Mantle Cell Lymphoma: Symptoms and Causes
Understand the warning signs, causes, and underlying genetics of mantle cell lymphoma—a rare but serious form of non-Hodgkin lymphoma.
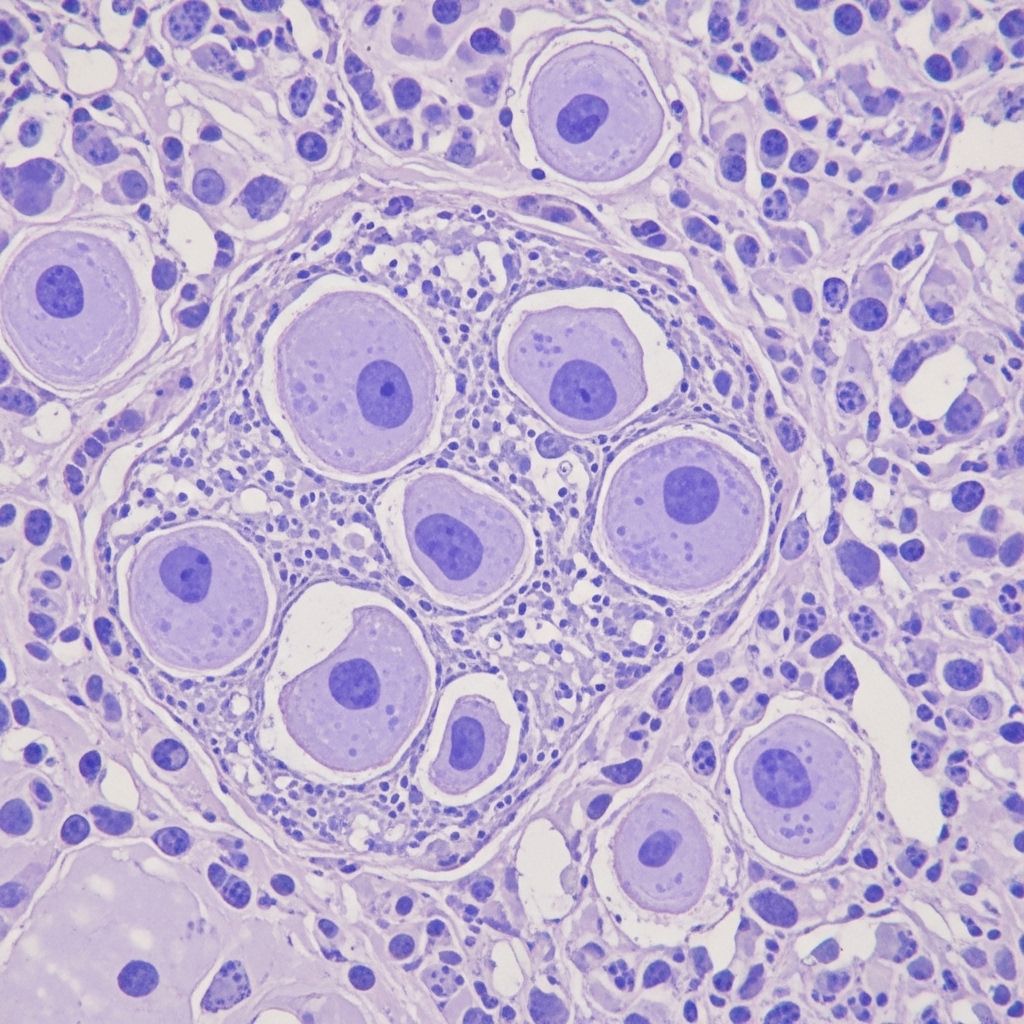
Mantle cell lymphoma (MCL) is a rare and aggressive subtype of non-Hodgkin lymphoma that primarily affects the lymphatic system. This form of cancer arises from malignant B lymphocytes in a part of the lymph node called the mantle zone. Given its subtle onset and non-specific symptoms, mantle cell lymphoma frequently goes undiagnosed until the disease is advanced. Understanding its symptoms, underlying causes, and risk factors is crucial for early detection and management.
Overview: What is Mantle Cell Lymphoma?
Mantle cell lymphoma is classified under non-Hodgkin lymphomas and specifically originates from B-cells. It accounts for approximately 6% of all non-Hodgkin lymphoma cases in the United States, making it a rare disease. MCL typically occurs in adults, with a higher prevalence in older males—most diagnoses are made in individuals between the ages of 60 and 70.
- Affects the “mantle zone” of lymph nodes: This is the outer edge of small lymphocytes encircling the lymphatic nodule core.
- B-cell origin: Emerging from a subtype of white blood cells crucial to the immune system.
- Aggressive nature: MCL tends to progress rapidly and often presents as widespread disease upon diagnosis.
- Rare frequency: About 1 out of every 200,000 people per year are diagnosed with MCL.
Signs and Symptoms of Mantle Cell Lymphoma
Symptoms of mantle cell lymphoma can vary significantly between individuals and often mimic those of less severe illnesses. In many cases, the disease is not detected until blood tests or imaging scans are performed for other reasons. A considerable proportion of patients do not experience symptoms during early stages (asymptomatic), leading to delayed diagnosis.
Common Symptoms
- Swollen and painless lymph nodes (neck, underarm, groin, chest, abdomen, pelvis)
- Fatigue or general weakness
- Unexplained weight loss
- Night sweats or fever
- Abdominal pain, discomfort, or bloating
- Loss of appetite
- Changes in bowel habits (diarrhea or constipation)
- Easy bruising or bleeding
- Headaches
- Indigestion, nausea, or vomiting
- Sensation of fullness soon after eating, especially if the spleen or abdominal lymph nodes are enlarged
When to Seek Medical Attention
Many of these symptoms are common to other, less serious conditions. However, persistent and unexplained swelling of lymph nodes, rapid weight loss, fever, and night sweats should prompt medical evaluation. Early detection can improve management and outcomes.
Distribution of Symptoms in the Body
MCL can involve almost any part of the body, but certain areas are more frequently affected:
- Lymph node regions: Especially the neck, underarms, and groin
- Waldeyer’s ring: A group of lymphoid tissues near the throat base, including tonsils and adenoids
- Abdominal organs: Spleen and liver enlargement (splenomegaly and hepatomegaly)
- Gastrointestinal tract: Involvement can cause fullness, indigestion, or altered bowel habits
- Bone marrow: Leading to changes in blood counts and increased vulnerability to infections
Causes of Mantle Cell Lymphoma
The exact cause of mantle cell lymphoma remains under investigation, but research has identified characteristic genetic abnormalities that drive the disease.
Key Genetic Abnormality: t(11;14) Translocation
- Chromosomal translocation: In most cases, MCL is associated with a specific genetic alteration known as t(11;14), in which pieces of chromosomes 11 and 14 are swapped.
- Overproduction of cyclin D1: This translocation causes the B-cells to produce excessive amounts of a protein called cyclin D1, which drives abnormal cell proliferation.
- Diagnostic marker: The presence of cyclin D1 overexpression (detected via biopsy or lab tests) is a defining feature of MCL and helps differentiate it from other lymphomas.
Other Genetic and Cellular Changes
- Errors in lymphocyte production: Transformation of normal B lymphocytes into malignant cells
- Abnormal proliferation: Uncontrolled multiplication of these abnormal cells spreads disease into lymph nodes, spleen, bone marrow, and other tissues
Risk Factors
Several risk factors can increase the likelihood of developing mantle cell lymphoma:
- Age: The average age at diagnosis ranges from 60 to 70 years
- Gender: MCL is more commonly diagnosed in males than females
- Genetic predisposition: While most cases do not have a hereditary basis, certain genetic features increase risk
- Other underlying health conditions: Some studies suggest a possible association with autoimmunity or immune compromise, but these links are not as clear as in other lymphomas
Pathophysiology: How Mantle Cell Lymphoma Develops
Mantle cell lymphoma develops as a result of uncontrolled growth of B lymphocytes in the mantle zone of lymph nodes. This process typically follows genetic mutations that alter normal cell signaling and apoptosis (programmed cell death), specifically:
- Malignant B cells accumulate in lymphatic tissues, causing lymph node enlargement
- These cells can invade the spleen, bone marrow, liver, gastrointestinal tract, and rarely, other organs
- The involvement of vital organs can lead to complications such as anemia, thrombocytopenia (low platelet count), and increased susceptibility to infection
Because MCL often grows aggressively and spreads beyond lymph nodes, patients may have advanced, widespread disease at the time of diagnosis.
Diagnosis of Mantle Cell Lymphoma
MCL is typically diagnosed based on the combination of clinical symptoms, physical examination, laboratory findings, and imaging studies. Diagnosis often occurs at a late stage, partly because early symptoms are mild or nonspecific. The following tools are used to confirm MCL:
- Biopsy: A tissue sample from a swollen lymph node or other involved site is examined under the microscope. Pathologists look for overexpression of cyclin D1 and other cell markers.
- Blood tests: Routine bloodwork may show elevated white blood cell counts, anemia, or abnormal levels of proteins such as lactate dehydrogenase (LDH) and beta-2 microglobulin.
- Imaging studies: CT or PET scans help identify the distribution and size of lymphadenopathy and detect involvement of internal organs.
- Bone marrow biopsy: Evaluates the extent of marrow involvement, important for staging the disease.
Frequently Affected Body Systems
| Body System/Region | Potential Manifestations |
|---|---|
| Lymphatic System | Swollen lymph nodes, especially in the neck, armpits, and groin |
| Digestive (Gastrointestinal) Tract | Bloating, pain, changes in bowel movements, nausea, indigestion |
| Spleen/Liver | Fullness, discomfort, pain from organ enlargement |
| Bone Marrow | Fatigue, increased infection risk, easy bruising/bleeding |
| General Body | Weight loss, night sweats, fever |
Complications and Prognosis
Late-stage MCL may cause the following complications:
- Severe cytopenias: Low blood cell counts due to bone marrow infiltration
- Widespread organ involvement: Spleen, liver, gastrointestinal tract, and rarely the brain
- Increased risk of infections: Due to immune system dysfunction or chemotherapy side effects
The overall prognosis depends on several factors, including the stage at diagnosis, the presence of certain genetic mutations, age, and overall health. Despite its aggressive nature, advances in targeted therapies and immunotherapy have improved patient outcomes.
Prevention and Outlook
There is currently no proven way to prevent mantle cell lymphoma, given the unclear causes and absence of specific lifestyle or environmental triggers. The best approach is awareness of symptoms and early medical consultation for unexplained lymph node enlargement or persistent systemic symptoms.
Frequently Asked Questions (FAQs)
Q: Who is most at risk for mantle cell lymphoma?
A: Middle-aged to older adults, particularly males aged 60 to 70, are most commonly diagnosed with MCL. Family history is generally not a significant risk factor, and no distinct environmental risk factors are known.
Q: Are the symptoms of mantle cell lymphoma unique?
A: The symptoms of MCL can mimic a wide range of common illnesses, making early diagnosis challenging. Classic lymphoma signs such as painless swollen lymph nodes, unexplained weight loss, night sweats, and severe fatigue are important red flags.
Q: Can mantle cell lymphoma be cured?
A: MCL is generally considered difficult to cure, especially once advanced, but some patients achieve long-term remission with combination therapies. Treatment approaches are evolving and include chemotherapy, immunotherapy, and newer targeted drugs.
Q: Is cyclin D1 important in all types of lymphoma?
A: No, overproduction of cyclin D1 is a hallmark of mantle cell lymphoma specifically, due to the t(11;14) chromosomal translocation. This marker is used to distinguish MCL from other B-cell lymphomas.
Q: Should I see a doctor if I have swollen lymph nodes?
A: Persistent or unexplained lymph node swelling, especially if accompanied by systemic symptoms (weight loss, night sweats, persistent fever), should be evaluated by a healthcare professional to rule out lymphoma and other conditions.
Note: If you are concerned about your symptoms or have a family history of lymphoma or related cancers, consult your physician promptly for evaluation and, if needed, further testing.
References
- https://www.lymphoma.org/understanding-lymphoma/aboutlymphoma/nhl/mantle-cell-lymphoma/
- https://rarediseases.org/rare-diseases/mantle-cell-lymphoma/
- https://my.clevelandclinic.org/health/diseases/24030-mantle-cell-lymphoma
- https://www.mayoclinic.org/diseases-conditions/b-cell-lymphoma/symptoms-causes/syc-20586599
- https://www.mayoclinic.org/diseases-conditions/lymphoma/symptoms-causes/syc-20352638
- https://www.mayoclinic.org/diseases-conditions/mantle-cell-lymphoma/diagnosis-treatment/drc-20584873
- https://www.mayoclinic.org/diseases-conditions/non-hodgkins-lymphoma/symptoms-causes/syc-20375680
- https://www.mayoclinic.org/documents/mc1604-0908-pdf/doc-20078848
- https://www.mayoclinic.org/diseases-conditions/mantle-cell-lymphoma/care-at-mayo-clinic/mac-20584875
Read full bio of medha deb