Understanding the Menstrual Cycle: Phases, Hormones, and Health
A comprehensive exploration of the menstrual cycle—phases, hormones, and its role in reproductive health.
The menstrual cycle is a cornerstone of female reproductive health. This regular, cyclical process prepares the body for potential pregnancy and encompasses complex interactions between hormones and reproductive organs. Recognizing how this cycle works is vital for understanding overall wellness and recognizing the signs of potential health concerns.
What is the Menstrual Cycle?
The menstrual cycle refers to the monthly sequence of physiological changes that occurs in the female reproductive system to prepare for a possible pregnancy. Every cycle, the body experiences hormonal fluctuations that orchestrate the maturation and release of an egg, readiness of the uterine lining for implantation, and, if no pregnancy occurs, the shedding of that lining. The visible part of this cycle—menstruation or a “period”—is only a portion of the overall process.
- Cycle Length: Typically considered from the first day of one period to the first day of the next, lasting on average 24-38 days.
- Menstruation: The shedding of the uterine lining, lasting usually 3-7 days.
- Purpose: Prepares the body for fertilization and pregnancy each month.
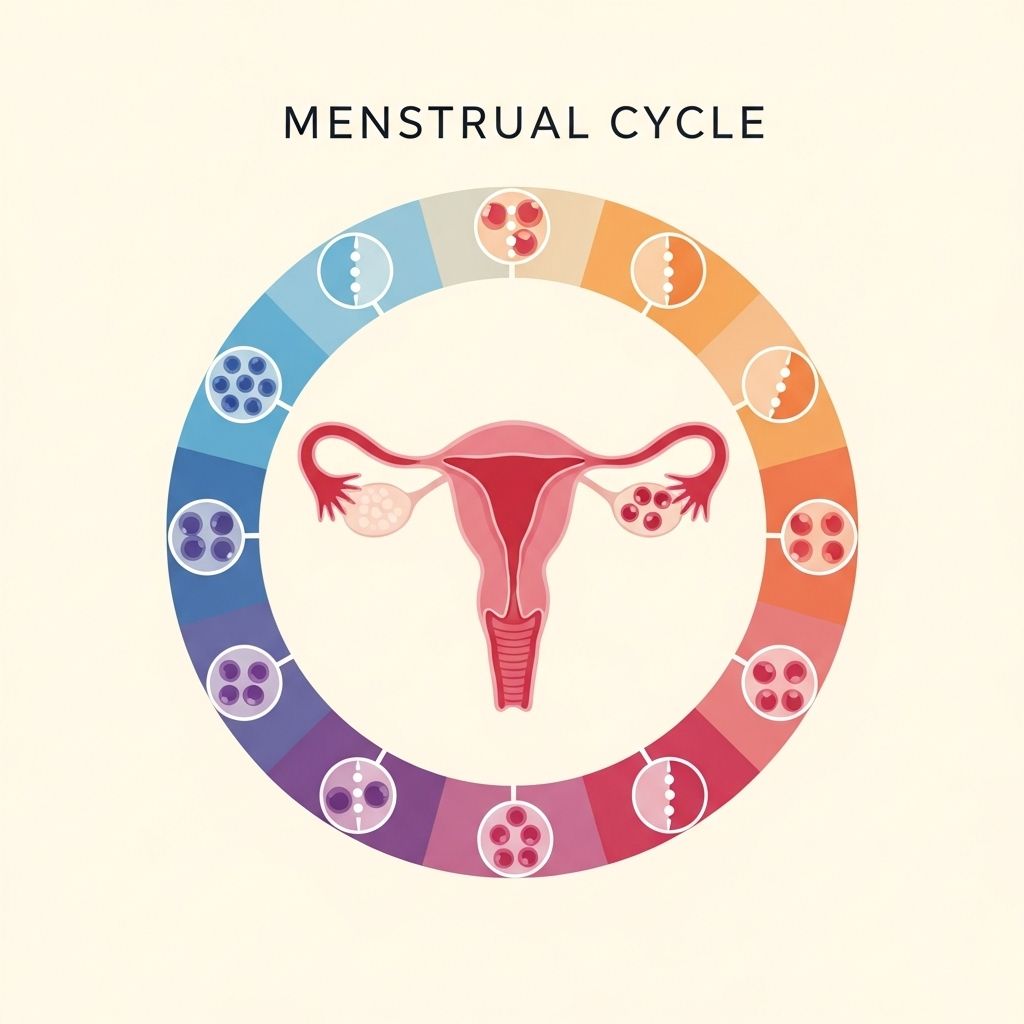
Main Phases of the Menstrual Cycle
The menstrual cycle is divided into distinct phases, each marked by characteristic hormonal and physical changes:
| Phase | Key Events | Main Hormones |
|---|---|---|
| Menstrual Phase | Shedding of uterine lining; menstrual bleeding occurs | Decline in estrogen & progesterone |
| Follicular Phase | Ovarian follicles mature; uterine lining rebuilds | Follicle Stimulating Hormone (FSH), Estrogen |
| Ovulation | Release of mature egg from the ovary | Luteinizing Hormone (LH) surge |
| Luteal Phase | Corpus luteum forms; uterine lining readies for implantation | Progesterone (primarily), Estrogen |
1. Menstrual Phase
This phase marks the beginning of the cycle. It starts on Day 1 of menstrual bleeding, which is when the thickened lining of the uterus is expelled. This bleeding lasts 3-7 days for most women.
2. Follicular (Proliferative) Phase
Concurrent with menstruation, FSH (follicle-stimulating hormone) prompts ovarian follicles to develop. Typically, one becomes dominant and matures into a Graafian follicle, increasing estrogen production. Estrogen encourages the uterine lining (endometrium) to regrow and thicken, preparing it for a potential embryo.
- Begins on Day 1 and ends with ovulation.
- Variable in length, usually 10-16 days.
- Estrogen levels rise during this phase.
- Cervical mucus becomes thinner and more slippery to aid sperm movement.
3. Ovulation
Triggered by a surge in LH (luteinizing hormone), the dominant follicle ruptures, releasing an egg (oocyte). This typically occurs around the midpoint—Day 14 in a standard 28-day cycle.
- Fertility is highest around ovulation.
- Ovulation may be accompanied by mild pelvic pain in some women.
- Post-ovulation, estrogen decreases slightly.
4. Luteal (Secretory) Phase
After ovulation, the ruptured follicle transforms into the corpus luteum, which secretes progesterone. Progesterone further prepares the endometrium, thickening and maturing it to support a fertilized egg if conception occurs.
- Typically lasts about 14 days across cycles.
- Progesterone dominates, causing basal body temperature to rise slightly.
- Cervical mucus thickens, becoming less hospitable to sperm.
- If pregnancy does not happen, the corpus luteum degrades, hormones fall, and menstruation begins.
Menstrual Cycle Hormones and Their Functions
Multiple hormones work together to regulate the menstrual cycle:
- Follicle-Stimulating Hormone (FSH): Promotes the growth of ovarian follicles in the ovary.
- Luteinizing Hormone (LH): Triggers ovulation and development of the corpus luteum.
- Estrogen: Produced by the developing follicles; stimulates thickening of the uterine lining and regulates other cycle hormones.
- Progesterone: Secreted by the corpus luteum; prepares the uterine lining for implantation and supports early pregnancy.
- Gonadotropin-Releasing Hormone (GnRH): Released by the hypothalamus to stimulate the pituitary gland to secrete FSH and LH.
What is Normal?
Every woman’s menstrual cycle is unique, though there are key patterns considered typical:
- Cycle length: 24-38 days is typical.
- Menstrual flow: Usually 3-7 days of bleeding.
- Amount of flow: Around 30-80 milliliters (2-6 tablespoons) of blood lost during a period.
- Variation: Some cycles might be longer, shorter, heavier, or lighter—especially in early years after menstruation begins or before menopause.
Factors that can influence the cycle include stress, significant weight changes, intense exercise, medical conditions, and certain contraceptive methods.
Common Menstrual Terminology
- Menarche: Onset of the first menstrual period, typically around age 12-13.
- Menopause: Permanent end of menstruation, occurring around age 50-51 (but can vary).
- Amenorrhea: Absence of menstruation for three cycles or more.
- Oligomenorrhea: Infrequent periods (cycle length greater than 38 days).
- Polymenorrhea: Frequent periods (cycle length less than 24 days).
Tracking and Understanding Your Menstrual Cycle
Keeping a menstrual calendar can provide valuable information for both personal awareness and healthcare visits. Tracking can include:
- First and last days of bleeding
- Flow intensity (light, moderate, heavy)
- Accompanying symptoms (pain, mood changes, etc.)
- Cycle length from one period to the next
- Irregularities or skipped cycles
This data can help identify patterns, inform contraceptive or fertility choices, and detect abnormalities early.
When to Seek Medical Advice?
Minor cycle irregularities can be common, but certain changes warrant prompt medical attention:
- Periods lasting longer than 8 days
- Excessively heavy bleeding (soaking through a pad or tampon every 1-2 hours)
- Missed periods for more than three cycles (excluding pregnancy, lactation, or menopause)
- Severe pain unrelieved by typical over-the-counter medications
- Sudden irregular cycles after years of regularity
- Bleeding between periods or after intercourse
These could signal underlying conditions such as hormonal imbalances, thyroid disorders, polycystic ovary syndrome (PCOS), fibroids, endometriosis, or other health concerns.
Common Menstrual Cycle Issues
- Dysmenorrhea: Painful periods, often due to increased prostaglandin production leading to strong uterine contractions.
- Premenstrual Syndrome (PMS): Mood swings, bloating, and discomfort preceding menstruation. Often managed by lifestyle changes or, in some cases, medication.
- Premenstrual Dysphoric Disorder (PMDD): A severe form of PMS with significant impact on daily function, requiring targeted medical treatment.
- Anovulatory Cycles: Occasional cycles where ovulation does not occur, common in adolescence or near menopause.
Influence of Birth Control on the Menstrual Cycle
Contraceptive methods can affect menstrual patterns:
- Oral contraceptives: Regulate periods, lighten flow, and can decrease period pain.
- Hormonal IUDs: Can cause lighter periods or stop menstruation altogether.
- Extended-cycle pills: Reduce the number of periods per year (e.g., every three months).
It is important to discuss expected changes with a healthcare provider before starting any new contraceptive.
Menstrual Cycle and Life Stages
- Adolescence: Cycles may be highly irregular during the first few years post-menarche.
- Reproductive Years: Cycles often become more regular.
- Perimenopause: Cycles become increasingly irregular before menopause.
- Menopause: Cycles stop permanently, marking the end of fertility.
Frequently Asked Questions (FAQs)
Q: How can I tell if my period is normal?
A: Most healthy periods last between 3-7 days, occur every 24-38 days, and involve blood loss of around 2-6 tablespoons. Large deviations from this pattern may require evaluation.
Q: What can cause irregular periods?
A: Stress, rapid weight change, excessive exercise, medical conditions like PCOS or thyroid disorders, and certain medications can all disrupt your menstrual cycle.
Q: Is it normal to have pain during my period?
A: Mild to moderate cramping is normal for many, but severe pain that limits daily activities should be assessed by a healthcare provider.
Q: Can I get pregnant at any time during my cycle?
A: Pregnancy is most likely in the days around ovulation, typically in the middle of the cycle. However, variations in cycle timing mean tracking is important for those trying to conceive or avoid pregnancy.
Q: Should I be concerned if my cycle changes as I age?
A: Cycles may change with life stages; irregularity is common in adolescence and perimenopause. Sudden significant changes in midlife should be discussed with a healthcare provider.
Tips for Menstrual Health and Wellness
- Track your menstrual cycles and any changes.
- Maintain a balanced diet and healthy weight.
- Exercise regularly, but avoid excessive overtraining.
- Stay hydrated and manage stress through mindfulness or relaxation techniques.
- Ask your healthcare provider about concerns or changes in your cycle.
Summary
Understanding the menstrual cycle empowers individuals to monitor reproductive health, identify potential issues early, and make informed decisions about wellness, birth control, and fertility. If in doubt about cycle patterns or health changes, consult with a healthcare professional for assessment and guidance.
References
- https://www.ncbi.nlm.nih.gov/books/NBK500020/
- https://my.clevelandclinic.org/health/articles/10132-menstrual-cycle
- https://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/menstrual-cycle/art-20047186
- https://www.hopkinsguides.com/hopkins/view/Johns_Hopkins_Diabetes_Guide/547090/all/Menstrual_Cycle_and_Glycemia_in_Premenopausal_Women
- https://pure.johnshopkins.edu/en/publications/menstrual-disorders-and-their-management-4
- https://www.youtube.com/watch?v=3Lt9I5LrWZw
Read full bio of medha deb












