Mental Health and Chronic Kidney Disease: Understanding the Hidden Burden
Chronic kidney disease profoundly impacts mental health, increasing the risk of anxiety, depression, and emotional distress.
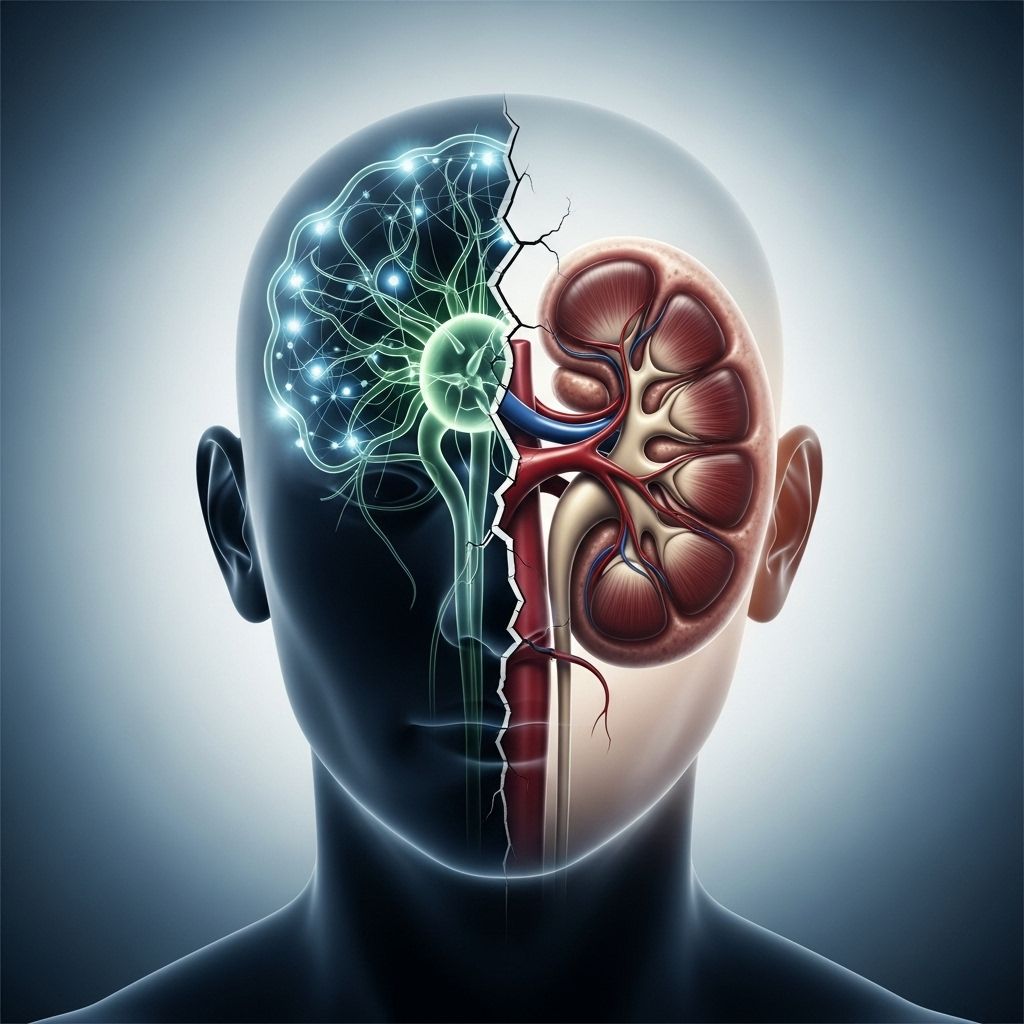
Chronic kidney disease (CKD) affects millions globally, causing lasting changes not only to physical health but also to emotional and mental well-being. The journey from diagnosis to ongoing management requires difficult lifestyle modifications, complex treatment decisions, and, in many cases, lifelong dialysis or transplantation. These stressors create a fertile ground for mental health issues, most notably depression and anxiety, which can hinder quality of life, self-care, and even clinical outcomes.
How Does CKD Impact Mental Health?
The relationship between chronic kidney disease and mental health is complex and mutually reinforcing. People with CKD experience high levels of psychological distress due to loss of physical and cognitive functioning, the burden of treatment, and changes in relationships, work, and overall lifestyle. Mental health disorders—particularly depression and anxiety—are significantly more common in people with CKD compared to the general population. For some, the emotional burden is as significant as the medical challenges they face.
- Depression prevalence: Occurs in up to 39% of people on dialysis and 25% of kidney transplant recipients.
- Anxiety prevalence: Affecting 19% as a disorder and 43% as elevated symptoms among CKD patients.
- Suicidal thoughts: CKD patients have higher rates of suicidal ideation and suicide attempts than the general population.
- Cognitive and emotional changes: CKD increases risk for cognitive impairment and dementia, which can further impact emotional health.
Why Are Mental Health Issues So Common with CKD?
There are several factors that make CKD a high-risk condition for mental health challenges:
- Physical symptoms and limitations: Fatigue, pain, and other CKD symptoms drain energy and motivation, making daily tasks and social participation harder.
- Treatment burden: Frequent medical appointments, treatments like dialysis, strict dietary restrictions, and complex medication regimens disrupt routines.
- Uncertainty about prognosis: The progressive nature of CKD causes anxiety about future disability, dependence, or even end-of-life issues.
- Social and occupational changes: Reduced work capacity and social isolation can lead to loss of identity, financial worries, and strained relationships.
Common Mental Health Conditions in CKD
Depression
Depression in CKD is not just a passing sadness—it’s a clinical disorder that can significantly affect daily life. Its symptoms can also overlap with those of kidney disease, making diagnosis harder.
- Persistent low or empty mood for most of the day
- Loss of interest or pleasure in almost all activities
- Major weight or appetite changes (increase or decrease)
- Sleep issues: insomnia or hypersomnia (too much sleep)
- Fatigue, low energy, and slowed movement or thinking
- Feelings of worthlessness, guilt, or hopelessness
- Diminished concentration, indecisiveness
- Recurring thoughts about death, suicidal ideation or attempts
Research indicates that depression can negatively impact treatment adherence, leading to missed medications, skipped dialysis sessions, and worse clinical outcomes. Untreated depression raises the risk of mortality and can lead to suicidal thoughts. Early identification and professional treatment (therapy, counseling, medication) can significantly improve both mental health and kidney outcomes.
Anxiety
Anxiety frequently coexists with CKD, presenting as persistent worry, panic attacks, restlessness, and fear. Stressors such as disease progression, possible dialysis, and uncertainty about the future contribute to high rates of anxiety disorders and elevated symptoms.
- Excessive fear about disease progression and health complications
- Obsessive thoughts about treatment, finances, family needs, and prognosis
- Panic attacks, rapid heartbeat, shortness of breath, and irritability
Other Emotional and Cognitive Effects
- Cognitive impairment: CKD increases risk of memory loss, difficulty concentrating, and even dementia.
- Stress: The emotional toll of managing a chronic disease can trigger ongoing feelings of stress for patients and caregivers alike.
- Suicidal ideation: Thoughts of self-harm, hopelessness, and suicide are sadly not uncommon when mental health symptoms go unaddressed.
Why Addressing Mental Health is Critical for CKD Patients
Tending to mental health is just as important as managing CKD’s physical symptoms. Poor mental health can lead to:
- Missed medical appointments and poor medication adherence
- Poorer physical outcomes and faster disease progression
- Greater use of healthcare resources and increased hospitalizations
- Higher mortality rates compared with CKD patients without psychological distress
Timely identification and proactive management of psychological symptoms can not only ease suffering but also enhance quality of life, boost treatment participation, and improve physical outcomes.
Recognizing Signs of Mental Health Challenges
For CKD patients, recognizing when sadness or worry becomes more than a passing feeling is crucial. Some signs that warrant attention include:
- Persistent negative thoughts (over two weeks or longer)
- Withdrawing from family, friends, or favorite activities
- Sleep problems: insomnia or excessive sleep
- Changes in eating habits (up or down)
- Physical complaints with no clear medical explanation
- Lack of interest, energy, or motivation
If these symptoms occur frequently, it may be time to speak with a healthcare provider. Supportive interventions exist and can make a meaningful difference.
Seeking Support and Treatment
Managing mental health alongside CKD often requires a team approach, including medical providers, mental health professionals, and loved ones. Treatment options may include:
- Counseling or therapy: Psychologists or counselors can help develop coping strategies and address emotional distress.
- Medication: If appropriate, antidepressants or anti-anxiety medication may be prescribed. Always discuss options with your nephrologist and mental health provider.
- Support groups: Peer support from others with CKD or similar experiences can reduce isolation and help with practical problem-solving.
- Mindfulness and stress reduction techniques: Meditation, deep breathing, and gentle exercise may help alleviate stress and improve mood.
- Involvement of caregivers: Caregiver stress is common and should be addressed through education, counseling, and respite care where possible.
When to Seek Immediate Help
If thoughts of self-harm or suicide appear, seek immediate help. Reach out to a trusted family member, friend, or therapist, or contact a crisis line for urgent support. The National Suicide Prevention Lifeline is available 24/7 (1-800-273-8255).
Strategies to Cope with CKD-Related Mental Health Challenges
- Stay connected: Maintain relationships with family and friends, even in small ways. Isolation worsens depression and anxiety.
- Set small, manageable goals: Focus on what you can control. Recognizing small wins can lift mood.
- Practice self-compassion: Accept that CKD brings real challenges, and avoid self-blame for emotional reactions.
- Communicate with your care team: Share concerns about emotional symptoms; mental health is a core part of your treatment.
- Engage in regular activities: Continue hobbies and interests as much as possible or find adaptations.
- Educate yourself: Learning about CKD and mental health empowers you to advocate for needed resources.
Mental Health Matters for Caregivers Too
Caregivers also face substantial emotional stress. Watching a loved one struggle with CKD, acting as a patient advocate, and managing treatment logistics all take an emotional toll. Caregivers are at increased risk for depression, anxiety, and burnout.
- Share responsibilities where possible.
- Seek social and professional support.
- Pay attention to personal health needs.
- When feeling overwhelmed, reach out to healthcare providers for resources and support.
Prevalence Table: CKD and Mental Health Challenges
| Condition | General Population | CKD Population | Impact on Health Outcomes |
|---|---|---|---|
| Depression | 8–12% | 25–39% | Poor treatment adherence; increased mortality |
| Anxiety | 10–15% | 19–43% | Hospitalization risk; day-to-day functioning impairment |
| Suicidal Ideation | Approx. 4% | Much higher; specific prevalence varies | Risk of suicide; requires urgent intervention |
| Cognitive impairment | 10–20% | Up to 40% | Impacts independence, safety, and management ability |
Professional Help and Resources
It is normal to feel overwhelmed by CKD and its management, but professional support exists. Mental health professionals, CKD support programs, and crisis resources can offer guidance and practical tools for recovery. Proactive steps can make a significant difference in the journey ahead.
- National Suicide Prevention Lifeline: 1-800-273-8255
- Kidney Disease Support Groups (contact local hospital or kidney association)
- Psychologist or social worker referrals via nephrology clinic
Frequently Asked Questions (FAQs)
Q: Why does CKD increase the risk of depression and anxiety?
Chronic illness, physical symptoms, frequent medical visits, dietary restrictions, and uncertain prognosis create a mental health burden for CKD patients, making depression and anxiety much more likely than in the general population.
Q: What should I do if I feel persistently sad or anxious with CKD?
Monitor your mood and reach out to your care team for help. Talking to a mental health professional, joining support groups, and connecting with loved ones are effective strategies. If suicidal thoughts occur, seek immediate crisis support.
Q: Are mental health symptoms treatable in CKD?
Yes, mental health conditions can be managed through therapy, medication, lifestyle support, and social networks. Treatment not only improves emotional wellbeing but also physical health outcomes and quality of life.
Q: Do caregivers of CKD patients also need mental health support?
Absolutely. Caregivers encounter high levels of stress and emotional strain. Support groups, counseling, and respite care can be invaluable.
Q: Is it normal to have emotional ups and downs with CKD?
Yes, it is normal to experience emotional highs and lows. However, frequent or severe depression and anxiety require professional attention for optimal health and safety.
Key Takeaways
- Chronic kidney disease is a serious medical condition—and a major risk factor for mental health challenges.
- Depression, anxiety, cognitive impairment, and stress are common among CKD patients and caregivers.
- Mental health symptoms can worsen CKD outcomes and reduce quality of life.
- Timely professional help, self-care strategies, and support systems can empower individuals and families to manage both CKD and emotional distress.
References
- https://academic.oup.com/ndt/article/38/10/2152/7005243
- https://www.kidneyfund.org/living-kidney-disease/mental-health-and-kidney-disease
- https://www.cdc.gov/pcd/issues/2025/24_0509.htm
- https://kidneycarepartners.org/mental-health-awareness-month-kidney-disease-and-mental-health/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9082446/
- https://www.kidney.org/kidney-topics/managing-your-emotions-while-living-kidney-disease
- https://www.nature.com/articles/s41598-024-57512-1
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9625106/
Read full bio of medha deb












