Lumbar Puncture: Procedure, Risks, and Patient Care
A thorough guide on lumbar puncture: why it’s done, how it works, who needs it, preparation, recovery, and answers to frequently asked questions.
Lumbar Puncture: Purpose, Preparation, Risks, and Results
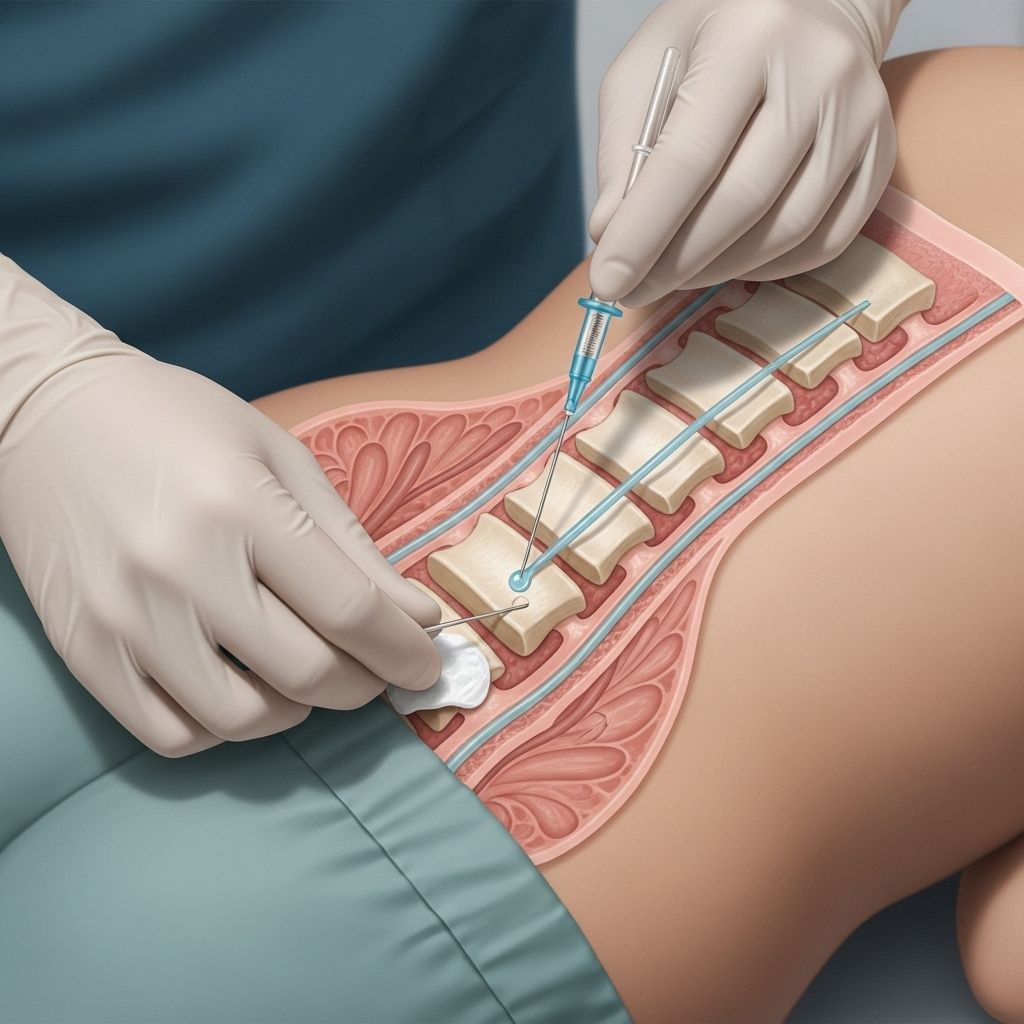
A lumbar puncture—also called a spinal tap—is a medical procedure in which a thin needle is used to access the spinal canal in the lower back to collect cerebrospinal fluid (CSF) for testing, deliver certain medications, or relieve pressure. Understanding why this procedure is done, how to prepare, the steps involved, potential risks, and what to expect after, can help patients approach the lumbar puncture with confidence and clarity.
What Is a Lumbar Puncture?
A lumbar puncture is a procedure performed to obtain cerebrospinal fluid, the clear fluid that cushions the brain and spinal cord inside the skull and spine. The test is critical for diagnosing several conditions and can also be used for therapeutic interventions.
- Alternative names: Spinal tap
- Main purpose: Gather information about central nervous system health or deliver drugs to the spinal canal
- Common location: Lower back, usually between lumbar vertebrae L3-L4 or L4-L5
Why Is a Lumbar Puncture Performed?
Doctors order lumbar punctures for several reasons, broadly split into diagnostic and therapeutic purposes:
- Diagnose infections: Such as meningitis (bacterial, viral, or fungal infections of the tissues surrounding the brain and spinal cord)
- Detect bleeding: Especially subarachnoid hemorrhage, or bleeding around the brain
- Diagnose inflammatory conditions: Such as multiple sclerosis or Guillain-Barré syndrome
- Detect cancers: By finding cancerous cells in CSF, aiding the diagnosis or staging of conditions like leukemia or lymphoma
- Measure CSF pressure: Abnormal pressure can indicate medical emergencies or chronic conditions affecting the brain and spinal cord
Less commonly, a lumbar puncture allows for the administration of chemotherapy, spinal anesthetics, or other medications directly into the CSF (an intrathecal injection). It can also help reduce high CSF pressure in some conditions.
Conditions Diagnosed or Treated with Lumbar Puncture
- Meningitis (bacterial, viral, or fungal)
- Encephalitis
- Subarachnoid hemorrhage
- Multiple sclerosis
- Guillain-Barré syndrome
- Cancers affecting the central nervous system
- Pseudotumor cerebri (idiopathic intracranial hypertension)
Who Needs a Lumbar Puncture?
A lumbar puncture is generally ordered when a doctor suspects a condition that involves the central nervous system and needs direct evidence from the CSF, or when there is a need to deliver medication to this space. Your healthcare provider will weigh the benefits against the risks and determine if it suits your particular situation.
How to Prepare for a Lumbar Puncture
Preparation helps ensure the procedure’s accuracy and reduce side effects. Here are important steps and considerations:
- Discuss medications: Inform your doctor about all current medications, especially blood thinners or anticoagulants.
- Allergies: Disclose any allergies to anesthetics, iodine, or antiseptics.
- Recent illnesses: Notify your physician of any fevers or infections.
- Imaging: Sometimes, a CT or MRI scan is performed beforehand to check for conditions that might make the puncture dangerous, such as raised intracranial pressure or brain mass.
- Fasting: Fasting may not be needed, but follow your doctor’s advice about eating or drinking before the test.
Most lumbar punctures are outpatient procedures, though some may take place in the hospital depending on the patient’s condition or reason for the procedure.
What Happens During a Lumbar Puncture?
The general sequence of events during a lumbar puncture includes:
- Consent: You will be asked to provide informed consent, confirming you understand the risks and benefits.
- Positioning: Typically, patients are asked to lie on their side with knees drawn up to their chest and chin to chest, assuming a fetal position. Alternatively, the procedure can be done while seated and leaning forward.
- Cleansing the site: The lower back is cleansed with an antiseptic solution, and a sterile drape is placed.
- Local anesthesia: The skin and deeper tissues at the site are numbed with a local anesthetic.
- Needle insertion: Once the area is numb, the doctor inserts a special thin needle between two lumbar vertebrae, advancing gently until it reaches the subarachnoid space around the spinal cord.
- Collection of CSF: CSF flows into sterile tubes for lab analysis. Typically, about 10 to 15 milliliters are collected.
- Measuring pressure: The opening pressure of the CSF may be checked with a manometer.
- Removing the needle and dressing the site: The needle is withdrawn and a bandage is applied.
- Observation: You’ll usually need to lie flat for up to an hour to minimize the risk of headache, under medical supervision.
What layers does the needle pass through?
- Skin
- Subcutaneous fat
- Supraspinous ligament
- Interspinous ligament
- Ligamentum flavum
- Epidural space
- Dura mater
- Subdural space
- Arachnoid mater
- Subarachnoid space (target for CSF collection)
What Are the Risks of a Lumbar Puncture?
Like all medical procedures, lumbar puncture has potential risks and complications, though serious problems are uncommon when performed by skilled professionals on appropriately selected patients.
- Headache: The most common side effect, called a post-dural puncture headache. It usually resolves in a few days but may last longer. Lying flat and staying hydrated may help.
- Back discomfort: Mild pain or tenderness at the insertion site may occur for a few days.
- Bleeding: Rarely, bleeding in or around the spinal canal happens, especially in people with bleeding disorders or those on anticoagulants.
- Infection: An infection at the puncture site or deeper inside the spine is rare due to sterile technique.
- Nerve irritation: Tingling or radiating pain may occur if the needle contacts nerve roots, but this is usually brief.
- Herniation risk: Very rarely, lumbar puncture can cause brain tissue to shift if there is increased intracranial pressure, which is why imaging may be done first in certain cases.
Most complications are mild and temporary, but your doctor will discuss all known risks and steps taken to minimize them.
How to Recover After a Lumbar Puncture
Post-procedure care is crucial for symptom relief and avoidance of complications. Here’s what to expect:
- Lying flat: Remain lying down for at least an hour after the procedure unless your doctor advises differently.
- Activity: Take it easy for the next 24 hours; avoid strenuous activity or heavy lifting.
- Fluids: Drink plenty of fluids, which may help reduce the risk of headache.
- Pain management: Over-the-counter pain relievers like acetaminophen can help relieve soreness or headache, but ask your doctor for the best option.
- Monitor for complications: Notify your healthcare team if you develop severe or persisting headaches, fever, drainage from the puncture site, back pain that worsens, numbness, tingling, or leg weakness.
When Should You Call the Doctor?
- Severe headache or one that worsens when upright and improves when lying down
- High fever or chills, which could indicate infection
- Redness, swelling, or drainage at the needle site
- Difficulty urinating or bowel problems
- New or worsening numbness, weakness, or tingling in the lower limbs
Results and Follow-Up
The CSF collected will be analyzed in the lab for:
- Cell counts: Number and type of white and red blood cells present
- Protein and glucose: Levels are measured and compared to normal values
- Culture: To detect infection
- Other markers: Sometimes, specialized tests such as PCR for viruses or cytology for cancer cells
Your healthcare provider will discuss the implications of these results and recommend further steps or treatments as necessary.
Potential Contraindications
- Increased intracranial pressure due to a mass (increased risk of herniation)
- Local infection at the lower back site
- Uncontrolled bleeding tendency (coagulopathy)
- Structural spine abnormalities making insertion dangerous
Your doctor will ensure that none of these risks apply to you before proceeding with a lumbar puncture.
Frequently Asked Questions (FAQ)
Q: Does a lumbar puncture hurt?
A: You will feel a needle prick for the local anesthesia and some pressure as the needle is inserted, but significant pain is uncommon. Some people report mild discomfort or an odd sensation in their back or leg. The area may be sore for a few days post-procedure.
Q: Can I eat before a lumbar puncture?
A: In many cases, you don’t need to fast before a lumbar puncture, but specific instructions may vary depending on whether sedatives or imaging are planned. Always follow your doctor’s advice.
Q: How long does the lumbar puncture take?
A: The actual procedure usually takes about 15–30 minutes, but you will be monitored for one to four hours afterward.
Q: What side effects should I expect?
A: The most common side effect is a headache, affecting up to 30% of patients, but it typically resolves within a few days. Soreness in the lower back is also possible. Serious side effects are rare.
Q: When will I get my results?
A: Standard results may be available in a few hours, but cultures and more complex tests can take several days. Your healthcare provider will advise you about the results and next steps.
Summary Table: Key Points of Lumbar Puncture
| Aspect | Details |
|---|---|
| Purpose | Diagnosis or treatment of central nervous system disorders |
| Typical duration | 15–30 minutes (may be longer with prep and observation) |
| Main risks | Headache, back pain, rare infection or bleeding |
| Recovery | Often same-day, resume normal activities within 24–48 hours |
| Follow-up | Monitor for severe headache, fever, wound issues; review test results with doctor |
Final Notes on Lumbar Puncture
A lumbar puncture is a time-tested, essential tool in diagnosing and treating neurologic conditions. With proper preparation, careful technique, and clear aftercare instructions, most people tolerate the procedure very well. Consult your healthcare provider with any questions or concerns before undergoing a lumbar puncture.
References
- https://www.ncbi.nlm.nih.gov/books/NBK367574/
- https://geekymedics.com/lumbar-puncture-osce-guide/
- https://www.merckmanuals.com/professional/neurologic-disorders/how-to-do-lumbar-puncture/how-to-do-lumbar-puncture
- https://en.wikipedia.org/wiki/Lumbar_puncture
- https://my.clevelandclinic.org/health/diagnostics/12544-lumbar-puncture-spinal-tap
- https://www.ncbi.nlm.nih.gov/books/NBK557553/
- https://www.youtube.com/watch?v=WpXGUn7eGZE
- https://radiology.ucsf.edu/patient-care/prepare/lumbar-puncture
Read full bio of Sneha Tete












