What to Avoid If You Have Mitral Valve Prolapse: Risks, Lifestyle Changes, and Management
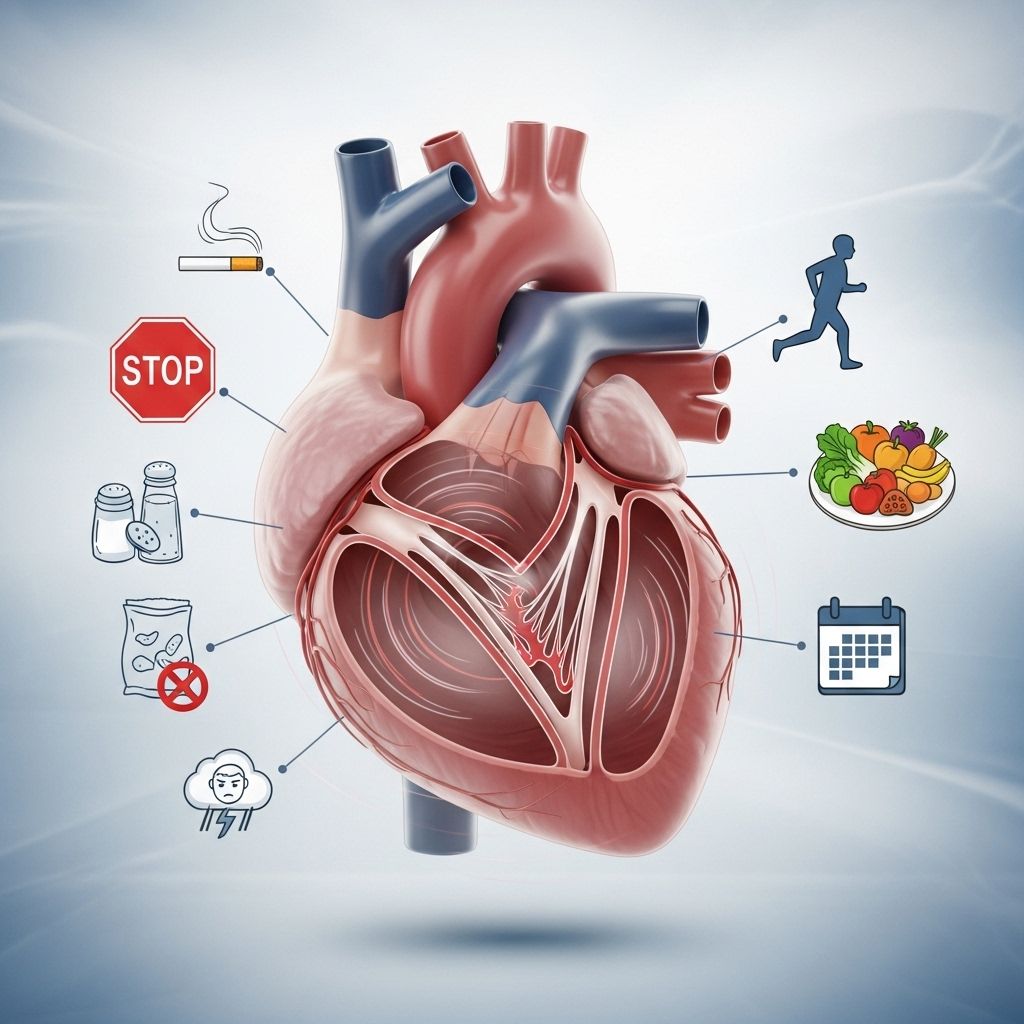
Managing mitral valve prolapse involves avoiding triggers, making informed lifestyle choices, and understanding potential complications.
What Should I Avoid If I Have Mitral Valve Prolapse?
Mitral valve prolapse (MVP) is a structural abnormality where the valve between the heart’s left atrium and left ventricle doesn’t close smoothly, sometimes causing blood to leak backward (regurgitation). While most individuals with MVP have no noticeable symptoms or complications, adopting sound lifestyle habits and avoiding certain triggers is essential for optimal heart health and to minimize risks of related problems.
Understanding Mitral Valve Prolapse
Mitral valve prolapse (MVP) occurs when the mitral valve’s flaps bulge or prolapse into the left atrium during contraction. This may cause a murmur and, sometimes, mitral regurgitation. The condition is present in about 2-3% of the population, often more commonly in women, and may run in families due to genetic predisposition. In most cases, MVP is harmless and doesn’t affect day-to-day health; only some need treatment.
Symptoms of MVP
- Palpitations (rapid or irregular heartbeat)
- Chest discomfort
- Fatigue
- Dizziness
- Shortness of breath, especially during activity or when lying flat
- Cough, sometimes related to exertion
Complications Can Occur in Severe Cases
- Mitral regurgitation (backflow of blood)
- Enlarged left atrium or ventricle
- Arrhythmias (abnormal heart rhythms)
- Heart failure (rare)
- Increased risk for stroke or heart attack due to blood clot formation
General Guidelines: What to Avoid with MVP
For most people, MVP doesn’t require drastic lifestyle changes. However, understanding what can aggravate your condition or increase your risk for complications is crucial. Specific foods, substances, and activities are best avoided or approached with caution.
1. Foods and Beverages to Avoid
Certain foods and drinks may trigger symptoms in people with MVP, especially those prone to palpitations or dizziness. Dietary changes can help manage your heart rhythm and maintain overall wellness.
- Caffeine: Coffee, energy drinks, caffeinated sodas, and tea can trigger or worsen palpitations and anxiety.
- Alcohol: Excessive consumption may increase risk of arrhythmia and is best limited or avoided.
- High-sodium foods: Excessive salt can increase blood pressure and exacerbate fluid retention, complicating any existing heart problems.
- Sugary foods and simple carbohydrates: Sudden spikes in blood sugar can affect heart rhythm, energy levels, and overall cardiovascular health.
- Processed foods: These often contain unhealthy fats, sodium, and preservatives that may increase heart disease risk.
Individuals may discover additional personal triggers. Keeping a food diary can help identify foods that worsen symptoms.
2. Medications and Supplements: Use with Caution
If you have MVP, always discuss any over-the-counter or prescription medications with your healthcare provider, specifically:
- Stimulants: Meds containing pseudoephedrine (found in some cold and flu medications) or amphetamines may worsen palpitations.
- Some herbal and dietary supplements: Caffeine-like compounds, weight-loss products, or any product affecting heart rate/rhythm should be used with caution.
Always ask your provider before starting a new medication or supplement.
3. Activities and Lifestyle Choices to Avoid or Modify
Most people with MVP can lead a normal, active life. However, it’s important to avoid extremes and exercise prudently:
- Intense endurance sports: Marathon running, extreme cycling, or other strenuous activities may increase heart stress in those with severe mitral regurgitation or arrhythmias.
- Sedentary lifestyle: Avoid inactivity. Gentle, regular exercise helps support heart function.
- Dehydration: Lack of fluids can lower blood pressure and trigger symptoms like dizziness or palpitations.
- Prolonged standing, sudden position changes: These may precipitate dizziness or fainting.
4. Smoking and Recreational Drugs
- Tobacco and vaping: Smoking increases cardiovascular risk, worsens overall heart health, and may aggravate symptoms.
- Recreational drugs: Especially stimulants (cocaine, amphetamines) should be strictly avoided due to their potential for increasing arrhythmia risk.
5. Stress Reduction and Mental Health Support
MVP is often associated with anxiety and panic attacks. Managing stress can reduce symptoms, especially palpitations, dizziness, or chest discomfort. Techniques include:
- Mindfulness and relaxation exercises
- Yoga or gentle stretching
- Cognitive-behavioral therapy (CBT) for anxiety disorders
- Regular sleep schedule
6. Avoiding Infection Risks: Dental and Medical Precautions
Though rare, some people with MVP and significant regurgitation may be at increased risk for endocarditis (an infection of the heart valve). Preventive steps include:
- Maintaining good oral hygiene
- Seeking prompt medical care for symptoms of infection (fever, chills, unexplained fatigue)
- Informing dentists and providers of your MVP diagnosis before procedures
- Discussing the need for preventive antibiotics before invasive procedures (generally not necessary unless severe regurgitation is present)
7. What If You Have Severe Mitral Valve Prolapse?
While most MVP cases are mild, those with severe regurgitation, arrhythmias, or symptoms that interfere with daily life require further management:
- Regular cardiac check-ups and echocardiograms
- Close monitoring for signs of heart failure or atrial fibrillation
- Careful use of medications (e.g., beta-blockers for arrhythmia, anticoagulants for risk of clot)
- Surgical options including mitral valve repair or replacement in advanced cases
Summary Table: Common Triggers and Risks
| Category | What to Avoid | Why? |
|---|---|---|
| Food/Beverages | Caffeine, excess alcohol, high-sodium, processed foods | Triggers palpitations, increases blood pressure, worsens symptoms |
| Medications/Supplements | Stimulants, weight loss pills, energy drinks | Can provoke arrhythmias, unsafe for heart health |
| Activities | Extreme endurance sports, dehydration, inactivity | May increase stress on the heart, cause dizziness/fatigue |
| Lifestyle Habits | Smoking, recreational drugs | Increase risk of heart problems, contribute to arrhythmias |
| Stress/Infection | Poor dental hygiene, unmanaged anxiety, ignoring infections | Can increase risk for endocarditis, arrhythmia, severe symptoms |
Key Steps for Managing MVP
- Follow up regularly with your healthcare provider, including echocardiograms and other heart imaging as recommended.
- Take prescribed medications precisely as instructed. Beta-blockers may help with palpitations; anticoagulants may be needed if you develop atrial fibrillation.
- Alert medical and dental professionals to your MVP diagnosis before procedures.
- Adopt balanced nutrition, aiming for whole grains, fresh fruits and vegetables, lean protein, and healthy fats.
- Exercise moderately and regularly unless your provider advises otherwise.
- Maintain excellent oral hygiene to prevent infection risk.
- Monitor your symptoms, and seek immediate care for chest pain, severe shortness of breath, or signs of stroke (numbness, sudden confusion).
FAQs About Mitral Valve Prolapse
Q: Is mitral valve prolapse a serious condition?
A: In most people, MVP is mild and does not affect health or longevity. Severe cases with substantial regurgitation or arrhythmias may require more attention, treatment, or surgery.
Q: Can I participate in sports or exercise with MVP?
A: Generally, yes. Moderate exercise is encouraged. Avoid strenuous endurance activities only if you have severe symptoms or arrhythmias; always consult your cardiologist first.
Q: Do I need to take antibiotics before dental procedures?
A: For most MVP cases, antibiotics are not needed. In severe regurgitation, your provider may advise otherwise. Always inform your dentist and ask your physician.
Q: Are palpitations dangerous?
A: Occasional palpitations are usually harmless in MVP. If they are frequent, accompanied by chest pain or dizziness, or new, let your doctor know immediately.
Q: Will I need surgery for MVP?
A: Only a small percentage require surgery, which is recommended for severe regurgitation, heart enlargement, heart failure, or persistent arrhythmias.
Q: What symptoms mean I should seek medical attention?
- Sudden severe chest pain
- Shortness of breath at rest
- Swelling in legs, feet, or abdomen
- Fainting or lightheadedness
- Signs of stroke (slurred speech, drooping face, weakness on one side)
If you experience any of these, seek prompt care.
Living Well with Mitral Valve Prolapse
A diagnosis of MVP should not prevent you from leading a full and active life. With the proper medical guidance and by avoiding known triggers (foods, medications, and activities that can provoke symptoms), most people remain asymptomatic and healthy. Partnering with your healthcare team, staying informed, and making smart lifestyle choices will help reduce the risk of complications and ensure the best possible outcomes.
Frequently Asked Questions (FAQs)
Q: Are there any long-term effects of MVP?
A: Most MVP cases remain stable and benign. However, some may progress to significant mitral regurgitation. Regular monitoring is key.
Q: Is MVP hereditary?
A: MVP can run in families. Genetic and connective tissue disorders play a role in some cases.
Q: Can MVP be prevented?
A: MVP itself often cannot be prevented, especially when it’s genetic. However, complications and symptom progression can be minimized with lifestyle management and regular medical care.
References
- https://www.heart.org/en/health-topics/heart-valve-problems-and-disease/heart-valve-problems-and-causes/problem-mitral-valve-prolapse
- https://www.healthline.com/health/mitral-valve-prolapse
- https://www.health.harvard.edu/heart-health/mitral-valve-prolapse-a-to-z
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5757046/
- https://www.healthline.com/health/mitral-valve-prolapse-symptoms
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6168064/
- https://www.ahajournals.org/doi/10.1161/JAHA.121.020919
- https://www.jeffersonhealth.org/conditions-and-treatments/mitral-valve-prolapse
Read full bio of Sneha Tete












