Lung Cancer and White Blood Cell Count: Frequently Asked Questions
Comprehensive insights on how lung cancer and its treatments affect white blood cell counts, risk factors, and clinical significance for patients.
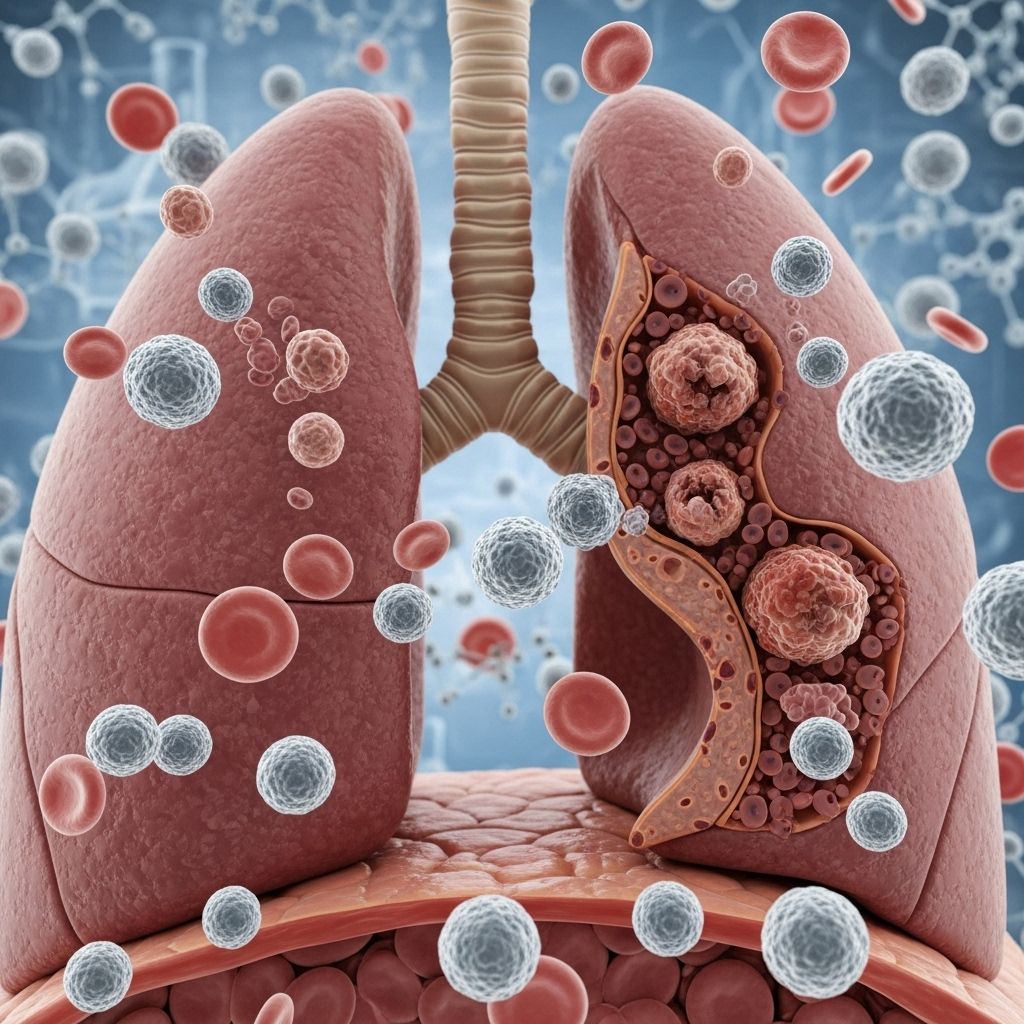
Lung cancer is a complex disease with wide-ranging impacts on the body, including on the immune system. One important indicator clinicians monitor is the white blood cell (WBC) count. Changes in this value can provide essential clues about the course of the disease, treatment side effects, and infection risks. This article compiles frequently asked questions about the relationship between lung cancer and white blood cell count, offering clear, evidence-based answers and practical guidance for patients and caregivers.
Understanding White Blood Cells
White blood cells, also called leukocytes, are a critical part of the immune system. They help protect the body from infections, fight off pathogens, and play a role in inflammation and the body’s response to injury and disease. WBCs are produced in the bone marrow and circulate in the blood and lymphatic system.
- Neutrophils: The most abundant type, essential for fighting bacterial infections.
- Lymphocytes: Key players in the adaptive immune response, targeting specific germs.
- Monocytes: Help clear away pathogens and dead cells.
- Eosinophils and Basophils: Involved in allergic responses and certain infections.
How Are White Blood Cell Counts Measured?
The WBC count is measured as part of a complete blood count (CBC) blood test. Normal values depend on age, health, and laboratory standards but generally fall between 4,000 and 11,000 cells per microliter of blood for healthy adults.
- High WBC count (Leukocytosis): May signal infection, inflammation, stress, or malignancy.
- Low WBC count (Leukopenia): Increases the risk of infection and can be caused by certain treatments or cancers.
- Absolute Neutrophil Count (ANC): Specifically tracks neutrophil levels, often monitored during cancer therapy.
Does Lung Cancer Affect White Blood Cell Counts?
Yes, lung cancer can influence WBC counts in multiple ways. Tumor-related factors, the body’s inflammatory response, and treatments like chemotherapy and radiation all play a part.
- Some lung tumors produce substances that stimulate the bone marrow to make more WBCs, especially neutrophils and monocytes.
- Increased WBC count at diagnosis or during the course of the disease may relate to the tumor itself or infection resulting from a suppressed immune system.
- Leukocytosis (elevated WBC count) is often linked with a poorer prognosis in patients newly diagnosed with lung cancer.
Alternatively, treatments such as chemotherapy commonly lower WBC counts, placing patients at higher risk for infections—particularly in the case of neutropenia (low neutrophil count).
What Causes Changes in White Blood Cell Counts with Lung Cancer?
There are several reasons why lung cancer patients may experience elevated or reduced WBC counts:
- Cancer-related inflammation: The immune system may increase WBC production in response to the tumor.
- Tumor secretion of growth factors: Certain lung cancers can secrete substances that stimulate WBC production unnaturally (paraneoplastic syndromes).
- Infection: Due to weakened immunity or obstruction in lungs, patients are at higher risk for infections, which can drive up WBC counts.
- Bone marrow involvement: Cancer that spreads to or affects the bone marrow can inhibit WBC production, causing leukopenia.
- Treatment side effects: Chemotherapy, radiation, and some targeted therapies suppress bone marrow activity—leading to lower WBC counts.
Is White Blood Cell Count a Risk Factor for Developing Lung Cancer?
Elevated pre-diagnosis WBC counts have been associated with an increased risk of developing lung cancer. Multiple large-scale studies have observed such associations, especially for higher neutrophil and monocyte counts.
- Higher baseline total WBC counts are linked to increased risk for lung adenocarcinoma, a major subtype of lung cancer.
- The link is particularly strong for monocytes and neutrophils, with monocyte count emerging as an important contributor to lung cancer risk.
However, it is important to note:
- Elevated WBC count is not, by itself, a cause of cancer. Rather, both high WBCs and cancer risk may share underlying chronic inflammation or immune dysregulation as a driver.
- Smoking status significantly modifies risk. Higher WBC counts predict greater lung cancer risk, especially in current or former smokers, but also in some never-smokers, notably women.
How Do Cancer Treatments Affect White Blood Cell Counts?
Most treatments for lung cancer—including chemotherapy, radiation, and some targeted therapies—can lower WBC counts by damaging the bone marrow, where these cells are produced. This effect can be temporary or long-lasting, depending on the therapy and individual response.
- Neutropenia: This is the most common and dangerous type of low WBC count during lung cancer treatment. It increases susceptibility to bacterial and fungal infections.
- Agranulocytosis: A severe reduction in granulocytes (mostly neutrophils) may occur with certain medications.
- Immunotherapy: Some immune checkpoint inhibitors may cause autoimmune effects on bone marrow, though less commonly result in neutropenia.
Monitoring and Managing Low WBC Counts
- Doctors frequently check blood counts during therapy to detect drops in WBCs early.
- If counts fall too low, treatment may be delayed or doses reduced.
- Medications called growth factors (e.g., G-CSF) may be used to stimulate WBC production.
- Poor WBC recovery or recurrent infections may require modifications to treatment or supportive care measures.
What Are the Risks of Low White Blood Cell Counts in Lung Cancer Patients?
Low WBC count, especially neutropenia, carries significant risks for people with lung cancer:
- Heightened infection risk: Even minor infections, such as a cold, can progress quickly and become severe.
- Hospitalization: Febrile neutropenia (fever with low neutrophils) is a medical emergency that often requires hospitalization and intravenous antibiotics.
- Treatment interruptions: Low counts may delay needed cancer therapies, potentially affecting outcomes.
Frequently Asked Questions (FAQs)
What is the normal range for white blood cell count?
The typical adult range is 4,000 to 11,000 cells per microliter of blood. Normal values may vary slightly by laboratory and age.
Can lung cancer cause high white blood cell counts before treatment?
Yes, some lung tumors secrete factors that stimulate bone marrow, resulting in higher WBC counts at diagnosis. Other causes can include infection or inflammation associated with the disease.
Why does chemotherapy lower my WBC count?
Chemotherapy, and sometimes radiation, target rapidly dividing cells, including cancer cells and healthy cells like those in the bone marrow. This suppresses new blood cell production, leading to temporary drops in WBC count.
How will I know if my WBC count is too low?
Routine blood tests will monitor counts. Symptoms such as fever, chills, mouth sores, or unexplained infections may indicate low WBCs and should be reported to your healthcare provider immediately.
Are there ways to boost my WBC count during treatment?
Medications known as white blood cell growth factors (like filgrastim or pegfilgrastim) can help your bone marrow produce more WBCs. Discuss this option with your oncologist, as not all patients require them.
Does my WBC count impact my cancer prognosis?
Abnormally high WBC count at diagnosis, especially due to leukemia-like effects of tumors, may be linked with poorer prognosis. Consistently low counts can interrupt treatment and increase infection risk, both of which may also affect overall outcome.
Is white blood cell count a reliable marker for diagnosing lung cancer?
No. While changes in WBC count can support clinical suspicion in the right context, they are not specific enough for diagnosis. Many conditions cause similar blood count changes. A diagnosis relies on imaging, tissue biopsy, and additional tests.
What can I do to lower my infection risk if my WBC count is low?
- Avoid crowds and people who are sick.
- Practice good hand hygiene by washing hands often.
- Stay current with recommended vaccines (as advised by your doctor).
- Monitor your temperature daily and report fevers promptly.
- Take care of your skin and mouth to prevent injury and infection.
Can physical activity or lifestyle changes influence my WBC count?
Regular physical activity and a healthy lifestyle may help regulate immune function and lower chronic inflammation, potentially influencing WBC levels. However, once under cancer treatment, any plans for vigorous activity should be discussed with your oncology team to ensure safety.
Key Takeaways for Patients and Caregivers
- Lung cancer and its treatments frequently affect white blood cell counts.
- Both elevated and reduced WBC counts have important implications for risk, infection, and management.
- Routine blood work is essential for monitoring during treatment.
- Alert your healthcare provider immediately about any signs of infection, fever, or new symptoms.
- With proper monitoring and prompt care, many WBC count changes can be safely managed.
When to Contact Your Doctor
Call your healthcare provider promptly if you:
- Develop a fever, chills, or sweats
- Notice unusual fatigue, bruising, or bleeding
- Experience new cough, shortness of breath, or chest pain
- Have signs of infection (e.g., redness, swelling, warmth, unusual pain)
Early intervention is key to preventing complications.
Resources for Support
- Oncology nurse navigators and cancer support staff
- Patient and caregiver support groups focused on lung cancer
- Educational resources from national cancer organizations
Managing the implications of WBC changes is a collaborative effort. Stay informed, communicate with your healthcare team, and ask questions whenever you’re uncertain about lab results or physical symptoms.
References
- https://www.nature.com/articles/s41598-025-88366-w
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7083262/
- https://acsjournals.onlinelibrary.wiley.com/doi/full/10.1002/1097-0142(20011101)92:9%3C2399::AID-CNCR1588%3E3.0.CO;2-W
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2692679/
- https://www.mylungcancerteam.com/resources/lung-cancer-and-neutropenia-what-to-know
- https://medlineplus.gov/ency/patientinstructions/000675.htm
- https://www.ukbiobank.ac.uk/publications/white-blood-cell-count-and-risk-of-incident-lung-cancer-in-the-uk-biobank/
Read full bio of medha deb












