Microalbuminuric Diabetic Nephropathy: Symptoms, Diagnosis, and Treatment
Explore how microalbuminuria is linked to diabetic nephropathy, its symptoms, diagnosis steps, causes, risks, treatments, and prevention.
Microalbuminuria, or the presence of small but abnormal amounts of albumin in the urine, is an early clinical marker signaling the onset of diabetic nephropathy, a complication that impacts the kidneys of people with diabetes. This condition is particularly critical because kidney damage related to diabetes often develops silently, with little to no symptoms in early stages, yet it can progress to kidney failure if not identified and treated promptly.
What Is Microalbuminuria and Why Does It Matter in Diabetes?
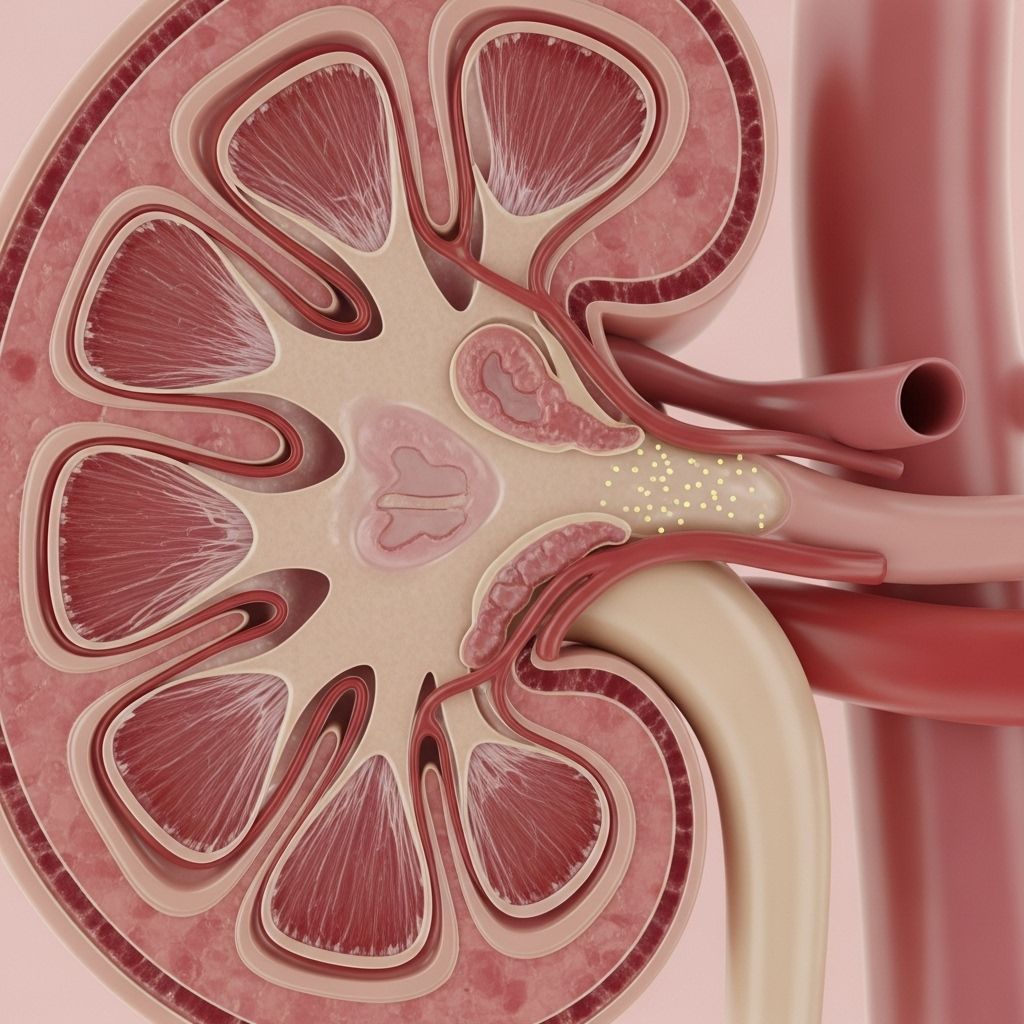
Albumin is a vital protein in the blood, integral for maintaining osmotic pressure and transporting various substances. Healthy kidneys prevent significant amounts of albumin from leaking into the urine. However, in the context of diabetes, persistently high blood sugar levels can damage the kidney’s filtering units (nephrons), leading to leakage of albumin into the urine—a condition known as microalbuminuria.
Microalbuminuria is considered a warning sign, indicating that kidney function is declining and the person with diabetes is at increased risk for developing diabetic nephropathy.
- Microalbuminuria refers to having a urine albumin level between 30–299 mg/g creatinine.
- Kidney damage progresses silently, often without obvious symptoms early on.
- About 40% of U.S. adults with diabetes develop kidney disease, making diabetes the most common cause of end-stage renal disease.
How Are Microalbuminuria and Diabetic Nephropathy Linked?
Diabetic nephropathy arises when the nephrons, the kidney’s filtering units, are damaged primarily due to persistently high blood sugar and high blood pressure. This results in the loss of their filtering ability, causing essential proteins like albumin to ‘leak’ into the urine.
Here’s how the process unfolds:
- High blood sugar damages both large and small blood vessels within the kidneys.
- This damage, along with high blood pressure, impairs nephron function.
- When impaired, the nephrons allow albumin and other proteins to pass into the urine, which would normally be retained in the bloodstream.
- Early on, microalbuminuria is often detected before overt kidney failure symptoms appear, thus serving as a crucial early marker for intervention.
Symptoms of Microalbuminuric Diabetic Nephropathy
Diabetic nephropathy typically progresses slowly. Most people experience no symptoms in early stages, making routine screening vital. As kidney function worsens and albumin levels in the urine increase, certain signs may appear. Later stage symptoms may also reflect the buildup of waste products due to failing kidneys.
- Foamy or bubbly urine
- Increased frequency of urination, especially at night
- Swelling (edema) around the eyes or in the feet, ankles, abdomen, or face
- Puffiness, especially in the morning
- Prolonged and unexplained fatigue (as the disease advances)
Since many symptoms are subtle or absent early on, the American Diabetes Association (ADA) recommends that:
- All people with type 2 diabetes undergo annual microalbuminuria screening starting at diagnosis.
- People with type 1 diabetes are screened annually beginning five years after their diagnosis.
How Is Microalbuminuric Diabetic Nephropathy Diagnosed?
The primary diagnostic tool is a urine albumin-creatinine ratio (ACR) test, which calculates the amount of albumin relative to creatinine (a waste product from muscles) in the urine. This test helps adjust for variations in urine concentration.
Diagnosis Process:
- A urine ACR value of 30 mg/g or higher is the threshold for microalbuminuria and an indicator for possible kidney disease.
- Values 300 mg/g or higher suggest overt albuminuria (macroalbuminuria), a more advanced stage.
- At least two abnormal results separated by at least three months are needed for a definitive diagnosis (to avoid false positives from temporary conditions).
- Testing is ideally performed in early morning urine samples for accuracy.
| Albumin/Creatinine Ratio (mg/g) | Risk Level |
|---|---|
| < 30 | Normal |
| 30–299 | Moderately Increased Risk |
| ≥ 300 | Severely Increased Risk (Overt Albuminuria) |
Persistent microalbuminuria is associated not only with kidney disease risk, but also with increased cardiovascular risk.
Treatment Options for Microalbuminuric Diabetic Nephropathy
Early detection and management can slow or even prevent disease progression. The main principles of treatment are controlling risk factors and preserving kidney function.
- Blood Sugar Management: Tight blood glucose control using diet, exercise, and medications helps reduce further kidney damage.
- Blood Pressure Control: Keeping blood pressure under 140/90 mmHg (or lower in some cases) is vital. ACE inhibitors and ARBs are often recommended for their protective effects on kidney health.
- Cholesterol Management: Statin therapy may be considered to lower cardiovascular risks.
- Dietary Adjustments: Reducing salt, managing protein intake (favoring plant over animal sources), and balancing fluids can lessen kidney workload.
- Avoiding Nephrotoxic Medications: Some pain relievers and contrast dyes can further injure kidneys and should be avoided or used with caution under physician guidance.
- Smoking Cessation: Quitting smoking decreases the rate of progression to kidney failure.
If progression occurs despite these measures, consultation with a nephrologist is recommended. In advanced stages, preparation for dialysis or transplant may become necessary.
What Causes Microalbuminuric Diabetic Nephropathy?
Both type 1 and type 2 diabetes can lead to diabetic nephropathy. Chronically high blood glucose levels, together with high blood pressure, directly damage the nephrons. Several other factors interplay to accelerate kidney damage:
- Genetics: Family history of diabetes or kidney disease increases risk.
- Poorly controlled blood sugar: Episodes of hyperglycemia, or elevated blood sugar, over extended periods are highly damaging.
- Hypertension (high blood pressure): Exerts excessive force on kidney blood vessels, speeding up damage.
- Obesity, high cholesterol, smoking, and sedentary life: All raise the risk of developing nephropathy and complicate diabetes management.
In rare cases, the presence of albumin in urine may be due to non-diabetic causes such as urinary infections or vigorous exercise.
Risk Factors for Developing Diabetic Nephropathy
- Duration of diabetes: The longer you have diabetes, the greater the risk.
- High blood pressure: Elevates stress on kidney filtering mechanisms.
- Poor blood sugar control: Persistent hyperglycemia causes cumulative damage.
- Family history: Genetics play a notable role.
- Obesity: Increases the risk and accelerates progression.
- High cholesterol: Contributes to vascular and kidney damage.
- Smoking: Accelerates kidney dysfunction.
Preventive Strategies
Proactive measures can substantially lower the incidence and progression of microalbuminuric diabetic nephropathy.
- Maintain optimized blood sugar levels through a combination of medical therapy, healthy eating, and regular exercise.
- Monitor and manage blood pressure to recommended target ranges.
- Prioritize annual screening for microalbuminuria as recommended by diabetes guidelines.
- Adopt a kidney-friendly diet low in salt, moderate in protein, and rich in plant-based foods.
- Avoid tobacco use.
- Achieve and maintain a healthy weight through balanced lifestyle choices.
- Minimize or avoid non-essential nephrotoxic medications and inform your healthcare provider about all medicines and supplements you take.
Outlook for People with Microalbuminuric Diabetic Nephropathy
The outlook for individuals diagnosed with early-stage diabetic nephropathy is significantly improved with timely and aggressive management. While the condition cannot always be reversed, it is often possible to slow or halt its progression, particularly with rigorous blood sugar and blood pressure control.
Left untreated, diabetic nephropathy can lead to:
- Chronic kidney disease (CKD)
- End-stage kidney disease (ESKD), requiring dialysis or a kidney transplant
- Increased risk of heart and vascular disease
Early detection through urine testing, lifestyle changes, and mediation compliance together offer the best pathway to preserving kidney and overall health in diabetes.
Frequently Asked Questions (FAQ)
What exactly is microalbuminuria?
Microalbuminuria means small but abnormal levels of albumin in the urine (30–299 mg/g creatinine), serving as an early sign of kidney filtration damage in diabetes.
Can microalbuminuria be reversed?
Microalbuminuria can sometimes be reduced or reversed, especially with prompt glucose and blood pressure control, often before severe kidney injury sets in.
How often should people with diabetes be screened for microalbuminuria?
The ADA recommends annual urinary albumin screening for all people with type 2 diabetes, and for those with type 1 diabetes starting five years after diagnosis.
Does microalbuminuria always mean kidney disease?
No. Temporary factors such as exercise, fever, or urinary tract infection may cause transient elevations. Persistent results over time are necessary for diagnosis.
What are the main risks if microalbuminuric diabetic nephropathy is left untreated?
Untreated cases may progress to chronic or end-stage kidney disease, with a high risk of cardiovascular complications—both require advanced, lifelong treatments.
Key Takeaways
- Microalbuminuria is a crucial early marker for diabetic nephropathy and overall kidney health in diabetes.
- Routine screening, good blood sugar and blood pressure control, and a healthy lifestyle are vital for prevention and management.
- Early intervention can lead to much better long-term outcomes and kidney preservation.
References
- https://www.healthline.com/health/diabetes/microalbuminuric-diabetic-nephropathy
- https://www.ncbi.nlm.nih.gov/books/NBK534200/
- https://medlineplus.gov/ency/article/000494.htm
- https://www.mayoclinic.org/diseases-conditions/diabetic-nephropathy/symptoms-causes/syc-20354556
- https://www.drugs.com/health-guide/diabetic-nephropathy.html
- https://www.aafp.org/pubs/afp/issues/2019/0615/p751.html
- https://phoenixchildrens.org/specialties-conditions/diabetic-nephropathy-kidney-disease
- https://diabetes.org/about-diabetes/complications/chronic-kidney-disease
Read full bio of Sneha Tete












