Lung Cancer and White Blood Cell Count: What You Need to Know
Understand how white blood cell counts relate to lung cancer risk, diagnosis, treatment side effects, and overall health considerations.
Lung Cancer and White Blood Cell Count: Frequently Asked Questions
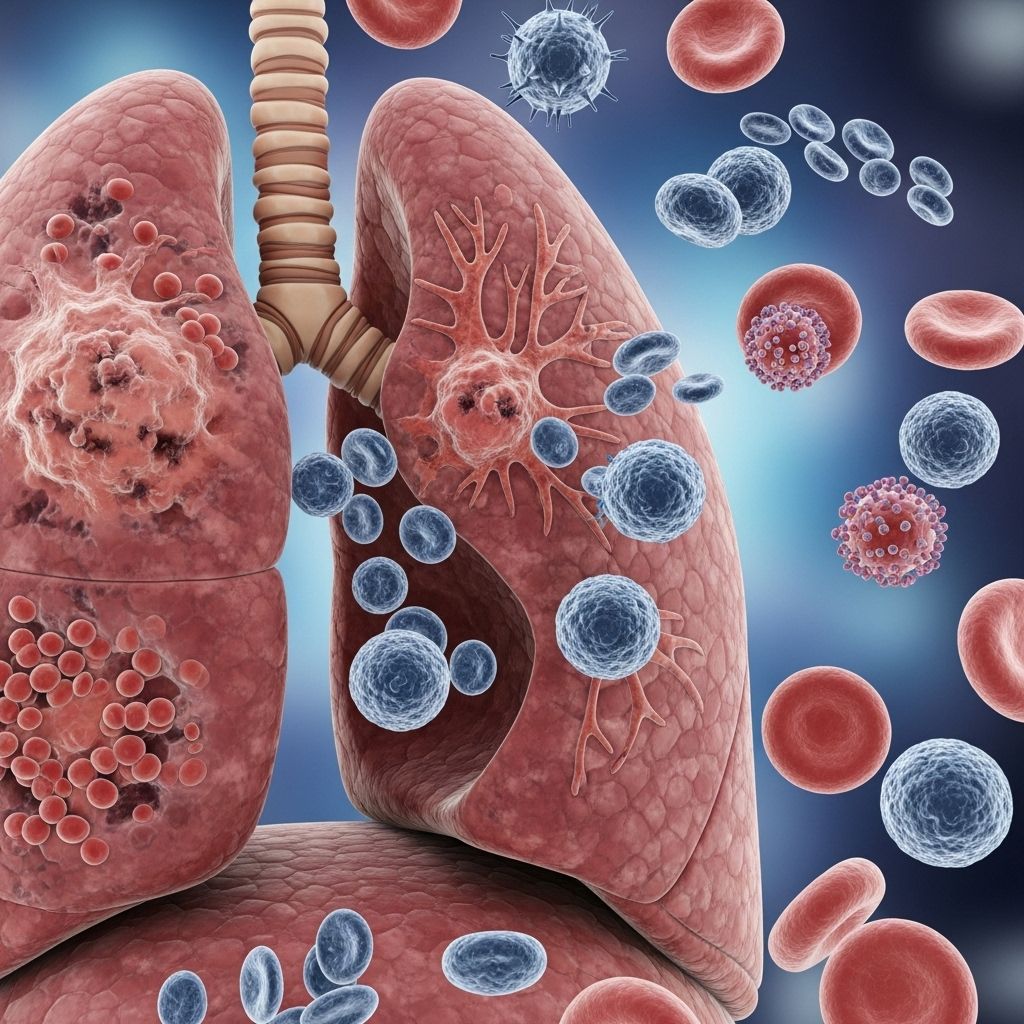
Lung cancer is a complex disease that directly and indirectly affects many aspects of the body, including the immune system. One area receiving growing attention is the relationship between white blood cell (WBC) counts and lung cancer. Understanding what changes in white blood cell count may signal, how treatments can impact your WBCs, and what these results might mean for your care is important for patients and families. Here, we answer the most common questions regarding lung cancer and white blood cell counts, drawing from the latest research and clinical experience.
What Are White Blood Cells?
White blood cells (also called leukocytes) are essential components of the immune system, tasked with defending the body against infections, inflammation, and foreign invaders. There are several types of white blood cells, each playing a unique role in immune response:
- Neutrophils: The most abundant type, crucial for fighting bacterial and fungal infections.
- Lymphocytes: Includes T-cells and B-cells, important for targeting viruses and abnormal (including cancerous) cells.
- Monocytes: Help remove pathogens and dead cells from tissues.
- Eosinophils: Combat multicellular parasites and are involved in allergic responses.
- Basophils: Release chemicals involved in inflammation and allergic responses.
Normal WBC counts vary by age, sex, and individual factors but generally range from 4,000 to 11,000 cells per microliter of blood in adults.
Why Do Doctors Monitor White Blood Cell Count in Lung Cancer?
Physicians routinely monitor white blood cell counts during the diagnosis and treatment of lung cancer for several reasons:
- To assess overall immune function
- To detect infections or an increased risk of developing them
- To track side effects from treatments like chemotherapy and radiation
- As a possible marker of disease activity or progression
White blood cell counts can help guide treatment choices, signal complications, or prompt further investigation if unexpectedly high or low.
How Can Lung Cancer Affect White Blood Cell Count?
Lung cancer can influence white blood cell counts in several ways:
- Tumor-Related Inflammation: Some tumors produce substances that stimulate bone marrow to make more WBCs, leading to elevated counts.
- Immune System Activation: Chronic inflammation due to cancer can cause persistently high WBC counts.
- Bone Marrow Infiltration: In rare cases, lung cancer may spread to the bone marrow, impairing the body’s ability to produce healthy blood cells, resulting in abnormal or low WBC counts.
Does a High White Blood Cell Count Mean I Have Lung Cancer?
No, a high white blood cell count does not always mean you have lung cancer. Elevated WBC counts may occur due to many reasons, including:
- Infections (such as bacterial, viral, or fungal infections)
- Inflammatory conditions (like rheumatoid arthritis, allergies, or asthma)
- Stress
- Other medical conditions (such as autoimmune diseases or use of corticosteroids)
That said, recent research suggests that a persistent elevation in white blood cell counts, particularly in certain subtypes like neutrophils and monocytes, may correlate with an increased risk of developing lung cancer, especially lung adenocarcinoma and among smokers. However, it is not specific enough to serve as a stand-alone diagnostic test for cancer.
Is a Low White Blood Cell Count Common in Lung Cancer?
A lower-than-normal white blood cell count (leukopenia) is commonly seen during cancer treatment, such as chemotherapy, rather than from the cancer itself. Chemotherapy targets rapidly dividing cells, including those in bone marrow, which reduces the number of new white blood cells being made. This can lead to a dangerously low WBC count, especially of neutrophils (neutropenia).
- Symptoms of low WBC:
- Frequent infections
- Fever or chills
- Sore throat
- Mouth sores
- Fatigue or weakness
What Do Research Studies Say About WBC Counts and Lung Cancer Risk?
Several large-scale studies have explored the connection between white blood cell count and the likelihood of developing lung cancer:
- Genetic studies: Mendelian randomization studies show that higher genetic variants linked to increased total WBC and especially monocyte counts are associated with increased risk for lung adenocarcinoma (LUAD).
- Epidemiological studies: Prospective cohort studies in the UK have shown that an increased total WBC count is a risk marker for lung cancer, particularly in current and past smokers, and is driven most by high neutrophil levels.
- Physical activity: Studies also indicate that low physical activity and elevated WBCs are independent risk factors for lung cancer.
However, an elevated WBC count is only one of many risk factors, and most people with high WBC counts do not develop cancer.
Can White Blood Cell Counts Be Used to Diagnose Lung Cancer?
White blood cell counts are not used as a screening or diagnostic tool for lung cancer. While changes may raise suspicion for infection or treatment side effects, they are not reliable enough for cancer diagnosis. Instead, the primary diagnostic methods include:
- Imaging tests (such as chest X-ray or CT scan)
- Tissue biopsy
- Other laboratory assessments (looking for tumor markers, etc.)
WBC counts may play a supportive role in guiding the need for further evaluation, especially when combined with other symptoms and risk factors.
How Does Chemotherapy Affect White Blood Cell Count?
Chemotherapy primarily targets rapidly dividing cells, including fast-growing cancer cells but also impacts healthy cells in the bone marrow—where blood cells are made. This often leads to a temporary drop in white blood cell production, especially neutrophils. This effect is called neutropenia.
- Time course: Neutropenia typically occurs 7-14 days after each chemotherapy cycle.
- Risks: Increases susceptibility to infections, which can quickly become severe.
Doctors monitor the absolute neutrophil count (ANC) closely and may delay or adjust chemotherapy if counts are too low.
What About Radiation Therapy and Immunotherapy?
Other cancer treatments also impact blood cell counts:
- Radiation therapy: Especially when directed at bones (like the spine, pelvis, or ribs), can reduce WBC production.
- Immunotherapy: Can alter immune cell function; may paradoxically increase risk for certain infections or, rarely, cause autoimmune-like drops in blood cell counts.
Managing low white blood cell counts is a priority during all types of cancer treatment.
How Is Low WBC (Neutropenia) Managed During Lung Cancer Treatment?
Managing and preventing complications from low white blood cell counts is key for safe cancer treatment:
- Growth factor medications: Drugs such as filgrastim or pegfilgrastim stimulate the production of neutrophils.
- Adjustments in chemotherapy: Dose reductions or treatment delays until counts recover.
- Antibiotic or antifungal medications: Preventive medicines may be given during high-risk periods.
- Good hygiene: Frequent handwashing, avoiding crowds or sick contacts, and prompt medical attention for fevers or signs of infection.
What Symptoms Should Prompt Medical Attention?
Cancer patients with low WBC counts should be vigilant for signs of infection or other complications. Immediate medical attention is needed for:
- Fever over 100.4°F (38°C)
- Chills or sweating
- Sore throat or new cough
- Shortness of breath
- Pain, redness, or swelling
- Unusual fatigue, confusion, or weakness
Infections during neutropenia can become dangerous rapidly. Hospitalization and intravenous antibiotics may be required.
Can You Do Anything to Influence Your WBC Count?
Keeping your immune system as healthy as possible may help maintain a stable WBC count. General recommendations include:
- Balanced nutrition, high in protein, vitamins, and minerals
- Physical activity, as tolerated (shown to independently lower lung cancer risk)
- Avoiding exposure to infectious agents
- No smoking and avoiding secondhand smoke
- Regular medical follow-up
Discuss specific strategies and limitations with your oncology team.
Common Terms Related to White Blood Cell Count and Lung Cancer
| Term | Definition |
|---|---|
| Leukocytosis | An abnormally high white blood cell count |
| Leukopenia | An abnormally low white blood cell count |
| Neutropenia | A dangerously low count of neutrophils (a type of WBC) |
| ANC (Absolute Neutrophil Count) | The specific number of neutrophils found in blood, vital for infection risk monitoring |
| Lymphocytes | White blood cells important in targeting virus-infected or cancer cells |
| Monocytes | WBCs that help remove pathogens and dead cells; high count may indicate infection or inflammation |
Frequently Asked Questions (FAQs)
Does a significant change in my white blood cell count mean my lung cancer is worsening?
Not necessarily. Many factors, including infections, medications, stress, or even laboratory variation, can affect WBC levels. However, a persistent, unexplained elevation or drop in WBCs may warrant further investigation for disease progression or complications. Always discuss changes with your care team.
Can high or low WBC counts affect treatment decisions?
Yes, especially during chemotherapy or immunotherapy. If your counts are too low, your oncologist may delay or adjust your treatment to prevent serious infection. Growth factor medications may be prescribed to help boost your counts.
Is there a difference in WBC counts and lung cancer in smokers versus non-smokers?
Studies show a stronger association between elevated WBC counts and lung cancer risk in smokers, especially men. However, increased risk is also observed in never-smoking women. The role of WBCs in non-smokers may relate more to genetic factors or underlying mutations in cancer pathways.
Are certain WBC types more important in lung cancer risk?
Yes; research indicates that elevated neutrophils and monocytes are particularly linked with higher lung adenocarcinoma risk.
Can physical activity or lifestyle changes lower my risk?
Evidence suggests that physical activity and avoiding smoking both independently reduce lung cancer risk, possibly through their effects on inflammation and immune function.Focus on a healthy lifestyle and regular checkups.
What should I ask my doctor about my white blood cell count?
- What do my current WBC results mean for my specific case?
- How often will my blood counts be monitored during treatment?
- What symptoms should I watch out for?
- What steps can I take to reduce infection risk?
- Will I need medication to raise my WBC count if it drops?
Summary
White blood cell counts are an important marker of health in people with lung cancer. Elevations in certain WBC subtypes may modestly increase risk for developing lung cancer, particularly adenocarcinoma and among smokers. Cancer therapies like chemotherapy commonly lower WBC counts, increasing infection risk and sometimes requiring adjustments in care. Monitoring, prevention, and prompt response to complications form the backbone of safe treatment. Always address concerns about your WBC with your care team—they will help put your results in the context of your overall health and treatment plan.
References
- https://www.nature.com/articles/s41598-025-88366-w
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7083262/
- https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/1097-0142(20011101)92:9%3C2399::AID-CNCR1588%3E3.0.CO;2-W
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2692679/
- https://www.mylungcancerteam.com/resources/lung-cancer-and-neutropenia-what-to-know
- https://medlineplus.gov/ency/patientinstructions/000675.htm
- https://www.ukbiobank.ac.uk/publications/white-blood-cell-count-and-risk-of-incident-lung-cancer-in-the-uk-biobank/
Read full bio of Sneha Tete












