Understanding Age-Related Macular Degeneration: Onset, Causes, and Management
Explore the onset, causes, symptoms, and management of age-related macular degeneration to protect your vision as you age.
Understanding Age-Related Macular Degeneration: Age of Onset, Causes, and Management
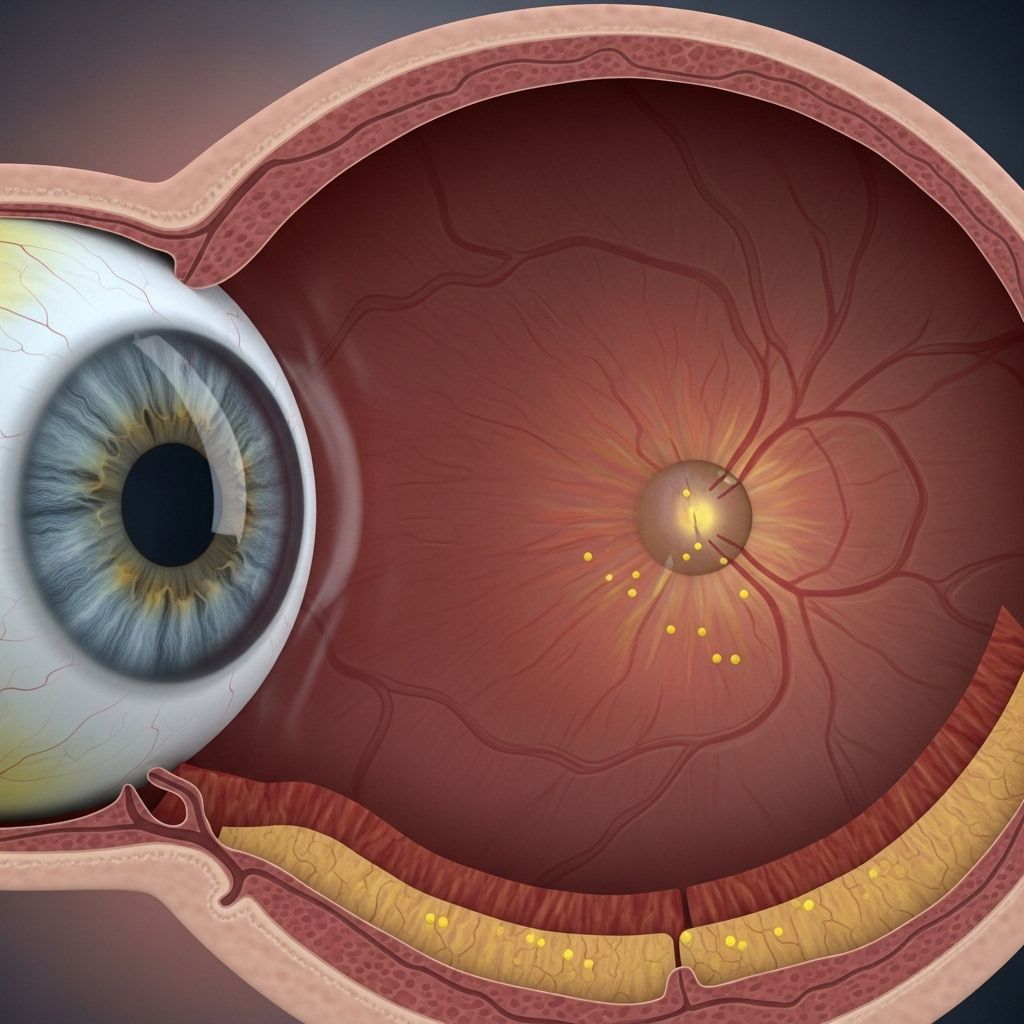
Macular degeneration is a progressive eye disease that commonly affects older adults, leading to the gradual loss of sharp, central vision. The condition occurs as the macula — a small but crucial part of the retina responsible for focused, central sight — deteriorates over time. This article examines at what age macular degeneration typically begins, discusses risk factors, symptoms, diagnostic methods, and treatment options, and provides essential guidance for managing and preventing this common cause of vision loss.
What Is Age-Related Macular Degeneration (AMD)?
Age-related macular degeneration, or AMD, is a leading cause of vision impairment among adults aged 50 years and older. AMD is a chronic, progressive condition that affects the macula, the retina’s central area, which is essential for reading, recognizing faces, driving, and other visual tasks that require fine detail. As AMD advances, central vision is compromised, while peripheral vision is typically preserved.
- Dry (atrophic) AMD: The most common form, accounting for about 85–90% of cases, characterized by gradual thinning of the macular tissue and accumulation of yellow deposits called drusen.
- Wet (neovascular or exudative) AMD: Less common but more severe, involving the growth of abnormal blood vessels under the macula, which may leak fluid or blood and cause sudden vision loss.
At What Age Does Macular Degeneration Typically Begin?
AMD is strongly associated with aging and rarely develops before age 50. The risk increases significantly as people get older:
- Early signs may develop in people in their 50s or 60s, often without noticeable symptoms.
- Most diagnoses occur after age 60, with the likelihood rising steeply in those over 75.
- Approximately 14% of adults over 80 are affected, with cases rising among longer-living populations.
While age remains the most critical risk factor, certain rare forms of juvenile macular degeneration — such as Stargardt disease — may occur in children and young adults.
Symptoms and Early Warning Signs
Macular degeneration often develops without pain and may not cause noticeable vision changes in the earliest stages. As the disease progresses, people may notice:
- Blurriness or distortion in central vision
- Difficulty reading or recognizing faces
- Need for brighter light for tasks such as reading
- Faded or less vivid colors
- Dark or empty areas in the center of vision
- Straight lines appearing wavy (metamorphopsia)
For those with wet AMD, symptoms may appear rapidly and can include sudden, dramatic changes in vision, sometimes over days or weeks.
Main Causes and Risk Factors
The exact cause of AMD is not fully understood, but multiple factors contribute to its development. The most significant include:
- Aging: The leading risk factor, with risk climbing after age 50.
- Genetics: Family history of AMD increases risk.
- Race: Individuals of European descent have higher prevalence rates; AMD is less common in African-American and Hispanic populations.
- Smoking: Significantly increases the likelihood of AMD.
- Cardiovascular disease: High blood pressure, high cholesterol, and atherosclerosis increase risk.
- Obesity and physical inactivity
- Poor diet: Low intake of leafy greens, antioxidants, and omega-3 fatty acids
- Excessive sun exposure
How Common Is Macular Degeneration?
AMD is the most frequent cause of central vision loss in older adults within developed countries. It is responsible for over 50% of vision impairment among non-Hispanic white populations in the United States. Prevalence sharply rises with age:
- Roughly 2% of people aged 40-49
- About 5% of those aged 60-69
- 14% or more by age 80
| Age Group | Estimated Prevalence |
|---|---|
| 40–49 years | ~2% |
| 60–69 years | ~5% |
| 80+ years | ~14% |
Different Types of Macular Degeneration
AMD is typically classified into two categories:
- Dry (Atrophic) AMD: Gradual breakdown of the macula, marked by drusen build-up and slow vision decline.
- Wet (Exudative/Neovascular) AMD: Abnormal blood vessels develop under the retina, leaking fluid or blood and causing more severe, sudden, and rapid vision loss. Responsible for most cases of advanced, central vision loss.
Other less common types include juvenile macular degeneration (e.g., Stargardt disease) affecting younger individuals.
Dry AMD Progression
- Early-stage: Few small or medium drusen, usually with no vision loss.
- Intermediate-stage: More drusen or pigment changes, possible mild vision symptoms.
- Advanced-stage (Geographic Atrophy): Large areas of retinal degeneration, more pronounced vision loss.
Wet AMD Progression
- Characterized by the appearance of abnormal, leaky blood vessels under the retina.
- Can cause rapid and severe damage — sometimes in days or weeks.
- Accounts for the majority of cases of legal blindness due to AMD.
Diagnosis
Early diagnosis can help slow the progression of AMD and improve quality of life. Eye care professionals typically use the following methods:
- Dilated eye exam: Eye drops are used to widen the pupil for a better view of retinal structures.
- Retinal imaging: Special cameras detect the presence of drusen, changes in pigmentation, or abnormal blood vessels.
- Amsler grid: A simple test to identify central distortion or missing vision.
- Optical coherence tomography (OCT): A noninvasive imaging technique that provides detailed cross-sectional images of the retina.
- Fluorescein angiography: For wet AMD, this test uses a dye to highlight leaky or abnormal blood vessels.
Regular comprehensive eye exams are crucial, particularly if you are over 50 or have risk factors for AMD.
Treatment Options and Disease Management
Currently, no treatment can reverse macular degeneration, but medical interventions and lifestyle adjustments can help slow disease progression and preserve vision for as long as possible.
Treatments for Dry AMD
- AREDS2 vitamin supplements: A specific formulation of vitamins and minerals (vitamin C, vitamin E, zinc, copper, lutein, and zeaxanthin) shown to reduce risk of advanced AMD in some people with moderate disease.
- Monitoring: Routine exams, self-monitoring with the Amsler grid.
- Healthy lifestyle: Managing blood pressure, eating an antioxidant-rich diet, and not smoking.
There is no approved therapy for early-stage dry AMD, but some new medications such as injectables (e.g., Izervay) may help slow the progression of advanced forms.
Treatments for Wet AMD
- Anti-VEGF therapy: Regular injections into the eye that block vascular endothelial growth factor (VEGF), slowing or stopping the growth of abnormal blood vessels.
- Examples of anti-VEGF drugs: ranibizumab, aflibercept, bevacizumab.
- Photodynamic therapy: Uses a laser and light-sensitive drug to close abnormal blood vessels.
- Laser surgery: Less commonly used, but can destroy abnormal vessels if detected early.
Early intervention is especially crucial for wet AMD to minimize vision loss.
Prevention and Lifestyle Considerations
While some risk factors for AMD cannot be changed, adopting healthy habits can reduce the likelihood of developing the condition and slow its progression:
- Do not smoke or quit smoking
- Eat a balanced diet high in leafy greens, colorful fruits and vegetables, and omega-3 fatty acids
- Maintain a healthy weight and exercise regularly
- Manage chronic diseases, especially high blood pressure and cardiovascular disease
- Wear sunglasses and a wide-brimmed hat to protect eyes from UV light
- Get regular comprehensive eye exams, especially after age 50 or with family history
Living with Macular Degeneration
Vision loss from AMD can significantly impact lifestyle, but advances in low vision aids, adaptations, and support services enable many people to maintain independence. Some practical tips include:
- Using magnifying devices or electronic readers
- Improving lighting throughout the home
- Exploring vision rehabilitation resources
- Regularly consulting with eye care professionals about new treatments and coping strategies
Frequently Asked Questions (FAQs)
Q: Is macular degeneration inevitable as I age?
A: While age is the strongest risk factor, many people never develop AMD. By controlling other risk factors, you can lower your risk.
Q: Can macular degeneration be reversed?
A: No current treatment can reverse AMD, but medical therapy and lifestyle changes can slow its progression and help preserve vision.
Q: How quickly does AMD cause vision loss?
A: Dry AMD progresses slowly over years, while wet AMD can cause significant vision loss rapidly — sometimes within weeks.
Q: What is the difference between wet and dry macular degeneration?
A: Dry AMD involves gradual thinning of retinal cells and drusen accumulation, causing slow vision decline. Wet AMD is marked by abnormal blood vessel growth, leading to leakage, scarring, and faster vision loss.
Q: Are there specific foods that help prevent AMD?
A: Diets rich in leafy greens, colorful vegetables, fruits, fish high in omega-3s, and low in saturated fat may help reduce risk. Supplements based on AREDS2 guidelines are sometimes recommended for those at higher risk.
Q: Should I get screened for AMD if I have no symptoms?
A: Regular eye exams are vital for early detection, especially for those over 50 or with a family history. Early AMD often has no symptoms, so routine screening is the best defense.
The Takeaway
Age-related macular degeneration is a leading cause of vision loss in older adults. While the disease cannot be cured, understanding your risk, maintaining regular eye care, and making healthy lifestyle choices can help you protect your sight. Early detection and appropriate management are crucial for preserving vision and maintaining quality of life as you age.
References
- https://www.medicalnewstoday.com/articles/can-macular-degeneration-be-reversed
- https://theretinainstitute.org/macular-degeneration
- https://www.healthline.com/health/eye-health/macular-degeneration-types
- https://www.medicalnewstoday.com/articles/exudative-macular-degeneration
- https://www.ncbi.nlm.nih.gov/books/NBK315804/
- https://www.britannica.com/science/macular-degeneration
- https://medlineplus.gov/maculardegeneration.html
Read full bio of Sneha Tete












