Lung Nodule Size Chart: Understanding Risks, Diagnosis, and Next Steps
A thorough, medically reviewed guide exploring lung nodule sizes, cancer risk, diagnosis, and prevention considerations.
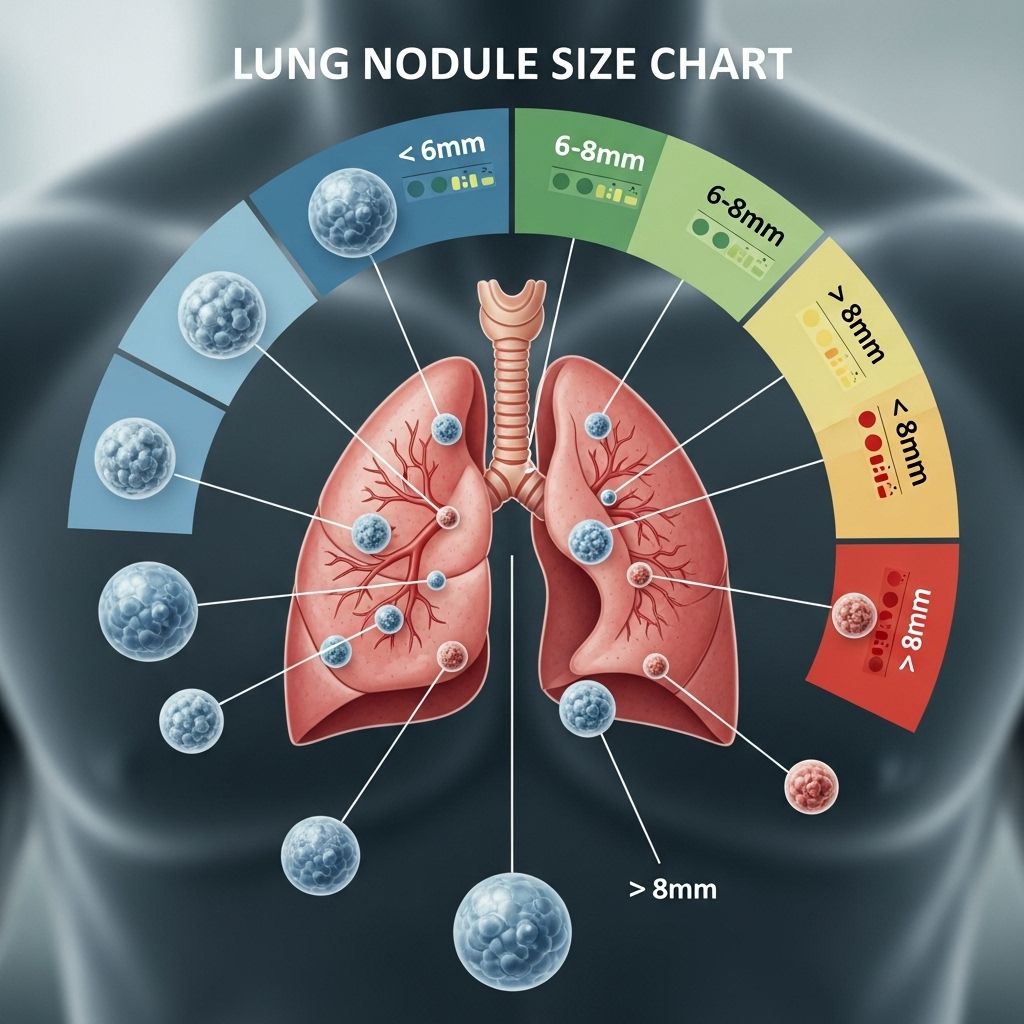
Lung nodules are small, rounded growths in the lungs, commonly discovered incidentally during imaging for unrelated conditions. The risk of cancer varies notably by nodule size, with most being harmless but some requiring further follow-up and, occasionally, removal. This guide presents an in-depth look at lung nodule sizes, relevant risks, diagnostic approaches, treatment options, and preventive strategies.
What Is a Lung Nodule?
A lung nodule is an irregular, rounded mass of tissue in the lung with a diameter less than 30 millimeters (mm) (about 1.2 inches). Nodules are extremely common, occurring in approximately 2% to 24% of the general population. Most lung nodules are found incidentally during chest X-rays or computerized tomography (CT) scans performed for other reasons.1
While many lung nodules are not cancerous, risk assessment relies heavily on nodule size, its growth rate, shape, composition, and pattern of calcification. Noncancerous causes include infections, inflammation from autoimmune disease (like rheumatoid arthritis), and benign tumors such as hamartomas.1
Key Points:
- Lung nodules under 30 mm in diameter are classified as nodules.
- Nodules above 30 mm are considered lung masses and are more likely to be cancerous.
Lung Nodule Sizes and Associated Cancer Risks
Assessing risk is predominantly based on nodule diameter. The Fleischner Society guidelines are the primary reference point for medical professionals. These guidelines address management strategies for various nodule sizes, accounting for growth rate and tissue composition, but notably do not apply to people under 35 or those with a history of cancer or immunosuppression.1
What’s Considered a Small Lung Nodule?
Small nodules are defined as those less than 10 mm in diameter, with nodules under 3 mm labeled as micronodules.1
| Diameter | Risk of Being Cancerous |
|---|---|
| 1 to 2 mm | Routine finding; very small risk |
| Less than 6 mm | 0% to 1% |
| 6 to 8 mm | 0.5% to 2% |
| More than 8 mm | ~9.7% |
| More than 10 mm | ~15.2% |
Most nodules smaller than 10 mm are only visible on CT scans and not detectable on chest X-rays.
What’s Considered a Large Lung Nodule?
Lung nodules over 10 mm in diameter are considered large. The risk of malignancy climbs with size:1,2
| Diameter | Risk of Being Cancerous |
|---|---|
| More than 10 mm | ~15.2% |
| More than 30 mm | Usually assumed cancerous (considered a lung mass) |
Larger nodules, and especially those termed “masses,” often require more extensive testing or immediate treatment due to the increased risk of malignancy.
Other Risk Factors Affecting Cancer Probability
- Growth rate: Nodules that increase in size over follow-up imaging are more likely to be cancerous.3
- Imaging patterns: Irregular shape, spiculated borders, or non-uniform calcification may indicate higher cancer risk.4
- Tissue composition: Solid nodules carry a higher suspicion for malignancy than ground-glass or partially solid ones.1,3
- Personal history: Individuals with previous lung cancer, immunosuppression, or those over age 35 are at greater risk.1
When Should You Be Concerned About a Lung Nodule?
While most detected nodules are benign, factors that heighten concern include:
- Nodule diameter above 6 mm, especially growing nodules
- Presence of symptoms such as persistent cough, hemoptysis (coughing up blood), chest pain, or shortness of breath
- Irregular shape or border on imaging
- History of smoking, lung cancer, or exposure to known carcinogens
- Age over 35, immunosuppression, or other risk factors for malignancy
Doctors may recommend more frequent monitoring or invasive diagnostic tests for nodules that meet these risk criteria.1,3
Next Steps After Finding a Lung Nodule
Upon discovering a lung nodule, your healthcare team considers multiple aspects before suggesting a management plan. Key steps include:
- Reviewing old imaging studies: If the nodule has not grown since previous scans, the likelihood of cancer decreases.2
- Surveillance: Small, stable nodules might only require periodic CT scans for monitoring.
- Further diagnostic tests: For higher-risk nodules, options include PET/CT scans, bronchoscopy, biopsy, or surgical sampling.3
Biopsies of lung nodules are reserved for cases where the perceived cancer risk justifies the procedure. Risks of biopsy include bleeding, infection, and rarely, a collapsed lung.2
Common Diagnostic Modalities:
- CT Scan: Preferred imaging for nodule assessment, helping determine size, growth, and characteristics.
- PET/CT Scan: Useful for evaluating metabolism; higher uptake suggests malignancy.
- Biopsy: Tissue sampling may be performed if malignancy cannot be excluded.
- Bronchoscopy or surgical tissue sample: If precise location allows, these may be utilized.
Lung Nodule Removal and Treatment Options
Most small, stable, and asymptomatic nodules do not require removal and are simply tracked over time. However, nodules that grow, are large (typically above 8 or 10 mm), or have suspicious imaging characteristics may require additional intervention:
- Minimally invasive surgery: Video-assisted thoracoscopic surgery (VATS) removes the nodule and provides tissue for diagnosis.
- Traditional open surgery: May be needed for nodules in difficult-to-access locations or when more extensive tissue needs sampling.
- Non-surgical options: If surgery is not possible, alternative treatments may be considered depending on the individual’s health status.
Patients with confirmed lung cancer will receive a personalized treatment plan from their oncology team, potentially involving surgery, radiation, chemotherapy, or immunotherapy.3
Prevention Strategies for Lung Nodules and Lung Cancer
You can lower your risk of developing lung nodules and lung cancer by:
- Not smoking: The number one preventive measure for lung cancer and related nodules.
- Reducing exposure to carcinogens: Minimize exposure to radon, asbestos, and air pollutants.
- Managing chronic illnesses: Control autoimmune diseases and respiratory infections.
- Routine checkups: Especially for higher-risk populations.
Frequently Asked Questions (FAQs)
Q: Are all lung nodules cancerous?
A: No, the vast majority—at least 95%—of lung nodules are benign. Most are caused by infection, inflammation, or harmless tissue growths.
Q: What does a micronodule mean in lung imaging?
A: A micronodule refers to a lung nodule smaller than 3 mm in diameter and generally carries an extremely low risk of cancer.
Q: How often do lung nodules turn out to be cancerous?
A: Of all lung nodules detected, approximately 5% are cancerous. The risk increases with nodule size and other factors.
Q: What will my doctor do if a lung nodule is found?
A: Your doctor will review your scans, assess risk factors, and may order further imaging or a biopsy, especially if the nodule is larger or has concerning features.
Q: Can lung nodules cause symptoms?
A: Most lung nodules do not cause symptoms. Larger or cancerous nodules may lead to coughing, chest pain, shortness of breath, or coughing up blood.
Q: Is it possible to prevent lung nodules?
A: While some lung nodules are unavoidable, not smoking and minimizing exposure to environmental toxins can help reduce your risk.
Summary
Lung nodules are common, often benign, and usually discovered incidentally on imaging. The risk of cancer rises with nodule size and suspicious imaging features, prompting careful evaluation and sometimes surgical removal. Proactive management, regular follow-up, and lifestyle choices such as avoiding smoking and carcinogens can reduce your lung cancer risk and facilitate early detection and treatment.
References
- https://www.healthline.com/health/lung-cancer/lung-nodule-size-chart
- https://www.cancercenter.com/cancer-types/lung-cancer/risk-factors/lung-nodules
- https://www.healthline.com/health/lung-cancer/lung-nodule
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6784443/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6178302/
- https://www.aafp.org/pubs/afp/issues/2023/0300/pulmonary-nodules.html
- https://www.medicalnewstoday.com/articles/317531
- https://www.thoracic.org/patients/patient-resources/resources/lung-nodules-online.pdf
Read full bio of medha deb












