How Your Gut and Mental Health Are Connected: Insights on the Gut-Brain Axis
Explore how gut health intertwines with mental wellness and why your microbiome may shape mood, anxiety, and overall wellbeing.
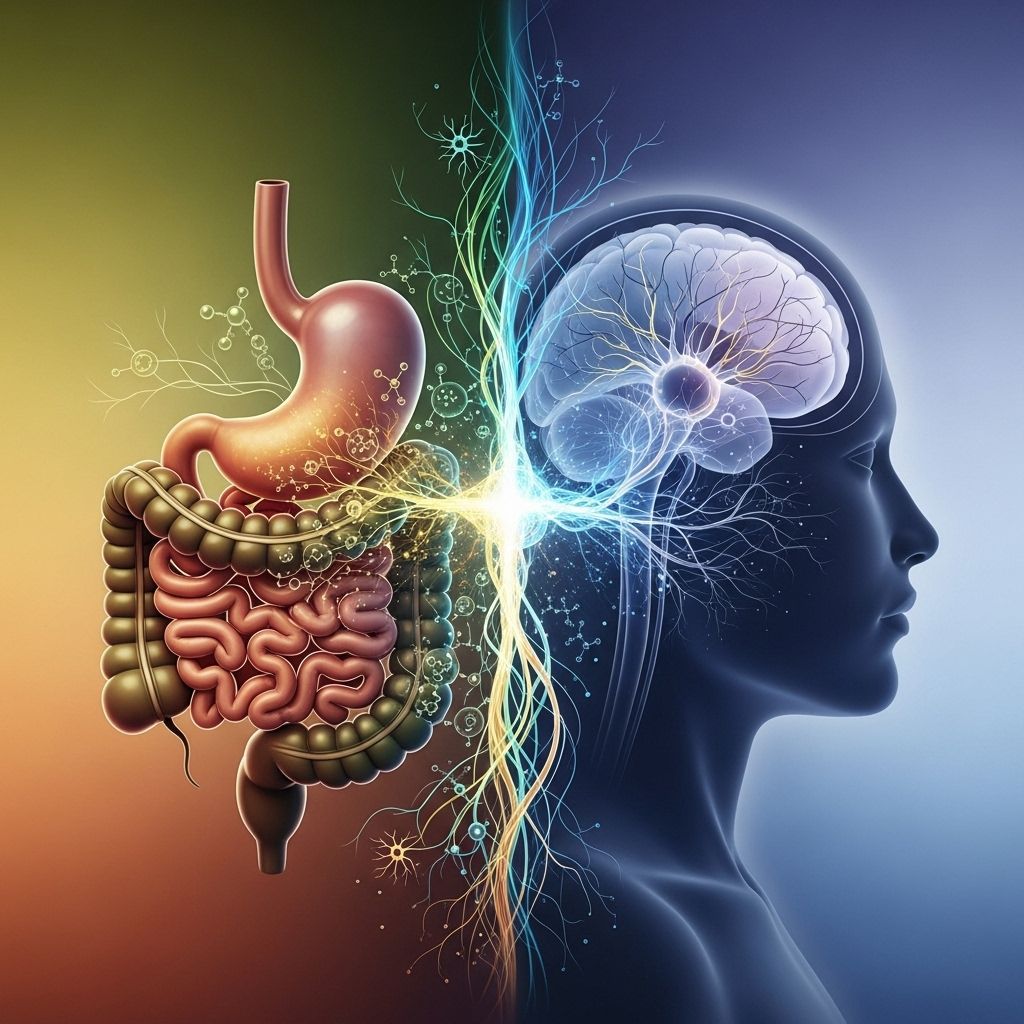
How Your Gut and Mental Health Are Connected
Your body is full of trillions of microbes, especially in your gut, and new science reveals they have surprising influence over your mental well-being. Researchers are unlocking the secrets of the gut-brain axis — the two-way link connecting your digestive system and your brain. This interplay affects not just your digestion, but also your mood, stress levels, and risk of mental health conditions like anxiety and depression.
Understanding the Gut-Brain Connection
The gut and brain are deeply connected in a network now referred to as the gut-brain axis. This communication system relies on a combination of:
- Nervous system signaling (via nerves like the vagus nerve)
- Hormonal signals
- Immune system interactions
- Chemicals produced by gut microbes
Messages transmitted along this axis flow both directions, meaning stress and emotional upheaval can influence digestion, while disruptions in gut health can directly affect your mental state.
How the Brain Affects the Gut
The most commonly recognized example is that emotional stress can trigger symptoms in the digestive tract, such as:
- Stomachaches
- Changes in appetite
- Nausea or “butterflies”
- Diarrhea or constipation
This effect isn’t only anecdotal. The nervous system in your gut (called the “enteric nervous system”) is so complex, it’s sometimes dubbed your “second brain.” Far from just passively receiving orders, your digestive system sends constant updates to your brain, largely via the vagus nerve and chemical messengers.
The Microbiome: Gut Bacteria’s Role in Mood
Inside your gut are trillions of bacteria, fungi, and viruses collectively known as the gut microbiome. These microbes don’t just influence digestion—they also produce chemicals and neurotransmitters vital for brain health. For example:
- Serotonin: About 90% of this mood-regulating neurotransmitter is produced in the gut.
- Dopamine: Some dopamine is also synthesized by gut bacteria, playing a role in reward and pleasure.
- Short-chain fatty acids: Produced by breakdown of dietary fiber, these compounds may reduce inflammation and support a healthy blood-brain barrier.
Disruptions in gut bacteria—sometimes called “dysbiosis”—have been linked with increased rates of mental health issues such as depression, anxiety, and even neurodevelopmental disorders.
The Science: Evidence for the Gut-Brain Axis
Research in recent years has deepened our understanding of the gut-brain connection:
- Studies in humans show that altered gut microbiota compositions often appear in people with major depression and anxiety disorders.
- Animal studies have found that swapping gut microbes between active and sedentary mice changes their behavior and dopamine levels.
- Large population analyses have shown that specific bacterial species are more (or less) abundant in people with depression or who score low on mental health surveys.
Bacteria and Mental Health: What the Research Shows
| Microbe | Linked Mental Health Effects |
|---|---|
| Eggerthella | Overgrowth associated with depression |
| Subdoligranulum | Reduced levels linked to depressive symptoms |
| Lactobacillus, Bifidobacterium | Higher levels linked to improved mood, lower anxiety |
| Bacteroides, Firmicutes (certain types) | Balance important for regulating stress and mental state |
These findings are strengthened by studies in large volunteer populations as well as clinical observations associating gut bacterial imbalances with different mental health conditions.
How Your Gut Affects Key Aspects of Mental Health
Stress, Anxiety, and the Gut
Many people notice that their digestion suffers during stressful times. But the relationship is not one-way—unhealthy gut microbiota can also worsen feelings of stress and anxiety. Some mechanisms include:
- Modulating levels of stress hormones (like cortisol)
- Altering immune system signals, which may increase inflammation linked to anxiety
- Reducing neurotransmitter production in the gut, limiting the brain’s supplies
For example, disruptions in the normal balance of gut bacteria have been shown to make mice, and possibly people, more vulnerable to stress-induced anxiety behaviors. Conversely, gut-friendly interventions like probiotics and certain dietary changes appear to lower anxiety in some studies.
Depression and Gut Health
Several studies suggest a clear association between lower microbial diversity or specific bacteria (like low *Subdoligranulum*) and depressive symptoms. In some cases, transplanting a healthy microbiome into animal models has led to rapid improvements in mood and behavior.
Diet quality appears especially important. Diets rich in:
- Vegetables and leafy greens
- Legumes and whole grains
- Fruits and nuts
- Healthy fats, especially omega-3s
are associated with a gut microbial profile linked to better mood and lower rates of depression and anxiety.
Gut Health and Cognitive Disorders
Researchers are exploring how gut health may affect the risk of conditions like Alzheimer’s disease and Parkinson’s. Some types of gut bacteria seem to encourage brain aging or inflammation, while others may have protective effects. While these discoveries are still developing, maintaining healthy gut diversity could support long-term cognitive health.
Bidirectional Impacts: How Mood Affects Your Gut
Not only does your gut affect your brain, but chronic mental health issues often appear alongside digestive symptoms. Examples include:
- IBS (Irritable Bowel Syndrome): Strongly associated with anxiety and depression
- Stomach ulcers: Linked to chronic stress
- Appetite changes: Occur with shifts in mental health (decreased in depression, increased in emotional eating)
Psychological distress can even alter gut motility, permeability (“leaky gut”), and the production of digestive hormones, further complicating both mental and physical health.
How to Support Gut and Mental Health
Although more research is needed, several practical steps show promise in supporting both gut and mental well-being:
- Eat a diverse, fiber-rich diet to promote healthy gut microbiota. Target multiple sources: vegetables, fruit, nuts, seeds, beans, whole grains.
- Include fermented foods such as yogurt, kefir, kimchi, sauerkraut, and miso for live beneficial bacteria.
- Limit ultraprocessed foods and excess sugar, which are linked to gut inflammation and unfavorable microbiome changes.
- Consider probiotics or prebiotic supplements, but consult with a healthcare professional to personalize your choice.
- Manage stress with mindfulness, meditation, regular exercise, or engaging hobbies.
- Sleep well: Chronic lack of sleep may disrupt your gut bacteria, worsening both physical and mental symptoms.
Other Approaches to Improve Gut-Brain Health
- Recent research supports exploring natural products (herbs, spices, plant polyphenols) for their gut-modulating effects and potential mental benefits.
- Some studies are investigating acupuncture and meditation as supportive options for nervous system and gut regulation.
Remember, gut health solutions are not one-size-fits-all. Genetic factors, current health status, medications, and even where you live may influence what works best for your unique microbiome and mental health needs.
Warning Signs of Gut-Mental Health Imbalance
Some clues that your gut health may be impacting your mental well-being include:
- Frequent digestive upset (bloating, gas, constipation, or diarrhea)
- Unexplained fatigue
- Changes in appetite or weight
- Persistent mood swings or irritability
- New or worsening anxiety or depression
If these symptoms are ongoing or worsening, talk to your healthcare provider. You may benefit from digestive health screening or a mental health assessment, especially if symptoms are affecting daily life.
When to Seek Help
While self-care and dietary strategies are helpful, professional support is essential when:
- You have severe or persistent digestive symptoms
- New or worsening depression or anxiety is interfering with life
- You have a history of eating disorders, severe mood instability, or major changes in health
- There is sudden, extreme alteration in bowel habits
Early intervention, with support from both mental health and GI specialists, can make a substantial difference.
Frequently Asked Questions (FAQs)
Can changing my diet improve my mental health?
Studies suggest that increasing fiber, plant foods, and healthy fats (especially omega-3s) can support the gut microbiome and improve mood in some people. Benefits vary, so lasting improvement may take time and individualized guidance.
What probiotic strains are most helpful for mood?
Certain strains, such as Lactobacillus and Bifidobacterium, have been studied for their ability to lower anxiety and support mental health. Always consult your healthcare provider before starting new supplements, especially if you have underlying conditions.
Is there a test for my gut-brain axis health?
Currently, there’s no single test. Comprehensive approaches may include digestive health assessments, dietary reviews, and mental health screening to develop a personalized plan.
Can stress or depression cause gut symptoms?
Yes. Stress and mental health conditions often trigger or worsen gut symptoms due to the bidirectional nature of the gut-brain axis.
Is the connection between gut health and the brain just a new trend?
The gut-brain connection is supported by decades of research, but methods for optimizing this link are still being refined. What is clear: gut and brain health are deeply entwined, and a holistic approach benefits both mind and body.
References
- Population-based and clinical studies connecting gut bacteria to depression and anxiety .
- Biological pathways: up to 90% of serotonin is produced in the gut .
- Research on dietary fiber, fermented foods, and polyphenols impacting the microbiome and mood .
References
- https://www.uclahealth.org/news/article/research-says-gut-brain-axis-plays-role-mental-health
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10384867/
- https://www.uchealth.org/today/improving-gut-health-improves-all-aspects-of-your-health/
- https://med.stanford.edu/news/insights/2025/03/gut-brain-connection-long-covid-anxiety-parkinsons.html
- https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5641835/
- https://mhanational.org/resources/gut-brain-connection/
Read full bio of medha deb












