Mitral Valve Prolapse (MVP) and Heart Murmur: Understanding the Connection
Explore the relationship between mitral valve prolapse and heart murmurs, their detection, symptoms, and available treatments.
Mitral valve prolapse (MVP) is a common heart valve condition that is often first detected due to the presence of a heart murmur, a unique sound heard during a heartbeat. While MVP can range from harmless to severe, understanding its symptoms, detection, and available treatments is crucial for heart health management.
About Mitral Valve Prolapse (MVP)
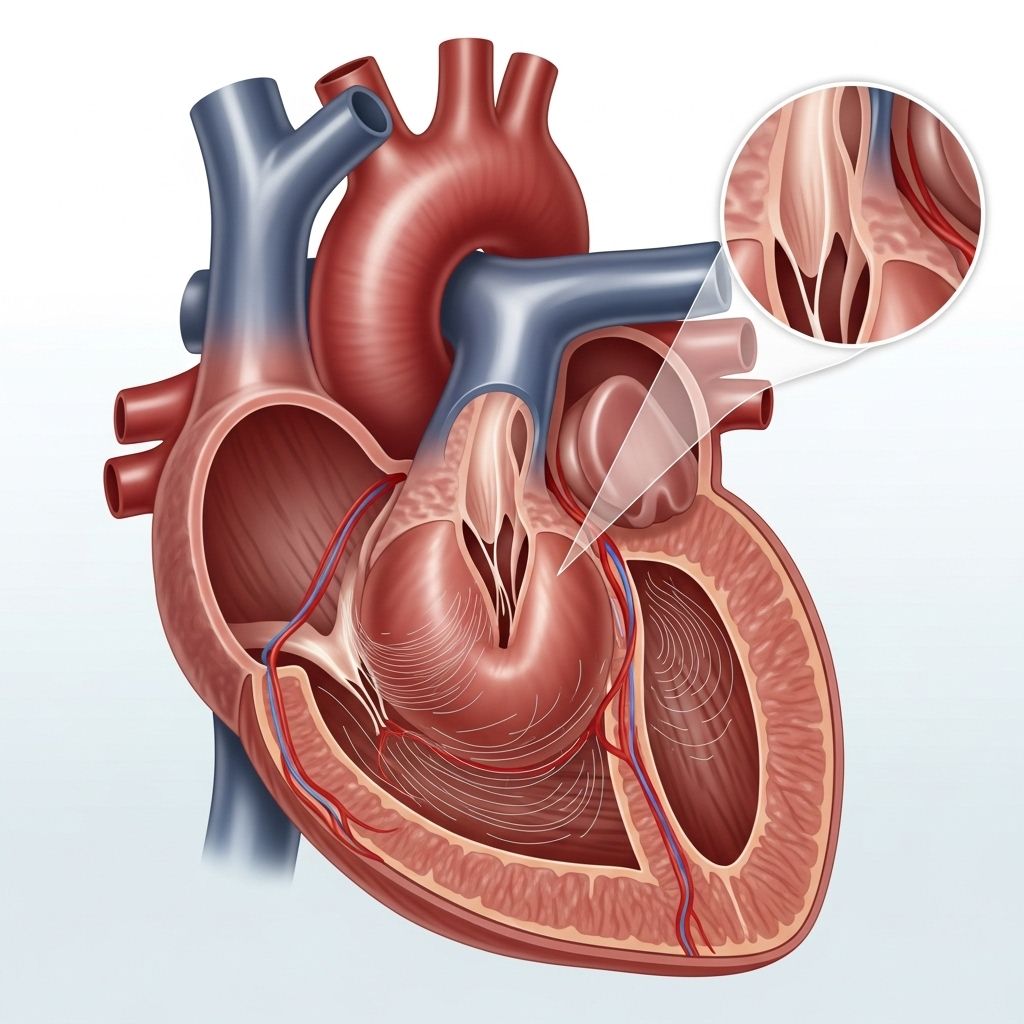
The mitral valve is a two-leaflet valve situated between the left atrium and the left ventricle of the heart. It ensures smooth, one-way blood flow as the heart contracts and relaxes. Problems arise when these flaps—also called leaflets—fail to close properly, causing them to bulge (prolapse) back into the left atrium during contraction. This can allow blood to leak backward, a condition known as mitral regurgitation.
The condition is known by several other names, including:
- Click-murmur syndrome
- Barlow’s syndrome
- Floppy valve syndrome
- Balloon mitral valve
MVP is the most common heart valve abnormality in developed countries, affecting around 2% of the U.S. population. Evidence suggests MVP is more common in women and often runs in families, indicating a genetic component. It can also be associated with inherited connective tissue disorders such as Marfan syndrome. Sometimes, MVP results from heart infections or cardiovascular disease, but often, the exact cause remains undetermined.
Is MVP Dangerous?
For most people, MVP is a mild condition that may never cause symptoms or require treatment. Many discover they have MVP during routine exams. However, in some cases, especially when significant mitral regurgitation is present, it can lead to complications such as:
- Heart rhythm problems (arrhythmias)
- Increased risk of infective endocarditis (heart infection)
- Heart failure, if regurgitation is severe
Therefore, correct diagnosis and monitoring are essential.
The Connection Between MVP and Heart Murmur
A healthy heart produces a steady, predictable sound with each beat. A heart murmur refers to any abnormal sound—typically a swishing or whooshing noise—heard during a heartbeat, caused by turbulent or irregular blood flow.
MVP can cause two main audible features:
- Murmur: Blood leaking back into the atrium (regurgitation) creates a swishing sound.
- Click: The floppy valve leaflets can snap or ‘click’ as they close—in combination with the murmur, this gives rise to the term click-murmur syndrome.
| Sound | Origin | Clinical Significance |
|---|---|---|
| Mid-systolic click | Valve leaflets snapping during closure | Suggests MVP |
| Late systolic murmur | Backflow of blood into left atrium | Indicates mitral regurgitation due to MVP |
Notably, the murmur’s timing and character may change depending on body position and blood flow, highlighting the importance of skilled clinical assessment.
How Are MVP and Murmurs Detected?
Often, MVP is first detected during a routine physical examination when a healthcare provider hears a murmur or click with a stethoscope. However, many individuals have mild MVP with no clear symptoms. Symptoms, when present, can include:
- Fatigue
- Shortness of breath, especially with exertion
- Heart palpitations (sensation of irregular or rapid heartbeat)
- Lightheadedness or dizziness
- Headache
- Chest pain (not always related to exertion)
- Abnormally low blood pressure when standing (orthostatic hypotension)
To confirm MVP and assess its severity, your healthcare provider may order the following tests:
- Physical Exam: Listening for the classic click-murmur and evaluating for extra sounds between heartbeats.
- 2D Echocardiography: This non-invasive imaging uses sound waves to provide a real-time view of heart valves and chambers, revealing the movement and closure of the mitral valve.
- Electrocardiography (ECG): Detects arrhythmias or other electrical abnormalities related to MVP.
- Cardiac MRI: Detailed images to assess valve structure and function.
- Cardiac Catheterization: Occasionally used for deeper investigation, especially prior to surgery.
- Stress Test/Stress Echocardiogram: Evaluates heart function and valve competency under exertion.
Symptoms Warranting Medical Advice
Seek timely evaluation if you experience:
- Persistent or unexplained chest pain
- Severe shortness of breath
- Sudden, rapid, or irregular heartbeat episodes
- Fainting spells or frequent dizziness
Treatment of MVP and Heart Murmur
Not everyone with MVP needs treatment. In many cases, the condition is mild and does not affect daily activities or prognosis.
Treatment is recommended when significant mitral regurgitation or bothersome symptoms are present. Strategies may include:
- Observation and Lifestyle Management: Routine screening echo, healthy diet, avoiding excessive stimulants, and regular checkups if symptoms are mild and regurgitation is absent or trivial.
- Medications:
- Beta-blockers: For palpitations or chest discomfort.
- Diuretics: To reduce fluid overload in moderate to severe regurgitation.
- Antiarrhythmics: For heart rhythm disturbances.
- Antibiotics: May be considered in high-risk situations to prevent infective endocarditis (usually not required just for MVP alone anymore).
- Procedures and Surgery:
- If MVP results in severe regurgitation, surgical repair or replacement of the mitral valve may be necessary.
- Minimally invasive techniques may be an option for suitable candidates.
Innovations in imaging and surgical repair have improved outcomes for those needing intervention. Regular monitoring is key to detecting changes that would make surgery beneficial before heart function is compromised.
Outlook and Living With MVP
Most people with MVP live normal, healthy lives, especially when there is no or only mild regurgitation. Regular follow-ups and lifestyle choices — such as maintaining a healthy weight, managing blood pressure, and avoiding tobacco — can optimize heart health and reduce risk of complications.
For patients with moderate to severe regurgitation or symptoms, collaborative care with a cardiologist and timely management help prevent progression to heart failure or other risks.
Frequently Asked Questions (FAQs)
Q: What causes mitral valve prolapse?
A: MVP most often results from abnormally stretchy mitral valve leaflets (myxomatous degeneration). It can have a genetic origin and is seen more frequently in people with connective tissue disorders such as Marfan syndrome.
Q: Can MVP be cured?
A: There is no cure for MVP, but most people do not need treatment. In cases where regurgitation is severe, surgical repair or replacement restores normal valve function.
Q: Are all heart murmurs due to MVP dangerous?
A: No, many heart murmurs are ‘innocent’ and harmless. MVP murmurs require attention when associated with symptoms or significant regurgitation.
Q: Can exercise worsen MVP?
A: Mild, symptom-free MVP typically does not restrict activity. However, your doctor may recommend limiting strenuous exercise if you have significant valve leakage or arrhythmias.
Q: Do I need antibiotics before dental procedures if I have MVP?
A: Current guidelines usually do not recommend routine antibiotics for dental or minor procedures solely for MVP patients, unless other risk factors are present.
Q: How often should I see my doctor if I have MVP?
A: Frequency depends on your individual condition. Many people with mild MVP need checkups every 1–2 years; those with more severe leakage may need more frequent monitoring.
Key Takeaways
- Mitral valve prolapse is common, sometimes inherited, and usually benign.
- A heart murmur, often a clue to diagnosis, results from turbulent blood flow due to incomplete valve closure.
- MVP is diagnosed by a combination of physical examination and imaging techniques like echocardiography.
- Treatment is tailored to symptoms and degree of regurgitation; most cases need only observation.
- Patients should follow healthy lifestyle habits and consult their doctor if new symptoms develop.
Staying proactive with heart health, understanding symptoms, and regular follow-up are the foundation for living well with MVP.
References
- https://www.healthline.com/health/heart/mvp-murmur
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9509210/
- https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-mitral-valve-prolapse
- https://www.healthline.com/health/heart-murmurs
- https://www.ncbi.nlm.nih.gov/books/NBK470288/
- https://www.medicalnewstoday.com/articles/318455
- https://www.merckmanuals.com/professional/cardiovascular-disorders/valvular-disorders/mitral-valve-prolapse-mvp
- https://www.droracle.ai/articles/28068/murmur-heared-in-mitral-valve-prolapse-
- https://www.ahajournals.org/doi/10.1161/circulationaha.113.006702
Read full bio of medha deb












