Understanding Macular Degeneration and Retinal Detachment
Unraveling the risks, symptoms, and treatments for vision-threatening retinal conditions
Macular Degeneration and Retinal Detachment: What You Need to Know
Macular degeneration and retinal detachment are two distinct yet serious eye conditions that can significantly impact vision and quality of life. Both commonly affect older adults but can occur at any age due to various risk factors. Understanding how these conditions develop, their symptoms, and the latest approaches to prevention and treatment is crucial for preserving sight.
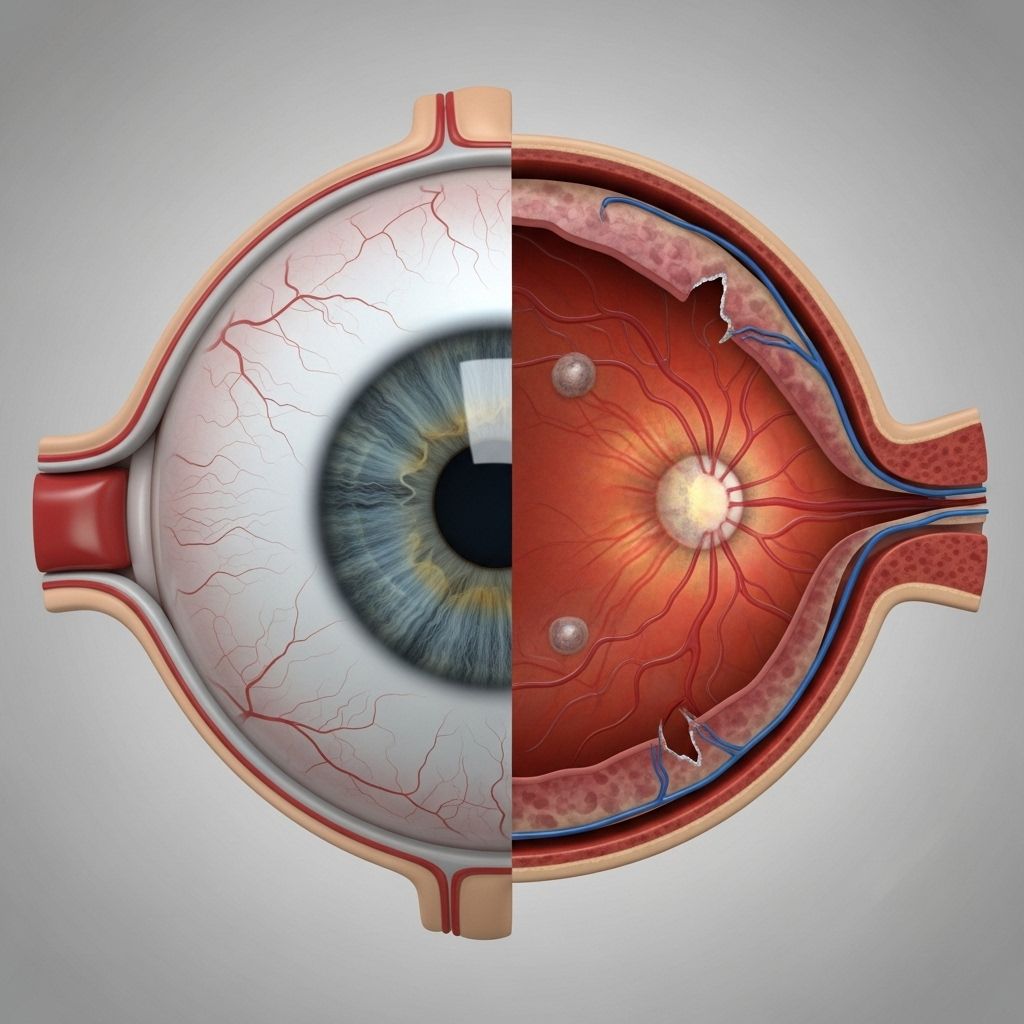
Overview of the Retina and Macula
The retina is a thin layer of nerve tissue lining the back of the eye that senses light and sends signals to the brain, creating visual images. At its center lies the macula, responsible for sharp, detailed central vision. Damage to the retina can result in loss of vision, and disruption to the macula specifically affects the ability to read, drive, and recognize faces.
What Is Macular Degeneration?
Macular degeneration refers to the progressive deterioration of the macula. The most common form is age-related macular degeneration (AMD), which primarily affects individuals over 60 years old. However, other types may develop earlier due to genetics or other factors.
Types of Macular Degeneration
- Dry (non-neovascular) macular degeneration: This form accounts for about 90% of AMD cases. It develops gradually, beginning with the accumulation of tiny yellow deposits called drusen beneath the retina. Over time, drusen increase in number and size, leading to thinning and patchy loss of retinal tissue, a process known as geographic atrophy.
Vision loss progresses slowly, and there is currently no way to reverse dry macular degeneration, although progression may be slowed with specific treatments. - Wet (neovascular) macular degeneration: Less common but far more aggressive. In wet AMD, abnormal blood vessels grow beneath the retina and leak fluid or blood, quickly damaging macular tissue and causing rapid vision loss. Prompt treatment is necessary to prevent permanent loss of sight.
Stages of Age-Related Macular Degeneration (AMD)
| Stage | Description |
|---|---|
| No AMD | No or few small drusen; normal pigment. |
| Early AMD | Increased number of small drusen or up to 20 medium-sized drusen; possible pigment changes. |
| Intermediate AMD | At least one large druse or extensive medium-sized drusen; non-central geographic atrophy (does not involve the fovea). |
| Advanced AMD | Central geographic atrophy affecting the fovea or presence of neovascularization (wet AMD). |
Symptoms of Macular Degeneration
- Blurry, fuzzy, or distorted central vision
- Difficulty reading, driving, or recognizing faces
- Dark, blank, or wavy areas in the center of vision
- Colors appear less vivid or bright
- Slow progression in dry AMD; rapid onset in wet AMD
Risk Factors
- Age (most significant factor)
- Genetics and family history
- Smoking
- Cardiovascular disease & hypertension
- High cholesterol
- Obesity
- Exposure to sunlight (UV light)
Treatment Options for Macular Degeneration
- Dry AMD:
- Currently irreversible, but progression may be slowed with AREDS2 formula vitamins and minerals (high-dose antioxidants, zinc, copper, lutein, and zeaxanthin).
- Ongoing research includes injectable therapies such as Izervay.
- Lifestyle changes: quitting smoking, healthy diet, blood pressure and cholesterol management.
Transform your understanding of the progression from dry to wet age-related macular degeneration. This insightful resource details how dry AMD can advance to its more severe form, highlighting the necessary steps for prevention and timely intervention that can protect your vision. - Wet AMD:
- Anti-VEGF (vascular endothelial growth factor) medications are injected into the eye to block abnormal blood vessel growth and leakage.
- Laser photocoagulation is rarely used but may help seal leaking vessels.
- Prompt diagnosis and treatment are critical for preserving sight.
What Is Retinal Detachment?
Retinal detachment is a medical emergency characterized by the separation of the retina from the underlying supportive tissue (choroid) at the back of the eye. When detached, the retina can no longer receive adequate oxygen and nutrients, leading to cell death and permanent vision loss if not treated quickly.
Types of Retinal Detachment
- Rhegmatogenous retinal detachment:
The most common type, occurs when a break, tear, or hole develops in the retina. Liquefied vitreous fluid seeps through the defect, lifting the retina from the back of the eye. Causes include aging, trauma, prior eye surgery, and high myopia. - Tractional retinal detachment:
Caused when scar tissue or abnormal strands (often from diabetes complications) contract and pull the retina off its support. No tear is present, but blood vessel closure, disease, or infection may be underlying triggers. - Exudative retinal detachment:
Develops when fluid accumulates beneath the retina without any hole or tear. Sources of fluid buildup include inflammation, infection, tumors, and conditions like age-related macular degeneration. Also linked to injuries, scleritis, or retinoblastoma.
Symptoms of Retinal Detachment
- Sudden appearance of floaters (small dark shapes or dots)
- Flashes of light in the periphery
- A dark curtain or shadow moving across vision
- Loss of peripheral vision
- Rapid central vision decline if the macula becomes detached
Retinal detachment requires immediate medical attention. Delaying treatment can result in irreversible blindness. If symptoms occur, do not drive – seek emergency eye care promptly.
Causes and Risk Factors for Retinal Detachment
- Aging (vitreous gel changes, thinning retina)
- Severe nearsightedness (myopia)
- Previous eye surgery (e.g., cataract surgery)
- Traumatic injury to the eye or head
- Diabetes complications (especially diabetic retinopathy)
- Eye infections, swelling, or inflammatory diseases
- Retinal vascular disorders and tumors
- Family history of detachment
Treatment Options for Retinal Detachment
Rhegmatogenous Retinal Detachment
- Pneumatic retinopexy: A gas bubble is injected into the eye to help reattach the retina.
- Vitrectomy: Surgical removal of the vitreous gel followed by retinal repair.
- Scleral buckling: A silicone band or sponge is placed against the eye wall to counteract the force pulling on the retina.
- Cryopexy: Freezing treatment to seal retinal tears.
- Laser photocoagulation: Laser surgery to create scar tissue that seals retinal tears and prevents further detachment.
Tractional Retinal Detachment
- Vitrectomy surgery: Removes traction bands, scar tissue, and cloudy vitreous gel.
- Addressing the underlying cause, such as improved diabetes management or treating infections/inflammation.
Exudative Retinal Detachment
- Medical therapy: Corticosteroids or immunosuppressive medications to reduce inflammation.
- Surgical intervention is rare.
- Treatment of the root cause (e.g., tumor or infection).
When to Seek Medical Help
Immediate evaluation is necessary for any sudden changes in vision, especially symptoms of retinal detachment or rapid loss of central vision in macular degeneration. The sooner treatment begins, the higher the chance of saving your sight.
Key Differences: Macular Degeneration vs. Retinal Detachment
| Feature | Macular Degeneration | Retinal Detachment |
|---|---|---|
| Affected Area | Central part of the retina (macula) | Any part of the retina; may include macula |
| Common Symptoms | Loss of central vision, difficulty reading/focusing | Floaters, flashes, peripheral or curtain-like vision loss |
| Progression | Slow (dry), rapid (wet) | Sudden, typically within hours to days |
| Primary Risk Group | Older adults (60+), family history, smokers | Older adults, myopia, diabetes, trauma |
| Treatment | AREDS2 vitamins, anti-VEGF injections, laser | Surgical reattachment, medical management |
Prevention and Eye Health Tips
- Get regular comprehensive eye exams, especially after age 50
- Report any sudden vision changes to your eye doctor immediately
- Maintain good blood sugar and blood pressure control
- Eat a nutrient-rich diet (leafy greens, fish, nuts) supporting retinal health
- Wear UV-protection sunglasses outdoors
- Avoid smoking and manage cholesterol levels
Frequently Asked Questions (FAQs)
Q: Are macular degeneration and retinal detachment related?
While both can cause vision loss, they are distinct conditions. Macular degeneration affects the central retina (macula), causing gradual vision loss, while retinal detachment is the physical separation of the retina, often leading to sudden vision loss. Age-related macular degeneration (AMD) can sometimes increase risk for certain retinal detachments, but they are not directly related.
Q: What is the earliest sign of macular degeneration?
The earliest sign is often blurriness or distortion in the central visual field. People may struggle to read or recognize faces, and colors may appear duller. Presence of drusen noted on dilated eye exam is also an early clinical finding.
Q: How urgent is retinal detachment?
Retinal detachment is a medical emergency. Rapid intervention can save vision, while delays may result in permanent blindness. If you notice a sudden curtain over your vision, flashes, or a sudden increase in floaters, seek care urgently.
Q: Can macular degeneration be reversed?
No, especially the dry type. Certain supplements and lifestyle changes may slow its progression. Wet AMD can sometimes be managed with injections to slow or halt vision loss, but lost vision cannot usually be regained.
Q: Who is most at risk for these conditions?
Individuals over age 60, those with a family history of AMD, smokers, those with high myopia, and people with diabetes or prior eye trauma or surgery are most at risk for both retinal detachment and macular degeneration. Regular eye exams are vital for detecting problems before vision is lost.
Final Thoughts
Early detection, awareness of risk factors, and prompt treatment are essential for preserving vision from macular degeneration and retinal detachment. Consult with an eye care specialist for regular screenings, and maintain a healthy lifestyle to minimize risks. If you experience sudden vision changes, do not delay in seeking professional care.
References
- https://www.healthline.com/health/eye-health/types-of-retinal-detachment
- https://www.ncbi.nlm.nih.gov/books/NBK560778/
- https://theretinainstitute.org/macular-degeneration
- https://my.clevelandclinic.org/health/diseases/15246-macular-degeneration
- https://www.tnretina.com/blog/dr-recchia-talks-to-healthline-on-coats-disease
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1705653/
- https://www.britannica.com/science/macular-degeneration
- https://medlineplus.gov/maculardegeneration.html
Read full bio of Sneha Tete












