disease may need surgical repair or replacement.
- Heart failure is managed with medications, lifestyle changes, and in some cases, advanced therapies like cardiac resynchronization or transplantation.
Medications
- ACE inhibitors and angiotensin receptor blockers (ARBs) help reduce cardiac stress and slow fibrosis progression.
- Beta-blockers decrease the heart’s workload and risk of abnormal rhythms.
- Aldosterone antagonists may reduce further scarring in some patients.
Lifestyle Modifications
- Maintaining a healthy diet (low in salt and fat).
- Regular physical activity, supervised by a health professional.
- Quitting smoking and limiting alcohol intake.
- Weight management and blood sugar control for those with diabetes.
Emerging and Experimental Therapies
- Research continues into medications and gene therapies targeting the molecular mechanisms of fibrosis.
- Some anti-fibrotic agents used in other diseases are under investigation for cardiac use.
- Novel biomarkers and imaging technologies are being developed to detect fibrosis earlier and monitor treatment response.
Long-Term Outlook and Prognosis
The outlook for people with myocardial fibrosis depends on many factors, including:
- The amount and location of scar tissue
- Underlying heart function before fibrosis development
- The presence of other medical conditions like diabetes, high blood pressure, or genetic diseases
- Timeliness and effectiveness of treatment
Large areas of fibrosis increase the risk for heart failure and rhythm disturbances; however, appropriate treatment and lifestyle modifications can significantly improve quality of life and may slow or prevent worsening of symptoms. Ongoing research aims to identify better strategies to detect, prevent, and reverse fibrosis in the future.
Frequently Asked Questions (FAQs) about Myocardial Fibrosis
Q: Can myocardial fibrosis be reversed?
Currently, there is no widely available treatment that can completely remove scar tissue from the heart. Some data suggest that treating the underlying cause (e.g., valve replacement in aortic stenosis) may result in partial regression of fibrosis. Ongoing research is focused on developing therapies targeting the fibrotic process.
Q: How serious is myocardial fibrosis?
Myocardial fibrosis can significantly affect heart function and increase the risk of heart failure, arrhythmias, and other severe complications. Larger or more diffuse scars are associated with higher risk.
Q: What is the main difference between fibrosis and heart disease?
Fibrosis refers specifically to the formation of scar tissue. Heart disease is a broader term encompassing various conditions affecting the heart, including those that may lead to fibrosis.
Q: Is myocardial fibrosis hereditary?
Some forms of myocardial fibrosis have a genetic basis, especially when related to inherited conditions like hypertrophic cardiomyopathy, Fabry disease, or Pompe disease. Most cases, however, are not directly inherited but result from acquired heart injuries, such as heart attacks.
Q: Can myocardial fibrosis be prevented?
The best prevention involves minimizing risk factors for heart injury, such as controlling high blood pressure, avoiding smoking, managing diabetes, and maintaining heart-healthy lifestyle habits.
Key Takeaways
- Myocardial fibrosis is scarring of the heart muscle, most commonly seen after heart attacks or in chronic heart conditions.
- Early detection and control of heart disease risk factors play a critical role in prevention.
- While current treatments cannot reverse existing scars, they can prevent further progression and greatly improve quality of life.
- Ongoing research continually improves our understanding and management of this condition.
If you have concerns about your heart health or symptoms described here, consult a qualified healthcare provider for personalized evaluation and treatment.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5299507/
- https://www.ahajournals.org/doi/10.1161/circresaha.115.306565
- https://www.healthline.com/health/heart-disease/myocardial-fibrosis
- https://www.ahajournals.org/doi/10.1161/circimaging.108.842096
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12112327/
- https://www.healthline.com/health/heart/cardiomyopathy-vs-heart-failure
Read full bio of medha deb












