Lung Adenocarcinoma: Symptoms, Diagnosis, Stages, and Treatment
Understanding lung adenocarcinoma: symptoms, progression, diagnosis, and modern treatment approaches.
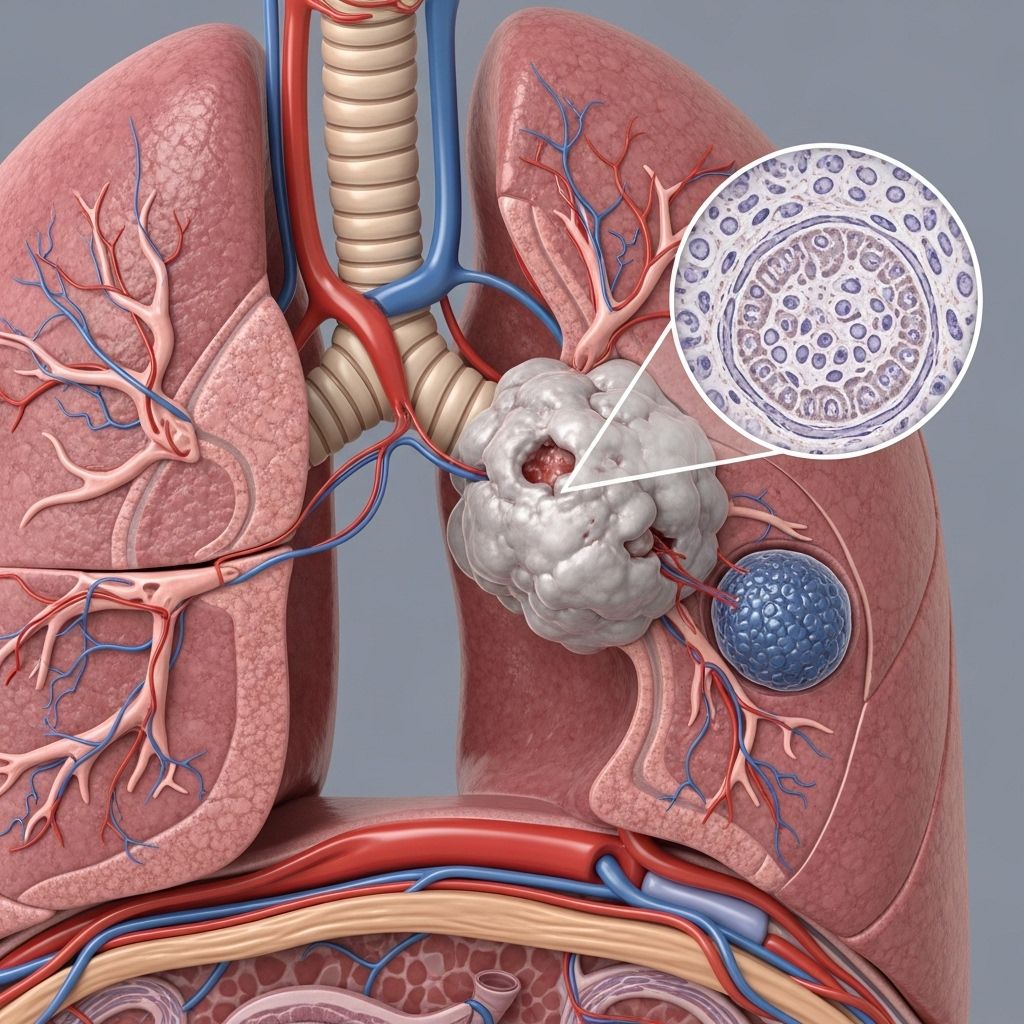
Lung Adenocarcinoma Overview
Lung adenocarcinoma is the most common type of non-small cell lung cancer (NSCLC), originating in the glandular cells lining the lungs. This type of cancer forms in cells along the outer regions of the lungs and is often associated with a history of smoking, though it also occurs in non-smokers. Adenocarcinoma tends to grow more slowly than other lung cancer variants, but its ability to spread—sometimes early in the disease course—makes early detection crucial for effective treatment.
What Are the Symptoms of Lung Adenocarcinoma?
Symptoms of lung adenocarcinoma typically appear in later stages, as early disease may be asymptomatic. Recognizing warning signs is vital for timely diagnosis:
- Persistent cough that does not resolve
- Coughing up blood (hemoptysis)
- Shortness of breath
- Chest pain, especially when coughing, laughing, or taking deep breaths
- Fatigue
- Hoarseness
- Wheezing
- Production of brownish or reddish phlegm
- Unintentional weight loss
- Reduced appetite
Some individuals may also develop symptoms related to local spread (such as superior vena cava obstruction) or rare paraneoplastic syndromes (like SIADH or Cushing syndrome).
Unique and Advanced Signs
- Phrenic nerve palsy (causing breathing difficulty)
- Horner syndrome (ptosis, miosis, anhidrosis)
- Compression of brachial plexus (limb weakness)
- Pericardial or pleural effusion (fluid around the heart or lungs)
Causes and Risk Factors
Cancer develops due to genetic changes within lung cells, many of which are associated with exposure risk factors:
- Smoking tobacco (primary and secondhand smoke)
- Environmental exposures (such as radon, asbestos, air pollution)
- Family history of lung cancer
- Previous history of lung disease (COPD, pulmonary fibrosis)
- Advanced age
Although smoking is the leading risk factor, a significant proportion of lung adenocarcinoma cases occur in non-smokers, especially women and younger individuals.
Growth and Stages of Lung Adenocarcinoma
Understanding cancer staging is vital for effective management. Adenocarcinoma typically progresses through five recognized stages:
| Stage | Description |
|---|---|
| Stage 0 | Cancer is confined to the inner lining (in situ) and has not invaded deeper tissues. |
| Stage 1 | Cancer is localized within the lung and has not spread to lymph nodes. |
| Stage 2 | Cancer has spread to nearby lymph nodes within or close to the lung. |
| Stage 3 | Spread to further lymph nodes or nearby structures within the chest. |
| Stage 4 | Spread (metastasis) to distant organs or tissues (such as bones, liver, or brain). |
Histopathology: Subtypes of Adenocarcinoma
Histological analysis categorizes lung adenocarcinoma based on the growth pattern and cell origin. Subtypes include:
- Acinar
- Papillary
- Bronchoalveolar
- Mucinous (mucus-secreting)
The subtype can influence prognosis and guide treatment approach.
How Serious Is Adenocarcinoma of the Lung?
The seriousness depends on several factors:
- Stage at diagnosis: Advanced stages (3 and 4) typically have a poorer outlook.
- Genetic alterations present in tumor cells (specific mutations may guide targeted therapy)
- Patient’s age and overall health
- The specific adenocarcinoma subtype
- The functional status of the lungs
Early detection and intervention can considerably improve survival rates and long-term outcomes.
How Is Lung Adenocarcinoma Diagnosed?
Diagnosis involves several steps using both clinical assessment and laboratory testing:
- Medical history and risk factor assessment (smoking, family history, previous illnesses)
- Physical examination: Checking lungs, vital signs, and overall health
Diagnostic Tests
- Blood tests (CBC, blood chemistry): To assess general health and rule out other causes
- Imaging tests:
- Chest X-ray: Initial screening for lung abnormalities
- Computed tomography (CT) scan: Detailed cross-sectional images
- Positron emission tomography (PET) scan: Detects active cancer cells
- Bronchoscopy: Thin, flexible tube with camera visualizes airways and allows tissue sampling
- Sputum cytology: Microscopic analysis of mucus (less helpful for peripheral adenocarcinoma)
- Thoracentesis: Sampling fluid around the lung if present (pleural effusion)
- Lung biopsy: Gold standard—tissue sample reviewed under microscope to confirm cancer presence
Tumor tissue may also be tested for specific proteins or genetic changes. These biomarkers help determine treatment strategy, especially for targeted therapy and immunotherapy.
Treatment Options for Lung Adenocarcinoma
Lung adenocarcinoma treatment depends on cancer stage, personal health status, and mutation status. Treatment modalities may be used alone or in combination:
Surgery
- Preferred for early-stage disease.
- Procedures include lobectomy (removal of a lung lobe), segmentectomy, or pneumonectomy (removal of entire lung).
- Lymph node removal for staging and prevention of further spread.
- Post-surgical recovery varies (hospital stay of 5–7 days, with full recovery taking weeks to months).
Chemotherapy
- Uses drugs to kill cancer cells systemically.
- May be used before surgery to shrink the tumor, after surgery to reduce recurrence risk, or for advanced disease.
Radiation Therapy
- High-energy beams target cancer cells.
- Often combined with chemotherapy for locally advanced cancers or used palliatively to relieve symptoms.
Targeted Therapy
- Targets specific genetic or protein changes (mutations) in cancer cells.
- Drugs may be prescribed for tumors with mutations such as EGFR, ALK, or ROS1.
Immunotherapy
- Stimulates the body’s immune system to attack cancer cells.
- Used for advanced stages; certain biomarkers (such as PD-L1) increase chances of response.
Palliative Care
- Focuses on symptom relief and quality of life for patients with advanced disease.
- May include pain management, nutritional support, and psychological care.
Prognosis and Outlook
The outlook for lung adenocarcinoma varies by stage at diagnosis, tumor biology, and patient health:
- Early-stage diagnosis allows for potentially curative treatment (such as surgery).
- Advanced stages generally require combination therapies and have lower survival rates.
- Modern advancements in targeted therapy and immunotherapy have improved outcomes for select groups.
- Regular follow-up is essential for monitoring recurrence and managing complications.
Prevention and Risk Reduction Strategies
- Avoiding tobacco smoke
- Minimizing exposure to environmental carcinogens (radon, asbestos, air pollution)
- Maintaining healthy lifestyle and regular medical checkups for high-risk individuals
- Genetic counseling for those with a strong family history of lung cancer
Frequently Asked Questions (FAQs)
Q1: Who is most at risk for lung adenocarcinoma?
Individuals with a history of smoking, significant exposure to carcinogens, or a family history of lung cancer are at highest risk. However, non-smokers—especially women—can also develop adenocarcinoma.
Q2: Can lung adenocarcinoma be cured?
Early-stage adenocarcinoma may be curable through surgery and adjuvant therapies. Advanced disease is less likely to be cured but may be managed effectively to prolong life and reduce symptoms.
Q3: Are symptoms unique in the early stages?
Most early-stage cases are asymptomatic, frequently discovered during routine imaging for other conditions. When present, the symptoms are often mild and nonspecific (persistent cough, mild chest pain).
Q4: What is the difference between adenocarcinoma and other lung cancer types?
Adenocarcinoma arises from glandular cells, is generally found in the lung periphery, and tends to grow slower than squamous cell carcinoma, which originates in the bronchi closer to the center of the lung.
Q5: How are genetic tests used in treatment planning?
Genetic and molecular tests on tumor tissue identify mutations that can be targeted with specific drugs, improving outcomes in select patients. Common targets include EGFR, ALK, and ROS1.
Key Takeaways
- Lung adenocarcinoma is the most common form of non-small cell lung cancer.
- Symptoms often appear late; early detection requires vigilance and screening, particularly for high-risk individuals.
- Treatment is personalized based on stage, genetic makeup of the tumor, and overall health.
- Advances in genetic testing and targeted therapies have improved the prognosis for some patients.
- Prevention centers on reducing tobacco exposure and managing environmental risks.
References
- https://www.healthline.com/health/lung-cancer/non-small-cell-adenocarcinoma
- https://www.ncbi.nlm.nih.gov/books/NBK519578/
- https://www.cancercenter.com/cancer-types/lung-cancer/types/adenocarcinoma-of-the-lung
- https://my.clevelandclinic.org/health/diseases/21652-adenocarcinoma-cancers
- https://my.clevelandclinic.org/health/diseases/4375-lung-cancer
- https://www.mayoclinic.org/diseases-conditions/lung-cancer/diagnosis-treatment/drc-20374627
- https://www.lungevity.org/lung-cancer-basics/types-of-lung-cancer/lung-adenocarcinoma
- https://www.aafp.org/pubs/afp/issues/2022/0500/p487.html
- https://www.mayoclinic.org/diseases-conditions/lung-cancer/symptoms-causes/syc-20374620
- https://www.mdanderson.org/cancer-types/lung-cancer.html
Read full bio of medha deb












