Lung Cancer and Blood Clots: Understanding Risks, Symptoms, and Prevention
Learn the crucial link between lung cancer and blood clots—including causes, symptoms, treatments, and prevention strategies.
Lung Cancer and Blood Clots: Risks, Symptoms, and Prevention
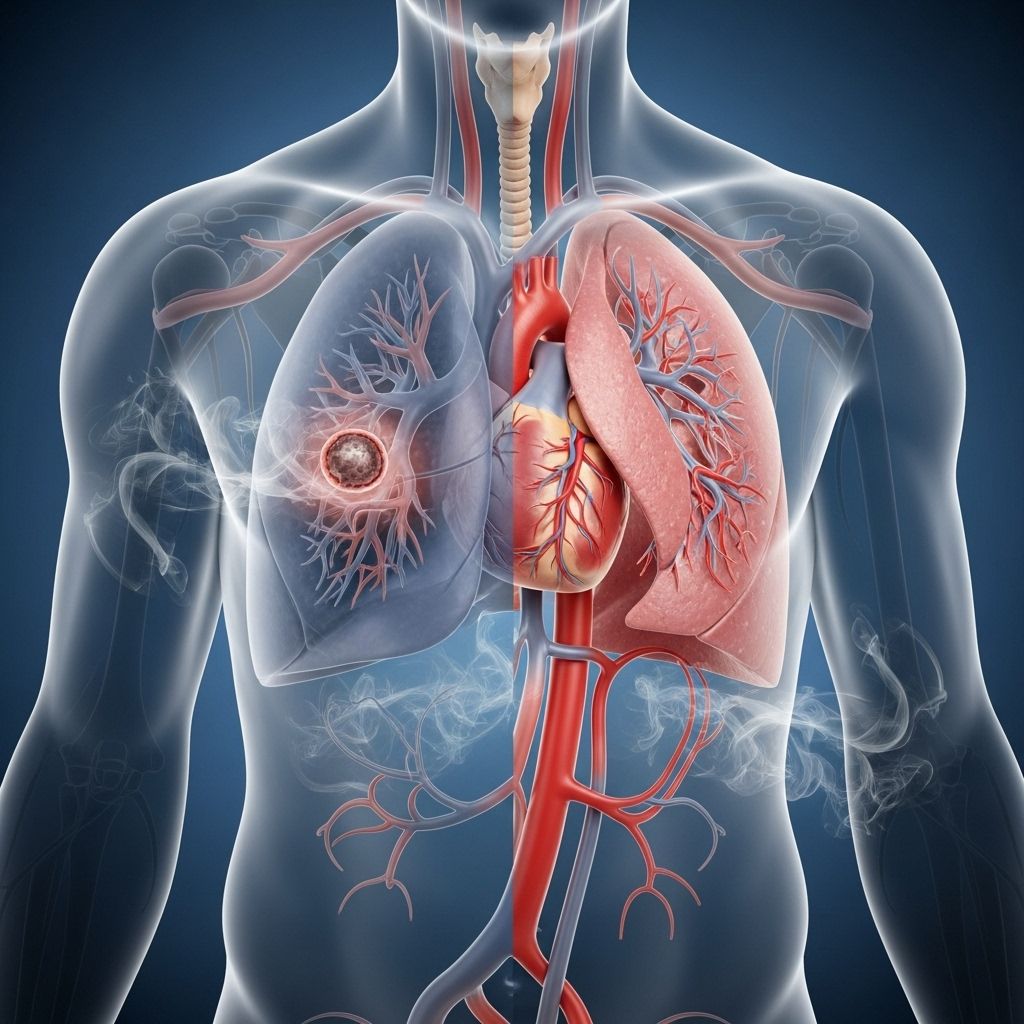
Lung cancer doesn’t just threaten the body through tumor growth—it also significantly increases the risk of dangerous blood clots. Understanding how and why blood clots form, recognizing symptoms, seeking treatment, and taking steps to prevent clots are essential for anyone affected by lung cancer, as blood clots are a leading cause of death in cancer patients.
How Lung Cancer Increases Blood Clot Risk
People with cancer, and especially those with lung cancer, have a higher risk of developing blood clots compared to the general population. Studies show that up to 20% of cancer patients will experience a blood clot during their illness, and for lung cancer patients, the risk can be four to seven times higher than in those without cancer.
Why Does Cancer Lead to More Blood Clots?
- Tumor Compression: Tumors can press against blood vessels, slowing blood flow and fostering clot formation.
- Blood Changes: Cancer cells can release chemicals that make the blood “stickier” and more likely to clot. These chemicals include proteins that promote clot formation, such as mucin.
- Damage from Treatments: Treatments like chemotherapy and radiation can damage blood vessel linings and disrupt normal anti-clotting signals in the blood.
- Immobility: Pain, surgery, or fatigue from cancer can lead to inactivity, a major risk factor for clot formation.
Blood clots may develop in veins (usually in the legs or arms), a condition known as deep vein thrombosis (DVT). These clots can travel to the lungs and cause a life-threatening pulmonary embolism (PE). Awareness and quick action are critical, as blood clots are the second leading cause of death in people with cancer, after the cancer itself.
Understanding Blood Clots: DVT and PE
A blood clot is a semi-solid mass of blood components that can form in the veins. When blood thickens too much, clots may form and restrict normal flow. The two main types of dangerous clots associated with cancer are:
- Deep Vein Thrombosis (DVT): A clot in a deep vein, usually in the leg or arm. If a DVT dislodges, it can travel through the bloodstream.
- Pulmonary Embolism (PE): A clot that has traveled to the lungs, blocking blood flow there.
Immediate medical attention is needed for both DVT and PE, as they can cause severe health problems or be fatal if left untreated.
Who’s Most at Risk?
Although all cancer patients face a higher risk, certain groups with lung cancer are especially vulnerable:
- Patients with advanced-stage (stage III or IV) lung cancer
- People with non-small cell lung cancer, particularly adenocarcinoma subtype
- Those undergoing surgery, chemotherapy, or radiation therapy
- Individuals with a history of blood clots or genetic clotting disorders
- People with other risk factors such as immobility, obesity, or infection
Cancer Treatments That Increase Clotting Risk
- Chemotherapy drugs, particularly platinum-based agents (like cisplatin)
- Hormonal therapies (such as tamoxifen)
- Drugs targeting blood vessels (VEGF inhibitors)
- Thalidomide and lenalidomide
- Surgery, especially major operations like tumor removal
- Central venous catheters (PICC lines)
Symptoms of Blood Clots in Lung Cancer
Symptoms can range from subtle to severe. It’s important to recognize early warning signs, as prompt treatment can be life-saving:
- Swelling, pain, or tenderness in one leg (especially the calf or thigh)
- Skin feels warm or looks reddish or bluish
- Pain in the arm, especially if a catheter is in place
Signs that a clot has moved to the lungs (pulmonary embolism) and become an emergency include:
- Sudden shortness of breath
- Chest pain, especially when breathing in
- Rapid heart rate
- Coughing up blood (hemoptysis)
- Severe weakness, fainting, or feeling light-headed
Why Do Blood Clots Happen in Lung Cancer?
Cancer alters the normal balance between substances that promote and prevent clotting. Key mechanisms include:
- Release of pro-coagulant chemicals: Cancer cells release substances that make the blood prone to clotting.
- Physical obstruction: Tumors compress or invade blood vessels, disturbing flow.
- Injury from treatments: Chemotherapy and radiation injure vessel linings, promoting clot formation.
- Immobility: Surgery, pain, or general weakness reduce movement, slowing blood flow and increasing risks.
Certain types of lung cancer, such as adenocarcinoma, and more advanced cancer stages tend to elevate clot risk even further. Blood “stickiness” or hypercoagulability is especially pronounced as the disease progresses.
Diagnosing Blood Clots
Diagnosing blood clots promptly is vital. Your doctor may recommend:
- Ultrasound to detect DVT in arms or legs
- CT or MRI scans to visualize blood vessels and check for clots in the lungs (PE)
- Blood tests (such as D-dimer) that can indicate clotting activity
- Physical examination and review of medical history and symptoms
Early detection and management dramatically improve outcomes. Always inform your healthcare provider about any new symptoms.
Treating Blood Clots in Lung Cancer
Blood clots associated with lung cancer are usually treated with anticoagulant medications that reduce the blood’s ability to clot. Treatment choices and duration depend on individual risk factors and whether the patient has other complicating issues such as low platelet counts.
Common Treatment Options
- Anticoagulants (“blood thinners”): Such as heparin, low-molecular-weight heparin (LMWH), and direct oral anticoagulants (DOACs). These prevent clots from growing and new ones from forming.
- Inferior vena cava (IVC) filter: A device sometimes placed in a vein to trap clots (when blood thinners aren’t an option).
- Adjusting cancer treatments if a specific drug is the likely trigger.
- Treating underlying infections, dehydration, or other medical conditions.
Close medical supervision is critical, as both cancer and anticoagulant medications can increase bleeding risk.
Preventing Blood Clots in Lung Cancer
Taking proactive steps to reduce blood clot risk is crucial for lung cancer patients. Prevention strategies include:
- Staying mobile: Move, stretch, or walk regularly—especially after surgery or hospital stays.
- Compression stockings to improve leg blood flow.
- Hydration: Drink plenty of fluids unless advised otherwise by your doctor.
- Follow doctor’s advice: Take prescribed medications and attend all follow-up appointments.
- Report symptoms immediately: Early detection of a clot can prevent serious complications.
Doctors will weigh the benefits and risks of preventive anticoagulants, especially in those with a high risk of clotting or a history of prior clots.
Special Risks with Catheters and Surgery
- Cancer patients often need central venous catheters for medications. These lines can raise clot risk, so regular checks are essential.
- Major surgery (e.g., tumor removal) increases clot risk. Preventive measures may include temporary blood thinners or mechanical devices to promote blood circulation.
Living with Lung Cancer and Blood Clots
Coping with both conditions brings extra challenges. Partnering with your healthcare team, being vigilant for symptoms, and adhering to treatment recommendations can help you avoid complications and improve your quality of life. If you experience:
- Sudden leg or arm swelling, warmth, or pain
- Unexpected chest pain or breathing difficulty
- Coughing up blood
Seek emergency help right away. These could be signs of DVT or a life-threatening PE. Your doctor may adjust your lung cancer treatment schedule to minimize clotting risks or treat underlying causes such as dehydration or infection.
Frequently Asked Questions (FAQs)
How common are blood clots in people with lung cancer?
Up to 20–25% of people with cancer will develop a blood clot at some point, with lung cancer patients at a four- to sevenfold increased risk compared to the general population.
What makes lung cancer patients more likely to get blood clots?
Cancer cells create pro-coagulant substances, tumors can block vessels and slow flow, and treatments such as chemotherapy or surgery damage vessel walls—all making blood clots more likely.
Are certain lung cancer treatments worse for clotting?
Yes. Some chemotherapies (especially platinum-based drugs), thalidomide, lenalidomide, VEGF inhibitors, and major surgery all pose significant clotting risks. Central lines or catheters also increase the chance of a clot forming in veins.
How are blood clots treated in someone with lung cancer?
The mainstay is anticoagulant medications (blood thinners), but your doctor may recommend additional measures—like an IVC filter or adjusting your cancer treatment, depending on individual risk factors and overall health.
Can blood clots be prevented if I have lung cancer?
While not all clots can be prevented, many steps—like staying active, using compression stockings, drinking fluids, and reporting symptoms promptly—can reduce your risk. Doctors may also prescribe preventive blood thinners if you’re at high risk.
Key Takeaways
- Lung cancer dramatically increases your risk for blood clots—especially deep vein thrombosis (DVT) and pulmonary embolism (PE).
- Symptoms to watch for include leg swelling, pain, sudden shortness of breath, or chest pain.
- The risk is greatest with advanced cancer, certain lung cancer types, and some treatments such as chemotherapy or surgery.
- Treatment usually involves anticoagulant drugs, with prevention strategies ranging from mobility to compression socks and medical interventions.
- Early recognition and prompt medical attention are essential for preventing life-threatening complications.
References
- American Cancer Society. Blood Clots and Cancer
- Lung Cancer Center. Blood Clots and Lung Cancer
- Cancer Research UK. Cancer and the Risk of Blood Clots
- Meyer Cancer Center. Lung Cancer: How to Protect Yourself from Blood Clots
References
- https://meyercancer.weill.cornell.edu/news/2017-08-09/lung-cancer-how-protect-yourself-blood-clots
- https://www.lungcancercenter.com/lung-cancer/symptoms/blood-clots/
- https://www.cancerresearchuk.org/about-cancer/coping/physically/cancer-and-the-risk-of-blood-clots
- https://www.cdc.gov/blood-clots/risk-factors/cancer.html
- https://www.healthline.com/health/pulmonary-embolus
- https://www.medicalnewstoday.com/articles/323701
- https://www.lungcancercenter.com/news/coughing-up-blood-hemoptysis/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6134828/
- https://www.mdanderson.org/patients-family/diagnosis-treatment/emotional-physical-effects/pulmonary-embolism-cancer.html
Read full bio of Sneha Tete












