Macular Edema: Causes, Symptoms, Diagnosis, and Treatments
Understanding macular edema, its underlying causes, warning signs, diagnostic process, and the most effective treatment and prevention strategies.
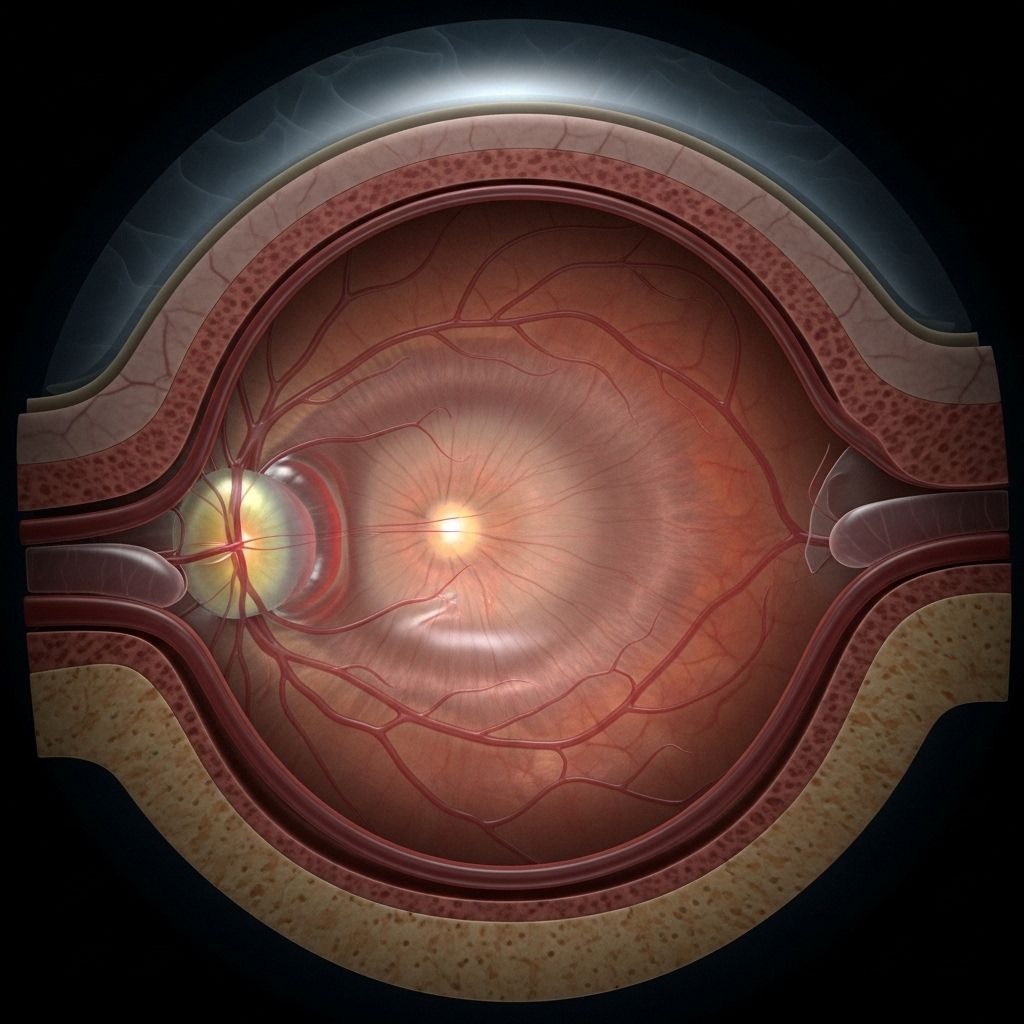
Macular edema is a common yet serious retinal condition that causes swelling and thickening in the macula—the central region of the retina responsible for sharp, detailed vision. Fluid accumulates due to leaking blood vessels, leading to blurry or distorted central vision and, if untreated, significant vision loss. Understanding the underlying causes, symptoms, diagnostic procedures, treatment options, and prevention strategies is essential for anyone at risk, particularly those living with diabetes or existing retinal conditions.
What is Macular Edema?
Macular edema develops when fluid collects in the macula, leading it to swell and impairing central vision. The macula is the area of the retina responsible for sharp, straight-ahead vision necessary for reading, recognizing faces, and fine visual tasks. When the macula swells, these vital visual functions are affected.
- Macular edema is usually secondary to other eye conditions or systemic diseases, such as diabetes, retinal vein occlusion, or inflammatory processes.
- Vision changes can range from mild to severe and may improve with appropriate intervention.
- Persistent macular edema can result in irreversible vision loss.
What Causes Macular Edema?
Macular edema is not a disease in itself but a manifestation of various underlying conditions that damage blood vessels in or near the macula, causing them to leak fluid. Key causes include:
- Diabetic Retinopathy: The leading cause, especially in adults with diabetes. Damaged retinal blood vessels leak fluid into the macula, causing swelling. When this occurs, it’s called diabetic macular edema (DME).
- Retinal Vein Occlusion (RVO): When veins in the retina are blocked, pressure and leakage increase, allowing fluid to accumulate in the macula. Both branch and central vein occlusions may result in macular edema.
- Age-Related Macular Degeneration (AMD): Particularly in wet AMD, abnormal blood vessels grow beneath the retina and may leak fluid or blood into the macula.
- Eye Surgery: Swelling of the macula may occur as a complication after cataract or other eye surgeries, often referred to as pseudophakic cystoid macular edema.
- Uveitis: Chronic inflammation in the eye can result in the breakdown of the blood-retinal barrier, leading to fluid leakage and swelling.
- Retinitis Pigmentosa (RP): Inherited retinal diseases like RP can disturb the blood-retinal barrier, predisposing to edema.
- Other Causes:
- Eales’ disease
- Retinal necrosis (from infections)
- Other retinopathies (e.g., hypertensive, radiation-induced)
- Certain medications (e.g., some glaucoma medicines)
Main Causes of Macular Edema
| Underlying Condition | How It Leads to Edema |
|---|---|
| Diabetic Retinopathy | High glucose damages blood vessels; leakage causes swelling in macula |
| Retinal Vein Occlusion | Blocked drainage increases pressure and fluid leaks into macula |
| Age-Related Macular Degeneration | Abnormal blood vessel growth and leakage beneath retina |
| Eye Surgery | Surgical trauma leads to inflammatory leakage in macula |
| Uveitis | Ocular inflammation breaks down blood-retinal barrier, causing leakage |
| Retinitis Pigmentosa | Genetic changes disturb barrier function, leading to leakage |
Symptoms: How Does Macular Edema Affect Vision?
Symptoms vary depending on the cause, severity, and duration of edema. Common signs include:
- Blurry or wavy central vision
- Colors appear faded or less vibrant
- Difficulty reading, recognizing faces, or focusing on detailed tasks
- Metamorphopsia (straight lines appearing bent or distorted)
- Micropsia (objects appearing smaller than actual)
- Central scotoma (a dark or blank spot in the middle of vision)
Peripheral (side) vision is usually unaffected. In some cases, symptoms are subtle and may go unnoticed in early stages, highlighting the importance of regular eye exams, particularly for at-risk populations.
Risk Factors: Who Is Most at Risk?
Anyone can develop macular edema, but certain factors increase risk:
- Diabetes (Type 1 or 2)
- Longstanding or poorly controlled blood sugar
- Hypertension (high blood pressure)
- Previous or ongoing retinal diseases
- Aging (risk rises in older adults)
- Eye injury, surgery, or chronic inflammation (uveitis)
- Family history of retinal disorders
Diagnosis: How Is Macular Edema Detected?
Accurate diagnosis is crucial for effective treatment. The evaluation typically involves:
- Comprehensive Eye Examination: Includes dilation to allow thorough assessment of the retina and macula.
- Optical Coherence Tomography (OCT): The gold-standard test. Provides detailed cross-sectional images of the retina, showing the presence and extent of edema.
- Fundus Fluorescein Angiography (FFA): A dye is injected into the arm; photographs are taken as dye passes through the eye’s blood vessels to highlight leakage areas.
- Visual Acuity Test: Measures the sharpness of central vision.
- Sometimes, other imaging tests or lab studies may be used if underlying systemic disease is suspected.
Treatment Options: How Is Macular Edema Managed?
Treatment depends on the cause, severity, and individual patient needs. Management goals are to reduce macular swelling, restore vision, and prevent further damage. Key treatments include:
- Anti-VEGF Injections: Medications injected directly into the eye (intravitreal injections) block vascular endothelial growth factor (VEGF), a protein that promotes leakage, especially effective for diabetic macular edema and wet AMD. Common anti-VEGF drugs include ranibizumab, aflibercept, and bevacizumab.
- Corticosteroids: Delivered as eye drops, posterior sub-Tenon’s injections, or sustained-release implants, these drugs reduce inflammation and vascular leakage. Steroids are particularly helpful in cases linked to inflammation, such as uveitis.
- Laser Photocoagulation: Precisely targets leakage points to seal blood vessels, used primarily in certain forms of diabetic macular edema and retinal vein occlusion.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Sometimes used topically for mild forms, or after surgery.
- Treating Underlying Causes: Proper management of diabetes, blood pressure, or uveitis reduces the likelihood of recurrence.
- Surgical Intervention: In rare and severe cases, a vitrectomy or other retinal surgery may be required when macular edema fails to respond to other treatments.
Treatment Approaches by Cause
| Cause | First-Line Treatments |
|---|---|
| Diabetic Macular Edema | Anti-VEGF injections, laser, systemic control of diabetes |
| Retinal Vein Occlusion | Anti-VEGF injections, steroids, laser |
| Post-Surgical | NSAID drops, steroids |
| Uveitis | Steroids, immunomodulatory treatment |
| Wet AMD | Anti-VEGF injections |
Outlook and Prognosis
The prognosis depends on both the underlying cause and how early treatment begins. Many cases, when addressed promptly, respond well to treatment with significant visual improvement. Delayed treatment or persistent/chronic edema increases the risk of permanent vision loss.
- Early intervention is essential to maximize outcomes.
- Regular follow-up appointments help monitor progress and address recurrence quickly.
- Some causes—such as chronic poorly controlled diabetes—may predispose to recurrent or persistent macular edema despite therapy.
Prevention: Steps to Protect Your Vision
Although not all causes of macular edema are preventable, you can greatly reduce your risk by:
- Managing systemic diseases like diabetes and high blood pressure carefully.
- Having regular comprehensive dilated eye exams, especially if you have diabetes, are over 50, or have a history of eye diseases.
- Promptly addressing visual changes or symptoms of eye inflammation.
- Following your doctor’s recommendations for medication and follow-up visits after eye surgeries or injuries.
For those with diabetes, strict blood sugar and blood pressure control is vital in preventing diabetic retinopathy, the root of most cases of macular edema in adults.
Living With Macular Edema
Coping with macular edema can be challenging, especially when vision is affected. Support resources, adaptive devices, and occupational therapy can help individuals maintain independence and quality of life. It’s important to:
- Follow your eye care professional’s guidance closely.
- Inform your provider promptly if symptoms worsen or new vision changes occur.
- Explore low-vision aids as needed to help manage daily tasks.
- Consider emotional support or counseling to cope with vision loss or limitations.
Frequently Asked Questions (FAQ)
What is the main cause of macular edema?
The most common cause is diabetic retinopathy, but it can also arise from retinal vein occlusion, wet age-related macular degeneration, post-surgical inflammation, and eye injuries.
Is macular edema permanent?
If detected early and treated appropriately, vision can often improve significantly. Chronic or untreated cases may result in permanent central vision loss.
What are the earliest symptoms?
Symptoms usually include blurry central vision and distorted or wavy appearance of straight lines. Peripheral vision is generally unaffected.
How is macular edema diagnosed?
Diagnosis involves a thorough eye examination, optical coherence tomography (OCT), and sometimes fundus fluorescein angiography to characterize blood vessel leakage.
Can macular edema be prevented?
Managing diabetes and hypertension, regular eye checkups, and rapid treatment of eye inflammation or injuries significantly lowers risk and limits vision loss.
Are the treatments painful?
Anti-VEGF or steroid injections are done in the office with topical anesthesia and are usually well tolerated. Any discomfort is transient.
Summary
Macular edema is a significant eye condition that can threaten vision if not properly managed. Early recognition, regular eye care, timely diagnosis, and advancements in targeted treatments have improved outcomes for most patients. By understanding the warning signs, risk factors, and available therapies, individuals can work closely with their eye care professionals to preserve their sight and maintain a high quality of life.
References
- https://www.ncbi.nlm.nih.gov/books/NBK576396/
- https://resources.healthgrades.com/right-care/eye-health/macular-edema
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/macular-edema
- https://www.asrs.org/patients/retinal-diseases/20/macular-edema
- https://www.healthline.com/health/eye-health/macular-edema
- https://www.healthline.com/health/eye-health/diabetic-macular-edema-symptoms-treatment
- https://www.medicalnewstoday.com/articles/macular-edema-vs-macular-degeneration
Read full bio of Sneha Tete












