Lung Adenocarcinoma: Symptoms, Diagnosis, Treatment, and Outlook
A comprehensive guide to lung adenocarcinoma symptoms, risk factors, diagnosis, treatment options, and prognosis.
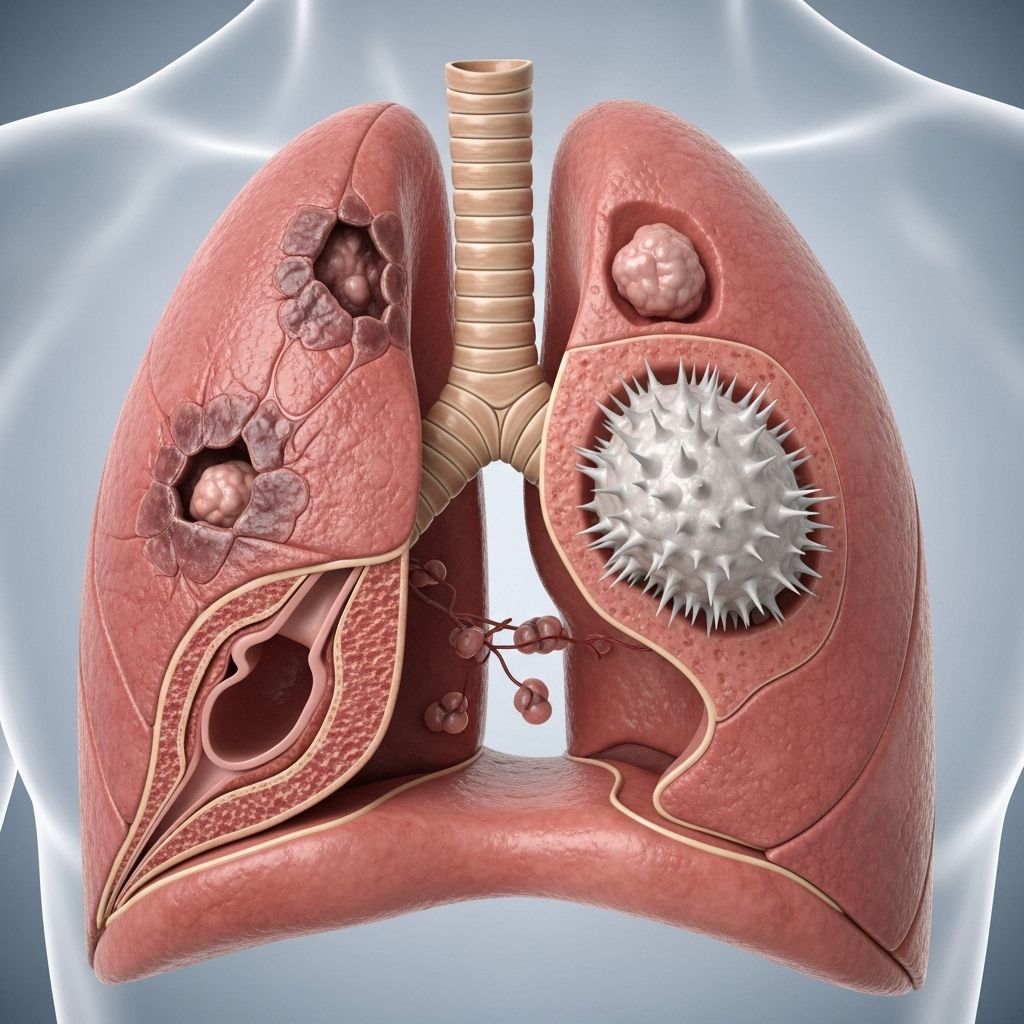
Lung Adenocarcinoma: An Overview
Lung adenocarcinoma is the most common type of non-small cell lung cancer (NSCLC), accounting for up to 40% of lung cancer cases. It typically originates in the outer regions of the lungs and affects both smokers and non-smokers, making it a critical topic in pulmonary health. This form of cancer is especially prevalent in women and younger individuals compared to other lung cancer types.
What Is Lung Adenocarcinoma?
Lung adenocarcinoma develops from glandular (mucus-producing) cells in the lung tissue. Unlike squamous cell carcinoma, which generally starts in the central bronchial passages, adenocarcinoma is often found in the lung periphery. It belongs to the group of non-small cell lung cancers, which tend to grow and spread more slowly than small cell lung cancer. However, diagnosis often occurs after the disease has advanced beyond the lungs.
Symptoms of Lung Adenocarcinoma
Early-stage lung adenocarcinoma is often asymptomatic, but as the disease progresses, a range of signs may develop. Symptoms can be subtle and may mimic other respiratory illnesses, making early detection a challenge.
- Persistent cough that does not go away
- Coughing up blood or blood-streaked mucus
- Shortness of breath or difficulty breathing
- Chest pain, especially worsened by deep breathing, coughing, or laughing
- Loss of appetite
- Unexplained weight loss
- Fatigue or feeling weak
- Recurring respiratory infections such as bronchitis or pneumonia
- Hoarseness or voice changes
- Pain while swallowing
- Fever without a clear cause
- New onset of wheezing
As the cancer spreads (metastasizes), additional symptoms might appear, such as:
- Bone pain (especially in the back or hips)
- Headaches, dizziness, seizures, or neurological symptoms (if spread to the brain)
- Swelling of lymph nodes (especially in the neck or above the collarbone)
- Jaundice (yellowing of skin and eyes, if spread to the liver)
Less Common and Advanced Symptoms
- Clubbing of fingers or toes (abnormal enlargement of the fingertips)
- Superior vena cava syndrome (swelling of the face, neck, and upper chest, caused by pressure from a tumor)
- Dysphagia (difficulty swallowing)
- Paraneoplastic syndromes, which may include hormone-related complications such as Cushing syndrome, SIADH, or hypercalcemia
Causes and Risk Factors
Understanding the risks associated with lung adenocarcinoma can support early detection and prevention efforts. While smoking remains the leading cause, other factors play significant roles:
- Tobacco smoking: Most patients have a history of smoking, although adenocarcinoma is also common in never-smokers.
- Exposure to radon gas: A radioactive gas that can accumulate in buildings, increasing lung cancer risk.
- Asbestos exposure: Especially in workplace environments.
- Air pollution: Chronic exposure to particulate matter and other pollutants.
- Genetic predisposition: Inherited genetic mutations, such as EGFR or changes on chromosome 6, may increase risk particularly in younger patients, women, and East Asians.
- Secondhand smoke: Increased risk for non-smokers exposed to tobacco smoke.
- Family history of lung cancer.
- History of lung diseases such as chronic obstructive pulmonary disease (COPD).
- Previous radiation therapy to the chest region.
How Is Lung Adenocarcinoma Diagnosed?
Early detection relies on a combination of clinical evaluation, imaging, and tissue sampling. Because its symptoms often overlap with those of other respiratory diseases, specific diagnostic tests are necessary to confirm lung adenocarcinoma.
- Medical history and physical exam: Focus on smoking status, environmental exposures, family medical history, and symptoms.
- Imaging studies:
- Chest X-ray: May identify a suspicious nodule or mass.
- CT scan (computed tomography): Offers detailed views of the lungs and chest, helpful for detecting smaller lesions.
- MRI or PET scan: Used to stage the cancer and check for metastases.
- Sputum cytology: Examining mucus coughed up from the lungs for cancerous cells.
- Biopsy: Essential for a definitive diagnosis, usually performed via techniques such as bronchoscopy, needle biopsy (guided by CT), or surgical biopsy.
Pathology then classifies the adenocarcinoma based on microscopic examination, which helps guide treatment. Subtypes include acinar, papillary, bronchoalveolar, and mucinous adenocarcinoma.
Staging
Lung adenocarcinoma is staged according to the TNM system, which evaluates the size of the tumor (T), lymph node involvement (N), and presence of metastasis (M). Staging determines treatment options and prognosis.
| Stage | Description |
|---|---|
| Stage I | Tumor localized in the lung, no lymph node involvement or metastasis. |
| Stage II – III | Tumor has spread to nearby tissues or lymph nodes but not distant organs. |
| Stage IV | Cancer has metastasized to distant parts of the body. |
Types of Lung Adenocarcinoma
- Acinar – Gland-like structures, mucus producing.
- Papillary – Tumor cells form finger-like projections.
- Bronchioloalveolar (now called lepidic) – Grows along the alveolar structures, often slow-growing.
- Solid – Tumor consists of solid sheets of cells with little mucus.
- Mucinous – Tumor cells produce significant mucus.
Treatment Options for Lung Adenocarcinoma
The optimal treatment plan depends on the stage at diagnosis, the tumor’s genetic features, and the patient’s overall health. Multimodal therapy, combining surgery, chemotherapy, targeted therapy, and immunotherapy, is often considered.
Surgical Treatments
- Lobectomy (removal of a lung lobe): The preferred treatment for early-stage cases.
- Pneumonectomy (removal of an entire lung): Utilized if the tumor is extensive.
- Segmentectomy or wedge resection: Less extensive surgeries to remove small tumors.
Non-surgical Treatments
- Radiation therapy: For those ineligible for surgery or as an adjunct post-surgery.
- Chemotherapy: Often used in advanced disease or alongside other therapies.
- Targeted therapy: Drugs that interfere with specific genetic mutations (e.g., EGFR, ALK, ROS1, BRAF) common in adenocarcinoma. These are especially effective in patients whose tumors harbor those mutations.
- Immunotherapy: Boosts the body’s immune system to attack cancer cells. It’s primarily used in metastatic or advanced disease.
Supportive and Palliative Care
- Pain management, oxygen therapy, pulmonary rehabilitation, and psychosocial support are important for improving quality of life in advanced cases.
- Palliative care: Focuses on relieving symptoms and increasing comfort, especially in late stages.
Prognosis and Survival Rates
The prognosis for lung adenocarcinoma varies widely and is largely determined by the stage at diagnosis:
- Early-stage (Stage I): 5-year survival rates can be as high as 60-80% when tumors are surgically resectable.
- Locally advanced (Stage II-III): Lower survival rates, generally 30-40% for Stage II and 10-20% for Stage III.
- Metastatic (Stage IV): 5-year survival is less than 10%.
Prognosis also depends on overall health, response to treatment, and the presence of actionable genetic mutations suitable for targeted therapy. Continued developments in targeted and immunotherapies are improving outcomes for some patients.
Prevention and Risk Reduction
- Don’t smoke: The single most important prevention strategy.
- Avoid secondhand smoke and environmental exposures (radon, asbestos).
- Test your home for radon and mitigate if needed.
- Live a healthy lifestyle: Eat a balanced diet, exercise regularly, and avoid exposure to harmful chemicals.
- Seek screening: Annual low-dose CT scans for high-risk groups can help with early detection.
Frequently Asked Questions (FAQs)
Q: What differentiates lung adenocarcinoma from other lung cancers?
A: Lung adenocarcinoma originates from glandular cells and is usually peripheral in the lung, while squamous cell carcinoma and small cell lung cancer have different origins, locations, and behaviors.
Q: How is lung adenocarcinoma detected early?
A: Early stages rarely cause noticeable symptoms, so high-risk individuals (such as long-term smokers) may benefit from routine low-dose lung CT scans as part of a lung cancer screening program.
Q: Can non-smokers develop lung adenocarcinoma?
A: Yes. While smoking is a leading risk factor, a significant proportion of lung adenocarcinomas occur in non-smokers due to genetic and environmental factors.
Q: Are there targeted treatments for lung adenocarcinoma?
A: Yes. If tumor cells feature mutations such as EGFR or ALK, targeted drugs may offer improved outcomes, especially in advanced disease.
Q: What lifestyle changes can reduce the risk?
A: Avoid smoking, limit exposure to carcinogens, improve home ventilation, maintain a healthy diet, and seek regular medical care for any persistent respiratory symptoms.
Key Takeaways
- Lung adenocarcinoma is the most common lung cancer in both smokers and non-smokers, often diagnosed at a later stage.
- Symptoms are frequently nonspecific or absent early, so high-risk individuals should consider regular screening.
- Diagnosis combines medical history, imaging, and biopsy.
- Treatment depends on stage, genetic profile, and patient health; modern advances in targeted and immunotherapies are making survival gains.
- Prognosis is best with early-stage detection; prevention remains the most effective strategy.
References
- https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/signs-symptoms.html
- https://en.wikipedia.org/wiki/Adenocarcinoma_of_the_lung
- https://www.mercy.com/health-care-services/cancer-care-oncology/specialties/lung-cancer-treatment/conditions/lung-adenocarcinoma
- https://lcfamerica.org/about-lung-cancer/diagnosis/types/adenocarcinoma/
- https://www.ncbi.nlm.nih.gov/books/NBK519578/
- https://www.cancercenter.com/cancer-types/lung-cancer/types/adenocarcinoma-of-the-lung
- https://www.mayoclinic.org/diseases-conditions/lung-cancer/symptoms-causes/syc-20374620
- https://my.clevelandclinic.org/health/diseases/4375-lung-cancer
- https://www.moffitt.org/cancers/lung-cancer/faqs/what-are-the-causes-of-adenocarcinoma-lung-cancer/
- https://www.lungevity.org/lung-cancer-basics/types-of-lung-cancer/lung-adenocarcinoma
Read full bio of Sneha Tete












