Understanding Mallory-Weiss Tear: Causes, Symptoms, Diagnosis, and Treatment
Gain comprehensive knowledge on Mallory-Weiss tears — from causes and risks to diagnosis, treatment options, and prevention strategies.
Mallory-Weiss Tear
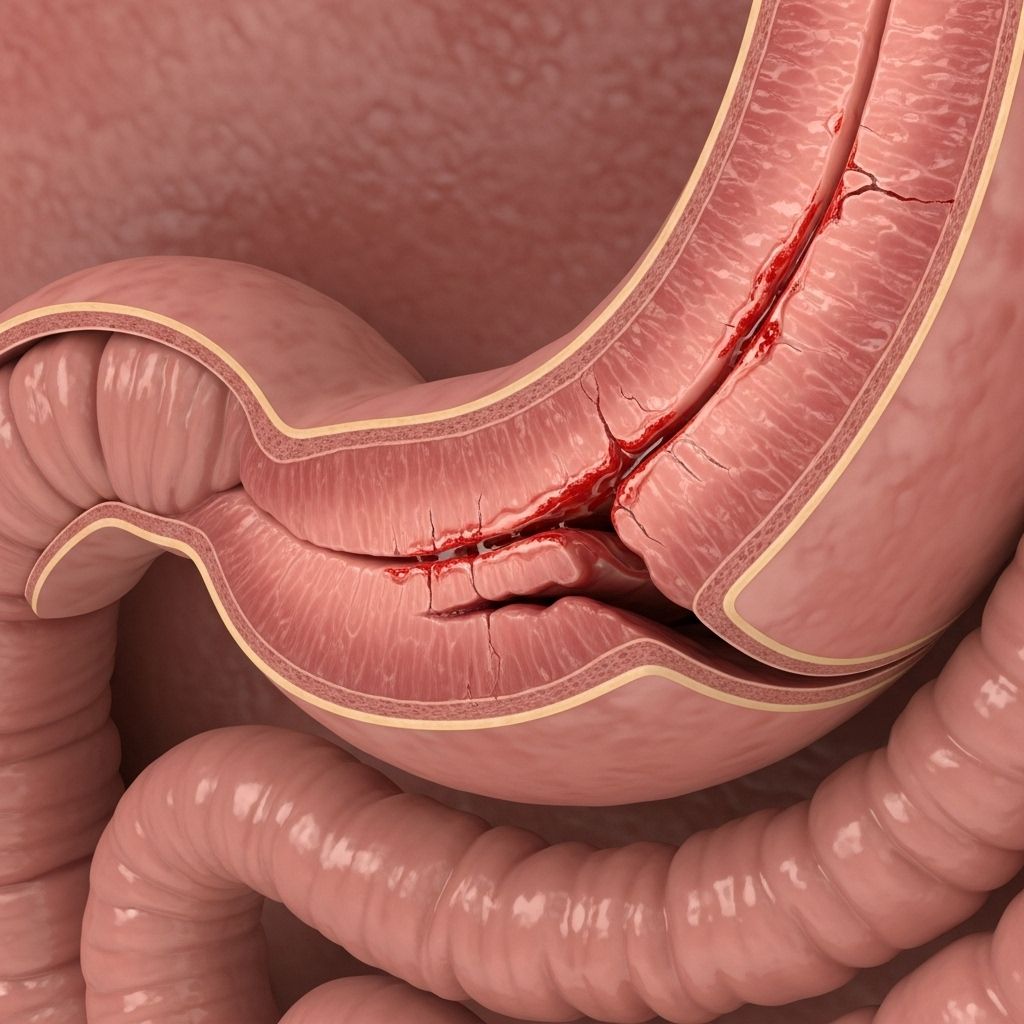
Mallory-Weiss tear is a condition characterized by a tear in the mucous membrane at the junction where the esophagus meets the stomach. This tear most commonly results from severe or prolonged vomiting but can develop due to various other causes. Mallory-Weiss tears frequently lead to upper gastrointestinal bleeding, a potentially alarming medical event necessitating quick evaluation and management.
What is a Mallory-Weiss Tear?
A Mallory-Weiss tear refers to a laceration or tear in the mucosal lining of the lower esophagus or upper stomach. The esophagus is the muscular tube conveying food from the throat to the stomach. This lesion usually occurs at the gastroesophageal junction and can result in significant bleeding into the gastrointestinal tract. Mallory-Weiss syndrome encompasses the tear and any associated symptoms, particularly bleeding.
Causes of Mallory-Weiss Tear
The primary cause of a Mallory-Weiss tear is forceful or prolonged vomiting. However, several situations and activities can increase the risk of such a tear, including:
- Severe and prolonged vomiting (as in acute gastroenteritis or bulimia nervosa)
- Chronic, heavy alcohol use
- Intense or prolonged coughing
- Seizures and convulsions
- Severe or prolonged hiccups
- Trauma to the chest or abdomen
- Hiatal hernia: when part of the stomach pushes through the diaphragm
- Heavy lifting or straining
- Gastritis: inflammation of the stomach lining
- Childbirth: increased abdominal pressure during labor
- Cardiopulmonary resuscitation (CPR): rarely, the process of performing CPR can cause a tear
Mallory-Weiss tears may also develop spontaneously in certain individuals or may be linked to underlying disorders that predispose to increased abdominal pressure.
Risk Factors
Several factors can increase the likelihood of developing a Mallory-Weiss tear, such as:
- Chronic alcoholism: repeated episodes of vomiting associated with alcohol use
- Male sex: Mallory-Weiss tears are more commonly diagnosed in men than women
- Middle to older age: especially ages 40–60, although cases can occur at any age, including in children
- Preexisting gastrointestinal disease: such as hiatal hernia or gastritis
Symptoms of Mallory-Weiss Tear
The hallmark symptom of a Mallory-Weiss tear is gastrointestinal bleeding. The bleeding can range from minor to severe and often manifests with:
- Hematemesis: vomiting bright red blood or material that looks like coffee grounds
- Melena: black, tarry, or sticky stools due to digested blood
- Fatigue and weakness: resulting from blood loss
- Dizziness or faintness (syncope), especially with severe bleeding
- Abdominal pain possibly radiating to the back
- Shortness of breath
- Diarrhea (less common)
These symptoms can be sudden and distressing, often prompting rapid medical attention. In severe or prolonged bleeding, additional signs such as pallor, rapid heartbeat, and even shock may develop. Severe, untreated cases can lead to life-threatening complications, including anemia and circulatory collapse.
Complications
Possible complications due to a Mallory-Weiss tear include:
- Ongoing or recurrent bleeding
- Anemia: due to blood loss
- Shock and organ failure: in rare, massive hemorrhage situations
- Death: exceptionally rare, mostly in cases with comorbidities or delays in treatment
- Increased risk of bleeding: in patients with liver disease (cirrhosis) or clotting disorders
Diagnosis
The diagnosis of a Mallory-Weiss tear begins with a careful clinical evaluation, focusing on the patient’s symptoms (especially evidence of upper gastrointestinal bleeding) and risk history. To confirm the diagnosis and assess the severity, doctors use several tools:
Physical Examination and Patient History
- Assessment for signs of bleeding or shock
- Recording triggers such as vomiting, trauma, or alcohol intake
Laboratory Tests
- Complete blood count (CBC): looks for low hematocrit or hemoglobin, indicating blood loss
- Coagulation studies: check for blood clotting problems
- Liver function tests: may be assessed if cirrhosis or liver dysfunction is suspected
Diagnostic Procedures
- Esophagogastroduodenoscopy (EGD or upper endoscopy): This is the gold standard for diagnosis. A thin, flexible tube with a camera is inserted through the mouth into the esophagus and stomach. It allows direct visualization of the tear, assessment of bleeding, and possible endoscopic treatment. EGD is most effective if performed while there is active bleeding or soon after symptoms begin.
Other imaging or diagnostic studies (such as angiography) may be reserved for rare cases where bleeding is recurrent, severe, or not accessible via endoscopy.
Treatment Options for Mallory-Weiss Tear
Mallory-Weiss tears frequently resolve without specific treatment. However, management is guided by the severity of the tear, the degree of bleeding, and the patient’s overall health.
Conservative (Non-Invasive) Treatment
- Observation: In the majority of cases, bleeding stops spontaneously within a few hours to several days.
- Medical therapy: Doctors may prescribe medications to reduce stomach acid, such as proton pump inhibitors or H2 blockers. Lower acid levels allow better healing and decrease the chance of rebleeding.
- Supportive measures: Rest, nil per os (NPO – avoiding food or drink), and monitoring may be recommended for mild cases.
Endoscopic Treatment
If bleeding persists, recurs, or is severe, endoscopic intervention is the next step:
- Epinephrine Injection: A diluted adrenaline solution may be injected near the tear to constrict blood vessels and reduce bleeding.
- Thermal coagulation: Endoscopic electrocoagulation, argon plasma coagulation, or multipolar coagulation are used to cauterize blood vessels.
- Endoscopic Clips or Band Ligation: Application of tiny metal clips or bands to close the tear.
- Sclerotherapy: (less common) — injection of a sclerosing (hardening) agent to promote clotting and vessel closure.
Angiotherapy
If endoscopic therapy fails or is unavailable, selective angiotherapy may be used. This involves radiologically guided injection of vasoconstrictor drugs or embolization of the bleeding vessel, usually the left gastric or superior mesenteric artery.
Surgical Intervention
Surgery is rarely needed and reserved for refractory or life-threatening bleeding. Procedures include direct laparoscopic repair of the tear, oversewing of the bleeding area, or, in extremely rare instances, balloon tamponade with a Sengstaken-Blakemore tube as a last resort in debilitated patients.
Blood Transfusions
- Transfusions: For patients with significant blood loss, transfusion of packed red blood cells may be necessary to restore hemodynamic stability and oxygen-carrying capacity.
Recovery and Prognosis
- Most Mallory-Weiss tears heal completely within 72 hours without further intervention.
- Re-bleeding is uncommon, particularly after a single episode and successful initial management.
- The majority of patients have an excellent prognosis, especially in the absence of comorbidities such as liver cirrhosis or clotting disorders.
- Patients with underlying liver disease may face a higher risk of recurrence and complications.
Prevention of Mallory-Weiss Tear
- Treat underlying causes of vomiting (e.g., gastroenteritis, eating disorders) quickly and effectively.
- Limit alcohol consumption and avoid binge drinking.
- Manage chronic coughs and avoid excessive straining when possible.
- Seek medical guidance during violent episodes of vomiting or coughing, especially if at risk.
Living with and Managing a Mallory-Weiss Tear
Most individuals recover quickly and return to normal activities after a Mallory-Weiss tear, provided there are no underlying risks for further bleeding. If you have experienced a Mallory-Weiss tear, your healthcare provider will recommend:
- Avoidance of triggers: such as alcohol, heavy lifting, or medications that increase stomach acid
- Follow-up visits: to monitor healing and ensure no recurrence of bleeding
- Medication adherence: completing the prescribed course of acid-suppressing medications
If you experience recurrent vomiting or develop new symptoms of gastrointestinal bleeding, seek prompt medical evaluation.
Frequently Asked Questions (FAQs)
Q: What causes a Mallory-Weiss tear?
A: Most Mallory-Weiss tears are caused by forceful or prolonged vomiting, but they may also result from intense coughing, seizures, trauma, or conditions causing increased abdominal pressure such as childbirth or hiatal hernia.
Q: What are the main symptoms?
A: Symptoms often include vomiting blood (which can be bright red or look like coffee grounds), passing black or tarry stools, feeling weak or dizzy, and sometimes abdominal pain.
Q: How is a Mallory-Weiss tear diagnosed?
A: Diagnosis typically involves clinical evaluation and is confirmed by an upper endoscopy (EGD), which allows direct visualization of the tear and assessment for bleeding. Laboratory tests may support the diagnosis.
Q: Do these tears always require surgery?
A: No, surgery is rarely required. Most tears heal on their own. Severe or persistent bleeding can be addressed with endoscopic techniques or, in rare cases, angiotherapy or surgery.
Q: How can I prevent another Mallory-Weiss tear?
A: Preventative steps include treating underlying causes of vomiting, limiting alcohol intake, avoiding heavy lifting, and following medical advice about any underlying gastrointestinal or liver conditions.
Key Points
- Mallory-Weiss tear is a mucosal laceration at the junction of the esophagus and stomach, most often resulting from forceful vomiting.
- The primary symptom is upper gastrointestinal bleeding (vomiting blood, black stools).
- Diagnosis is mainly by endoscopy (EGD), and most cases resolve without invasive intervention.
- Endoscopic and, rarely, surgical techniques are available for severe ongoing bleeding.
- Prognosis is excellent for most patients with timely recognition and treatment.
References
For detailed medical references and more in-depth reading, consult leading clinical resources or reach out to a gastroenterologist for personalized advice and care.
References
- https://www.healthline.com/health/mallory-weiss-tear
- https://www.ummhealth.org/health-library/mallory-weiss-tear-0
- https://www.mountsinai.org/health-library/diseases-conditions/mallory-weiss-tear
- https://www.ncbi.nlm.nih.gov/books/NBK538190/
- https://my.clevelandclinic.org/health/diseases/22035-mallory-weiss-tear
- https://rarediseases.org/rare-diseases/mallory-weiss-syndrome/
- https://bestpractice.bmj.com/topics/en-us/1145
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=134&contentid=201
- https://www.merckmanuals.com/professional/gastrointestinal-disorders/esophageal-and-swallowing-disorders/mallory-weiss-syndrome
Read full bio of medha deb












