Lung Cancer Images, Types, and Diagnosis Explained
Explore how lung cancer appears in imaging, its types, common signs, diagnostic techniques, and key facts through a detailed overview.
Lung Cancer: What Does it Look Like?
Lung cancer is among the most common and serious forms of cancer worldwide. Timely identification and understanding of its visual presentation through various diagnostic images are crucial for treatment and prognosis. This comprehensive article examines what lung cancer looks like on imaging tests, explores the main types, diagnostic approaches, and answers frequently asked questions.
Overview of Lung Cancer
Lung cancer arises when abnormal cells in one or both lungs grow uncontrollably. This unchecked growth can form masses (tumors) that interfere with normal lung function, sometimes spreading to other parts of the body. According to recent data, an estimated 238,340 people in the United States were expected to be diagnosed with lung cancer by the end of 2023. Despite its seriousness, improved screening and treatment options continue to offer hope for early detection and effective management.
- Lung cancer is the second most common cancer in both men and women in the U.S.
- The rate of new cases is decreasing, partly due to greater awareness, healthier lifestyles, and advanced treatments.
- There are two primary types: non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC).
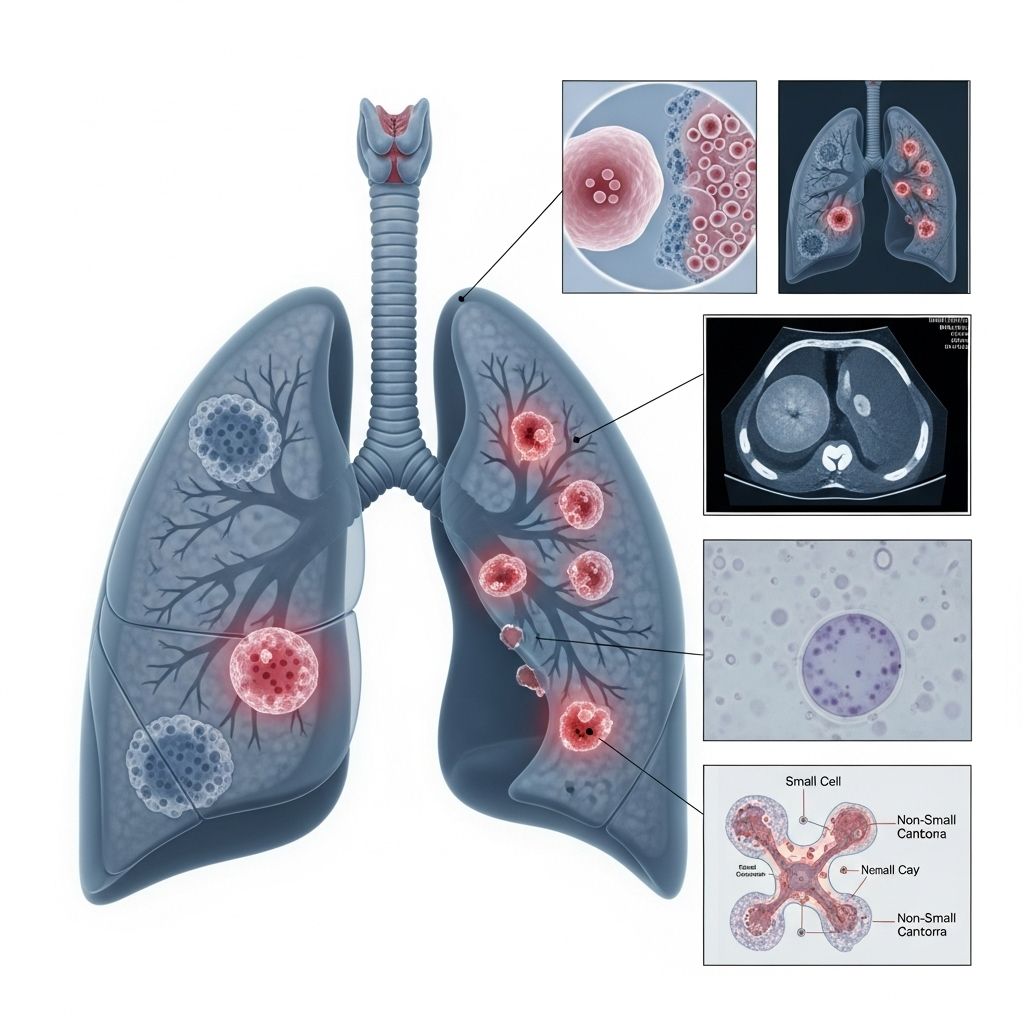
What Does Lung Cancer Look Like on Imaging?
For people suspected of having lung cancer, imaging tests are among the first steps in the diagnostic process. These tests not only help in initial detection but also guide treatment by determining the cancer’s size, location, and potential spread.
Chest X-ray
A chest X-ray is usually the first imaging test recommended if lung cancer is suspected. On an X-ray, lung cancer may appear as a distinct mass or nodule, represented by a white spot or shadow against the normally black background of air-filled lungs. Not every white spot signals cancer; other causes include benign (non-cancerous) nodules from infections or inflammation.
- The mass or nodule visible on an X-ray can vary in shape and size.
- Some cancers may cause atelectasis (lung collapse) or fluid build-up, seen as dark or hazy regions.
However, chest X-rays alone may not always detect very small or early-stage cancers, making it important for doctors to use further imaging tests for a definitive assessment.
CT Scan
Computed tomography (CT) scans provide more detailed, cross-sectional images compared to X-rays. CT scans can reveal:
- Solid tumors or masses, sometimes surrounded by smaller nodules
- Irregular or diffuse patterns of abnormal lung tissue
- Enlarged lymph nodes in the chest
- Fluid accumulation (pleural effusion)
A CT scan also aids in detecting cancer spread (metastasis) to other areas, such as bones or the liver. When cancer progresses, recurring scans may show new nodules or enlargement of existing ones, and involvement of nearby organs, including the heart, chest wall, or major blood vessels.
| Imaging Test | Findings Associated with Lung Cancer |
|---|---|
| Chest X-ray | White mass/nodule, dark patches (collapse), fluid shadows |
| CT Scan | Solid tumor(s), enlarged lymph nodes, fluid, tissue changes |
| PET Scan | Detects metabolic activity; highlights spread to lymph nodes & distant organs |
| MRI/Bone Scan/Ultrasound | Checks for metastasis to brain, bone, liver, or adrenal glands |
Images and Visual Presentations
While real diagnostic images are only available to clinicians, visual descriptions are useful for general understanding:
- Masses or Nodules: Look like solid, clearly visible white or gray spots in the lung field.
- Collapsed Areas: Appear darker due to the absence of air in affected regions.
- Fluid Build-up: Results in hazy, white shadows at lung bases or around the edges.
Types of Lung Cancer
Lung cancers fall into two major categories based on the cells involved and their microscopic appearance:
Non-Small Cell Lung Cancer (NSCLC)
- Accounts for about 80–85% of lung cancer cases.
- Includes subtypes such as adenocarcinoma, squamous cell carcinoma, and large cell carcinoma.
- Tends to grow and spread more slowly than small cell carcinoma.
Small Cell Lung Cancer (SCLC)
- Makes up 10–15% of lung cancer cases.
- Noted for its aggressive growth and early widespread metastasis.
- Treatment often involves chemotherapy and radiation rather than surgery.
Both types can present with various shapes and sizes on imaging, but their biological behavior and response to treatment differ.
Common Symptoms and Signs of Lung Cancer
Early lung cancer may not cause noticeable symptoms. When they do occur, they often resemble other less severe conditions, making early diagnosis challenging. Watch for:
- Persistent cough (sometimes worsening over time)
- Coughing up blood or rust-colored sputum
- Chest pain or discomfort
- Hoarseness or voice changes
- Shortness of breath and wheezing
- Frequent lung infections (bronchitis, pneumonia)
- Unexplained weight loss and appetite loss
- Constant fatigue
Advanced or metastatic lung cancer may result in:
- Bone pain or fractures
- Neurological symptoms (headaches, weakness)
- Swelling in lymph nodes, especially around the neck or above the collarbone
- Jaundice (yellowing of the skin/eyes) if the liver is involved
How Lung Cancer Is Diagnosed
Diagnosing lung cancer involves several integrated steps, starting from clinical evaluation and imaging, to laboratory and tissue sampling tests.
Imaging Tests for Lung Cancer Detection
- Chest X-ray: Often the first test performed, revealing suspicious masses.
- CT Scan: Gives detailed cross-sections of the chest, helping characterize the mass more precisely.
- PET Scan: Highlights potentially active cancerous regions, even in distant organs.
- MRI/Bone Scans: Used to check for metastatic spread to the brain or bones.
Tissue Sampling and Biopsy
Imaging tests cannot always definitively distinguish benign from malignant growths or identify the cancer subtype. A biopsy—examining tissue under a microscope—is necessary for a conclusive diagnosis. This can involve:
- Fine needle aspiration: Using a thin needle to remove cells from the suspicious area (sometimes guided by imaging)
- Bronchoscopy: Inserting a flexible tube into the airways to collect tissue or cells
- Surgical biopsy: More invasive techniques (e.g., thoracoscopy) are used for hard-to-access tumors
Other Laboratory Tests
- Pleural fluid analysis: Examining fluid that accumulates around the lungs for cancer cells
- Sputum cytology: Checking mucus from deep coughs for abnormal cells
- Blood tests: Assisting in overall assessment but not usually able to diagnose lung cancer on their own
Staging: How Extensive Is the Cancer?
Once lung cancer is diagnosed, it needs to be staged—determined how far it has spread in the body. The primary staging systems include:
- Localized: Cancer confined within a limited lung area
- Regional: Spread to nearby tissues or lymph nodes
- Distant (metastatic): Cancer has spread to distant organs or lymph nodes
The TNM system (Tumor, Node, Metastasis) offers a more detailed staging description combining the size of the primary tumor, involvement of lymph nodes, and presence of distant spread.
Limitations of Imaging and Tests
While imaging and laboratory tests have revolutionized early detection, they have some limitations:
- Imaging alone cannot differentiate all cancer types or confirm malignancy; benign infections or inflammations can mimic cancer appearance.
- Some early or small cancers might be missed, particularly in asymptomatic individuals.
- False positives can occur, requiring further invasive tests like biopsy for definitive diagnosis.
Currently, only a tissue biopsy can definitively confirm the presence and specific type of lung cancer.
Frequently Asked Questions (FAQs)
Q: What are the main risk factors for developing lung cancer?
A: Cigarette smoking is the most important risk factor, but air pollution, occupational exposures, family history, and a history of certain lung diseases also contribute.
Q: Is lung cancer always visible on a chest X-ray?
A: No, not all lung cancers are visible on a chest X-ray, especially in early stages or for small tumors. Additional imaging, such as CT scans, may be needed for detection.
Q: How often should high-risk individuals undergo lung cancer screening?
A: The U.S. Preventive Services Task Force recommends annual screening with low-dose CT scans for individuals aged 50 to 80 who have a significant smoking history and currently smoke or quit within the past 15 years.
Q: Can a lung nodule seen on imaging be non-cancerous?
A: Yes, many nodules are benign, often caused by previous infections or inflammation. Further tests, including biopsies, are needed to determine if a nodule is cancerous.
Q: What are the latest advances in lung cancer treatment?
A: Treatments continue to evolve, with options such as targeted therapies, immunotherapy, and minimally invasive surgical techniques showing promising results alongside traditional chemotherapy and radiation.
Key Takeaway
Lung cancer remains a major cause of cancer death, but increasing awareness, early detection through modern imaging techniques, and evolving treatments are improving outcomes. If you have symptoms or risk factors, discuss screening options with your healthcare provider and seek medical evaluation promptly if you notice any persistent changes in your respiratory health.
References
- https://www.patientpower.info/lung-cancer/what-does-lung-cancer-look-like
- https://www.healthline.com/health/lung-cancer/pictures
- https://www.medicalnewstoday.com/articles/323701
- https://www.healthline.com/health/lung-cancer
- https://www.britannica.com/science/lung-cancer
- https://www.chp.gov.hk/en/static/80049.html
- https://www.healthline.com/health/video/5-things-pnsclc
- https://www.lungcancercenter.com/lung-cancer/types/small-cell-lung-cancer/
Read full bio of Sneha Tete












