Mammary Duct Ectasia: Symptoms, Causes and Diagnosis
Learn about mammary duct ectasia: a noncancerous breast condition, its symptoms, causes, diagnosis, treatment options and when to seek care.
Mammary duct ectasia is a noncancerous (benign) condition affecting the breast’s milk ducts, typically occurring near the nipple. This article explains its symptoms, underlying causes, diagnostic strategies, and guides when to seek medical attention. Understanding this condition helps reduce anxiety related to benign breast changes and promotes appropriate care-seeking behavior.
Overview
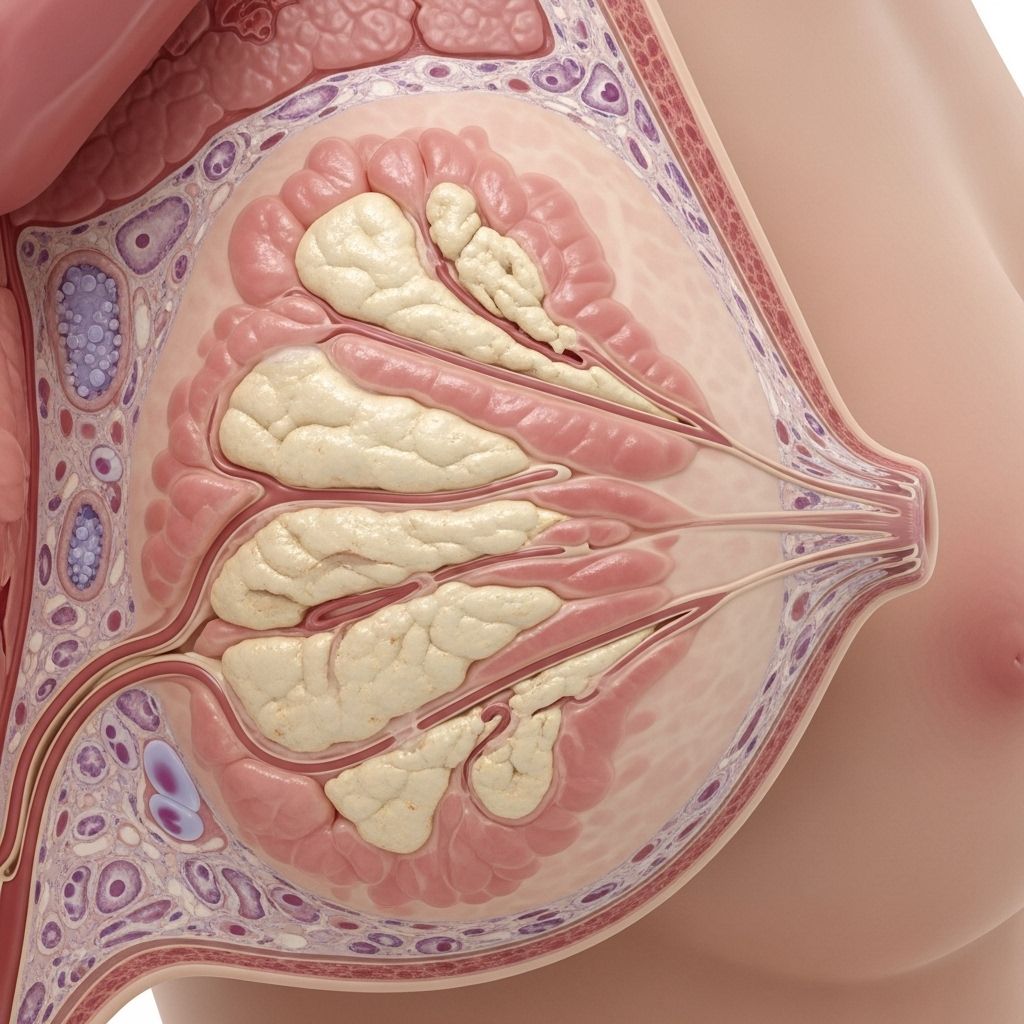
Mammary duct ectasia (pronounced ek-TAY-zhuh) is a benign breast condition that involves the milk ducts—the tubes responsible for transporting milk from the glandular tissue to the nipple. In this condition:
- One or more milk ducts beneath the nipple widen (become dilated).
- Duct walls may thicken and become inflamed.
- Ducts may fill with fluid and become clogged by a thick, sticky substance (often yellow or green in color).
Most commonly, mammary duct ectasia arises in women around perimenopause (ages 45 to 55), but it can also occur postmenopausally and, rarely, in younger women.
Key Points
- Mammary duct ectasia is noncancerous and not a risk factor for breast cancer.
- The condition can be asymptomatic, but may present with various breast symptoms.
- Most cases improve without medical intervention; some may require antibiotics or minor surgery.
Symptoms
Many people with mammary duct ectasia experience no symptoms. When symptoms do occur, they may include:
- Nipple discharge, which can be dirty white, yellow, green, or sometimes dark (even black).
- Breast tenderness or discomfort beneath the nipple or areola.
- Redness, swelling, or discoloration of the areola (area around the nipple).
- Lump or palpable thickening near the involved duct.
- Nipple inversion (the nipple turning inward that was previously outward).
If the clogged duct becomes infected (a condition called periductal mastitis), further symptoms may develop:
- Persistent or increasing breast tenderness.
- Noticeable inflammation or redness surrounding the nipple.
- Fever (suggesting a bacterial infection).
When to Seek Medical Attention
- If you notice a new lump, persistent spontaneous nipple discharge, nipple inversion, or changes in nipple or areola appearance not related to menstrual cycle or pregnancy.
- If there is skin redness, warmth, or swelling around the nipple, especially with fever or chills (possible infection).
Causes
The precise cause of mammary duct ectasia is not always clear, but several factors are known or suspected contributors:
- Aging and hormonal changes: Structural changes in breast ducts often occur as women approach menopause, leading to widening or dilation of ducts and thickening of their walls.
- Inflammation: Chronic or repeated episodes of inflammation can damage duct walls, allowing for clogging and fluid accumulation.
- Bacterial infection: Clotted ducts sometimes become infected when bacteria enter through ducts or cracks in the nipple, resulting in periductal mastitis.
- Smoking: Some studies suggest that smoking may contribute due to its effect on ductal tissue and vascular supply.
Risk Factors
- Age (most common in women ages 45–55)
- History of nipple inversion
- Smoking tobacco
- Previous breast infections or inflammatory breast conditions
Diagnosis
Diagnosing mammary duct ectasia usually involves a combination of clinical evaluation and imaging, with additional tests to rule out other causes for symptoms.
Steps in Diagnosis
- Clinical history and physical examination: Your healthcare professional will ask about your breast symptoms, medical history, and perform a focused breast and nipple examination.
- Imaging:
- Ultrasound: Uses sound waves to visualize the dilated ducts or other abnormalities in the region beneath the nipple and areola.
- Mammogram: X-ray of the breast, often performed to rule out other causes for lumps or nipple discharge, and to obtain a detailed view if any abnormalities are felt or seen.
- MRI (Magnetic Resonance Imaging): Ordered when other imaging is inconclusive, MRI provides high-resolution images to assess the structure of ducts and any associated masses or changes.
- Biopsy: If a lump is present, a needle or sometimes surgical biopsy may be performed to obtain breast tissue for microscopic evaluation. This is especially important to rule out breast cancer or other pathologies.
| Test | Purpose | Details |
|---|---|---|
| Ultrasound | Initial evaluation of ducts and breast tissue | Detects duct dilation, fluid, or thickening |
| Mammogram | Screening for masses or suspicious changes | X-ray images; more detailed if needed (diagnostic mammogram) |
| MRI | Further assessment if ultrasound/mammogram are inconclusive | High-resolution imaging—helpful for complex cases |
| Biopsy | Rule out cancer or other diseases | Needle or excisional sampling; tissue evaluated microscopically |
Treatment and Self-Care
In many cases, mammary duct ectasia resolves on its own without specific treatment. When symptoms persist or infection develops, several strategies are used:
Self-Care Measures
- Applying warm compresses to the affected breast to reduce discomfort and promote drainage.
- Over-the-counter pain relievers (such as ibuprofen) to alleviate tenderness or pain.
- Maintaining good breast hygiene, wearing a supportive bra, and avoiding nipple squeezing.
Medical Treatment
- Antibiotics: If a bacterial infection (mastitis) develops, a course of oral antibiotics is typically prescribed.
- Surgical Intervention: If there is persistent ductal blockage, significant discomfort, or recurrent infections that don’t respond to conservative measures:
- Minor surgery may be performed to remove the affected duct(s).
- This surgery is generally simple, performed under local anesthesia, and involves removing the abnormal duct via an incision along the edge of the areola.
- Recovery is typically quick, though a slight scar may remain.
Follow-Up and Prognosis
Most individuals recover fully without complications. The condition does not increase the future risk of breast cancer.
FAQs: Frequently Asked Questions About Mammary Duct Ectasia
Q: Is mammary duct ectasia a sign of breast cancer?
A: No. Mammary duct ectasia is a benign, noncancerous condition and does not progress to or increase the risk of breast cancer.
Q: Does mammary duct ectasia always need treatment?
A: No. Many cases resolve on their own without any treatment. Treatment is needed only for troublesome symptoms or infection.
Q: What kind of nipple discharge does this condition cause?
A: Discharge can range from dirty white, yellow, green, or sometimes dark brown or black. The amount and color may vary, and it can emerge from one or both nipples.
Q: What increases my risk for this condition?
A: Risk increases with age, especially between 45–55 years and after menopause. Smoking and previous breast infections may contribute as well.
Q: Can men get mammary duct ectasia?
A: Mammary duct ectasia is extremely rare in men, as male breast ductal tissue is less developed.
When to Contact Your Healthcare Provider
- Any new breast lump or area of thickening
- Unusual, spontaneous or persistent nipple discharge
- Redness, warmth, swelling, or pain of the breast or areola
- New-onset nipple inversion
- Presence of fever or chills with breast symptoms
Takeaway Messages
- Mammary duct ectasia is a benign and treatable condition.
- Seek evaluation for any significant, persistent, or new breast changes.
- Awareness and timely consultation can often prevent complications and provide peace of mind.
References
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/diseases-conditions/mammary-duct-ectasia
- https://www.mayoclinic.org/diseases-conditions/mammary-duct-ectasia/symptoms-causes/syc-20374801
- https://www.augustahealth.com/disease/mammary-duct-ectasia/
- https://www.mayoclinic.org/diseases-conditions/mammary-duct-ectasia/diagnosis-treatment/drc-20374806
- https://my.clevelandclinic.org/health/diseases/17949-mammary-duct-ectasia
- https://www.mayoclinic.org/diseases-conditions/mammary-duct-ectasia/multimedia/mammary-duct-ectasia/img-20007970
- https://www.mayoclinic.org/symptoms/nipple-discharge/basics/causes/sym-20050946
- https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/managing-plugged-ducts-mastitis-when-breastfeeding
Read full bio of Sneha Tete












