Understanding the Link Between Lung Cancer and Blood Clots
People with lung cancer face significantly increased risk for blood clots, which can impact prognosis and treatment.
Lung Cancer and Blood Clots: A Detailed Overview
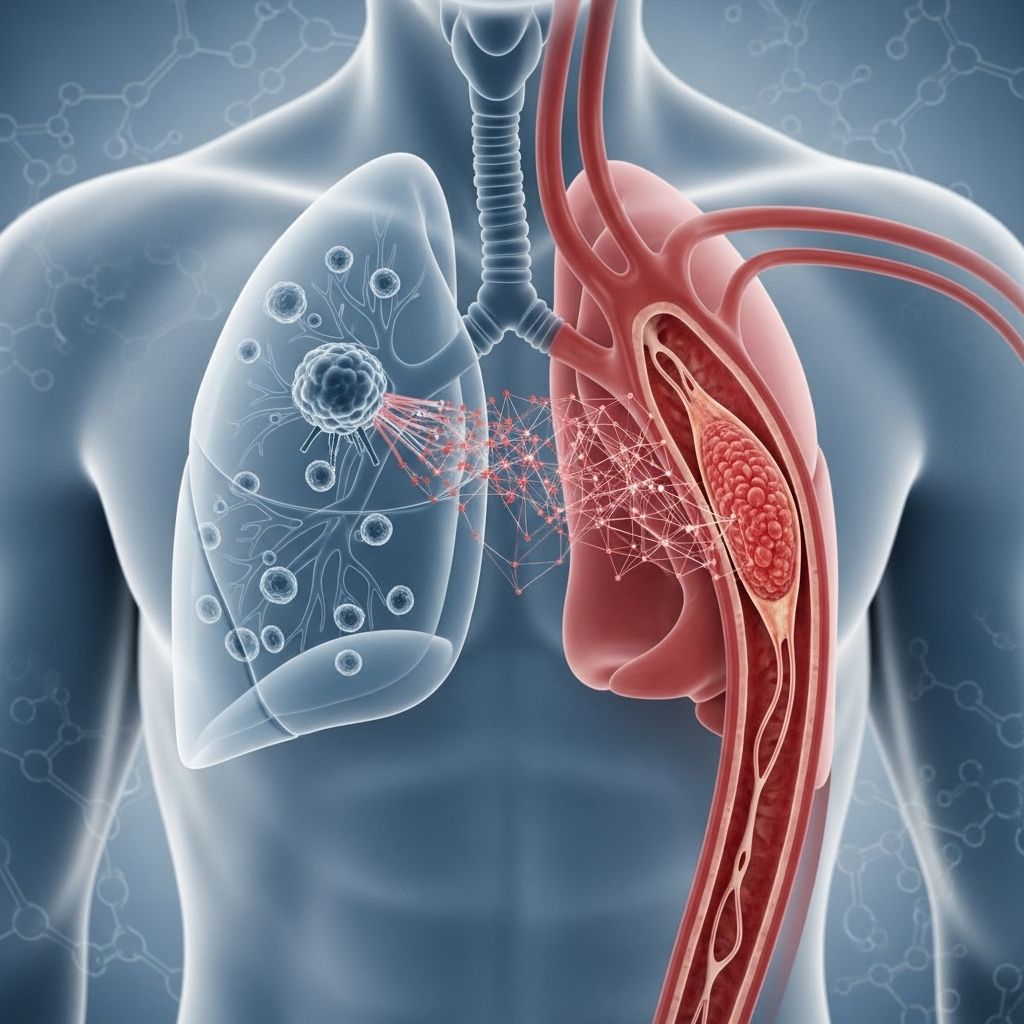
Lung cancer not only poses a direct threat to respiratory health but also greatly increases the likelihood of blood clots, specifically in veins and the lungs. The occurrence of blood clots is a serious and sometimes life-threatening complication for people living with lung cancer, impacting both short-term and long-term outcomes. Understanding the relationship between lung cancer and clot formation is crucial for effective prevention, early detection, and management.
What Are Blood Clots?
A blood clot is a mass formed from blood that has thickened or coagulated. Normally, clotting protects the body by stopping bleeding after injury, but abnormal clotting can occur inside blood vessels, leading to significant health problems—especially for cancer patients.
- Venous thromboembolism (VTE): A blood clot that occurs in a vein.
- Deep vein thrombosis (DVT): A clot in a deep vein, typically in the legs.
- Pulmonary embolism (PE): A clot travels to the lungs, blocking blood flow.
Both DVT and PE are serious and potentially fatal, demanding urgent medical attention.
How Does Lung Cancer Increase Blood Clot Risk?
Patients diagnosed with lung cancer are four to seven times more likely to develop blood clots than the general population. Research shows that as many as 13.8% of people with lung cancer will experience a venous thromboembolism during their disease course, and blood clots account for the second leading cause of death in these patients, after cancer itself.1,3
Multiple factors drive this increased risk:
- Tumor Pressure: Tumors can press against blood vessels, reducing blood flow and leading to clot formation.
- Changes in Blood Chemistry: Cancer cells release substances (like mucin and pro-coagulants) that make blood stickier and promote clotting.
- Therapeutic Side Effects: Cancer treatments—including certain chemotherapy drugs—can damage blood vessel linings and alter clotting factor balance.
- Physical Inactivity: Pain, fatigue, and other symptoms can result in limited movement, increasing the risk for blood clots.
Which Stages and Types of Lung Cancer Carry the Greatest Risk?
While any stage of lung cancer can elevate the risk of blood clots, the risk is especially heightened in the more advanced stages (III and IV). Research indicates that non-small-cell lung cancer, particularly adenocarcinoma, carries a higher risk than small-cell lung cancer.2,3
| Type / Stage | Clotting Risk |
|---|---|
| Advanced (Stage III & IV) | Highest risk; blood may be hypercoagulable |
| Adenocarcinoma (NSCLC) | Higher risk compared to other lung cancer types |
| Recent surgery or chemotherapy | Significantly increased risk |
Cancer Treatments That May Trigger Blood Clots
The following therapies can heighten the risk of abnormal clot formation in lung cancer patients:
- Chemotherapy agents, especially platinum drugs (like cisplatin)
- Lenalidomide and thalidomide
- L-asparaginase
- Tamoxifen
- Radiation therapy
- Surgery (especially major operations)
- VEGF inhibitors (e.g., bevacizumab)
- VEGF tyrosine kinase receptors inhibitors (e.g., sorafenib, sunitinib)
These interventions may damage blood vessel walls, exacerbate immobility, or directly stimulate coagulation, further raising the risk for VTE and PE.3
Who Is Most at Risk?
- Patients diagnosed with late-stage or metastatic lung cancer
- Individuals undergoing chemotherapy, radiation, or recent surgery
- People with limited physical activity due to cancer symptoms
- Patients with additional clotting risk factors (genetic predisposition, previous history of clots, obesity)
- Those exposed to carcinogenic substances like asbestos
Warning Signs and Symptoms of Blood Clots in Lung Cancer Patients
Recognizing the signs and symptoms early is key to prompt treatment and improved outcomes. Blood clots associated with lung cancer often present as:
- Deep pain, swelling, or redness, particularly in the legs (suggestive of DVT)
- Sudden onset shortness of breath or difficulty breathing
- Chest pain, especially while breathing
- Rapid heartbeat (palpitations)
- Coughing, sometimes with blood (hemoptysis)
- Fatigue or dizziness
Note: Pulmonary embolism, where a clot travels to the lungs, may result in acute symptoms such as severe shortness of breath and chest pain—medical emergency requiring immediate attention.
Complications Associated with Blood Clots in Lung Cancer
Beyond the immediate danger, blood clots lead to further complications:
- Pulmonary Embolism: Sudden blockage in the pulmonary artery can be fatal.
- Post-thrombotic syndrome: Chronic pain and swelling in the affected limb post-DVT.
- Impact on Cancer Treatment: Blood clots may delay or complicate ongoing cancer therapies.
Blood clots can also signify progression or complication of the underlying cancer, making ongoing monitoring essential.
Diagnosis: How Are Blood Clots Detected in Lung Cancer?
If symptoms suggest a blood clot, diagnostic techniques may include:
- Ultrasound imaging (especially for DVT)
- CT or MRI scans
- Blood tests (e.g., D-dimer)
- Venography or pulmonary angiography (for PE detection)
Early diagnosis is key to preventing serious complications.
Prevention Strategies for Blood Clots in Lung Cancer Patients
Managing the risk of clots involves proactive steps:
- Encourage gentle movement and physical activity when possible
- Use compression stockings to support blood flow
- Administer anticoagulant medications if prescribed
- Hydrate adequately to prevent thickening of the blood
- Monitor for symptoms, especially during periods of inactivity, after surgery, or while receiving chemotherapy
Healthcare teams may recommend preventive medicine or regular screening in high-risk patients.
Treatment of Blood Clots in Lung Cancer
Blood clots associated with lung cancer require tailored treatment strategies, considering overall health and concurrent therapies:
- Anticoagulants (blood thinners)—such as warfarin, heparin, or newer agents (NOACs)
- Thrombolytic therapy—medications to actively dissolve clots in emergencies
- Compression garments—to alleviate swelling and prevent further clot formation
- Surgical interventions—rarely, to remove clots
- Modifying cancer therapy—dose adjustments or palliative measures
Doctors carefully balance the risk of bleeding with the need to prevent further clotting, especially during combined cancer and clot treatment.
Coping Strategies and Support for Patients
- Regular communication with your cancer care team
- Joining support groups for emotional and practical help
- Seeking guidance from oncology nurse navigators
- Utilizing mental health services, as anxiety is common after clot diagnosis
Many cancer centers offer resources for navigating these complex challenges.
Frequently Asked Questions (FAQs)
Q: Why does lung cancer increase the risk of blood clots?
A: Lung cancer affects blood flow and increases substances that promote clotting. Tumors may physically compress vessels, cancer cells can secrete pro-coagulants, and treatment modalities often damage blood vessel linings—making clots more likely.
Q: What are the most serious complications of blood clots for lung cancer patients?
A: The most severe risk is a pulmonary embolism—a potentially fatal clot in the lungs. Other concerns include chronic swelling (post-thrombotic syndrome), delays in therapy, and increased mortality.
Q: Are blood clots more common with certain cancer treatments?
A: Yes. Treatments such as chemotherapy, especially platinum-based agents, radiation therapy, surgery, and drugs targeting VEGF or hormone receptors are strongly linked to increased clot risk.
Q: How can I reduce my risk of blood clots if I have lung cancer?
A: Important steps include staying active as possible, wearing compression stockings, staying hydrated, following prescribed medicine regimens, and alerting your healthcare team at the first sign of symptoms.
Q: What should I do if I think I have a blood clot?
A: Seek emergency medical attention. Symptoms such as sudden leg swelling, severe pain, chest pain, or trouble breathing need urgent evaluation.
Summary Table: Blood Clots in Lung Cancer
| Feature | Description |
|---|---|
| Prevalence | 4–7x higher risk than non-cancer patients |
| Main Types | DVT (legs), PE (lungs) |
| High-Risk Groups | Advanced stage, recent surgery/chemotherapy, immobility |
| Symptoms | Pain, leg swelling, chest pain, rapid heartbeat, coughing blood |
| Prevention | Movement, hydration, compression, medication |
| Treatment | Anticoagulants, thrombolytics, supportive care |
Takeaway: What Patients and Families Need to Know
Blood clots are a frequent and serious complication in lung cancer patients. Awareness of risk factors, early detection of symptoms, and close partnership with healthcare providers are vital for avoiding life-threatening outcomes. Cancer patients should be proactive with their care—noticing new or worsening symptoms, asking about preventive measures, and reporting any concerns immediately.
With timely intervention, coordinated care, and support, patients and their families can better manage the risk of blood clots and maintain quality of life throughout their cancer journey.
References
- https://www.mylungcancerteam.com/resources/what-to-know-about-lung-cancer-and-blood-clots
- https://meyercancer.weill.cornell.edu/news/2017-08-09/lung-cancer-how-protect-yourself-blood-clots
- https://www.lungcancercenter.com/lung-cancer/symptoms/blood-clots/
- https://www.medicalnewstoday.com/articles/lung-cancer-blood-clots
- https://www.healthline.com/health/cancer-and-pulmonary-embolism
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10814098/
- https://www.fredhutch.org/en/news/center-news/2019/03/blood-clots-thrombosis-what-cancer-patients-need-to-know.html
- https://www.cancerresearchuk.org/about-cancer/coping/physically/cancer-and-the-risk-of-blood-clots
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6134828/
Read full bio of medha deb












