LPR vs. GERD: Understanding Key Differences, Symptoms, and Treatments
Uncover the differences between LPR and GERD, their symptoms, diagnosis, and the best approaches for effective treatment.
If you’ve ever experienced acid reflux symptoms, you might be aware of conditions like Gastroesophageal Reflux Disease (GERD). However, another type, Laryngopharyngeal Reflux (LPR), often referred to as ‘silent reflux’, can have symptoms that are more subtle yet equally impactful. This comprehensive guide will help you distinguish between LPR and GERD, understand their respective symptoms and risks, and discover the most effective ways to manage them.
What Are LPR and GERD?
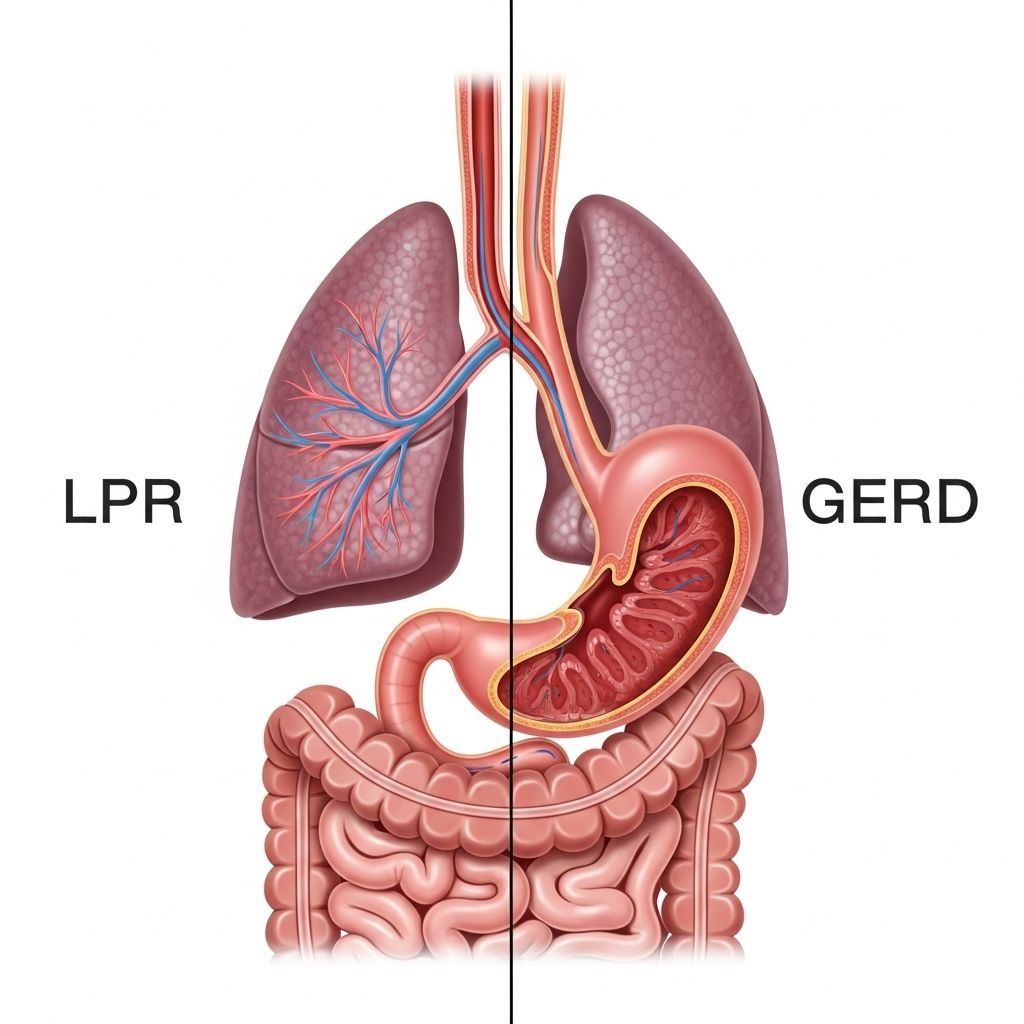
Laryngopharyngeal Reflux (LPR) and Gastroesophageal Reflux Disease (GERD) are both caused by the backward flow of stomach acid, known as acid reflux. However, they differ in the areas they affect and the symptoms they present.
- GERD occurs when stomach acid flows back into the esophagus, leading to symptoms mainly in the chest area.
- LPR happens when the refluxed stomach acid travels even higher, reaching the larynx (voice box) and pharynx (throat), irritating more sensitive tissues.
Because both are forms of acid reflux, they share some symptoms but also have distinctive features that can affect diagnosis and treatment.
What’s the Difference Between GERD and LPR?
The main difference between GERD and LPR lies in where the symptoms occur and how they manifest.
| GERD Symptoms | LPR Symptoms |
|---|---|
| Difficulty swallowing lower in the throat or chest (pharyngoesophageal dysphagia) | Difficulty starting a swallow (oropharyngeal dysphagia) |
| Burning sensation in the chest (heartburn) | Chronic cough |
| Pain in chest, especially when lying down | Vocal hoarseness |
| Burning feeling in the throat | Sore throat |
| Bad taste in the back of the throat | Shortness of breath |
| Pain that wakes you up at night | Red, swollen, or sore voice box |
Differences in Symptom Location and Recognition
- GERD usually affects the lower esophagus and presents as the classic burning sensation known as heartburn.
- LPR affects the upper airway, including the throat and larynx, causing symptoms like chronic cough, hoarseness, and sore throat, often without heartburn.
- LPR is sometimes dubbed “silent reflux” because it can go unnoticed or may be mistaken for colds, allergies, or even asthma.
Symptoms Overlap and Timing
- Both conditions can cause difficulty swallowing, known as dysphagia.
- GERD symptoms often increase after meals or when lying down.
- LPR symptoms tend to occur throughout the day and can be aggravated by eating certain foods (especially acidic foods).
Why Do LPR and GERD Occur?
At their core, both LPR and GERD result from acid reflux, when digestive acid escapes from the stomach upward into the esophagus or beyond. This happens due to:
- Weakness or relaxation of the lower esophageal sphincter (LES), a muscle that normally acts as a one-way valve.
- The acid can sometimes pass through the upper esophageal sphincter (UES) as well, causing LPR symptoms by reaching the throat and larynx.
- Physical factors such as hiatal hernia, delayed stomach emptying, or overproduction of acid.
- Lifestyle contributors like overweight, smoking, alcohol use, fatty meals, or eating large meals late at night also play a significant role.
Acid Reflux, LPR, and GERD in Infants and Children
Infants and young children can experience both GERD and LPR, but their symptoms often differ from those in adults due to developing digestive muscles and anatomy.
- In infants, GERD may manifest as vomiting, frequent spit-ups, irritability during feeding, and poor weight gain.
- LPR in babies might look like recurring cough, hoarseness, feeding difficulties, trouble breathing, or even growth stagnation.
- Because these symptoms can have various causes, always consult a pediatrician for any concerning signs—especially unexplained or severe breathing issues.
- If your child’s skin turns blue, seek emergency care immediately.
Diagnosing LPR and GERD
Diagnosing these reflux conditions can be challenging—especially with LPR, given its “silent” symptoms. Doctors typically use a combination of medical history, symptom assessment, and specialized tests, including:
- Physical examination: An ENT specialist may assess the condition of your throat, voice box, and esophagus.
- Endoscopy: A thin tube with a camera views the esophagus and throat for inflammation or damage.
- pH monitoring: A test measuring acid levels in the esophagus and throat over 24 hours.
- Barium X-rays: Imaging to visualize reflux or anatomical abnormalities.
Accurate diagnosis helps ensure targeted and effective treatment for the correct reflux type.
Risk Factors for Developing LPR or GERD
- Obesity: Excess body weight increases pressure on the stomach, promoting reflux.
- Pregnancy: Hormonal changes and abdominal pressure can weaken sphincter muscles.
- Eating habits: Large meals, spicy or fatty food, caffeine, and carbonated drinks can aggravate symptoms.
- Lifestyle: Smoking and alcohol use relax the LES and worsen reflux.
- Some medications: Certain drugs can slow digestion or relax sphincters.
- Physical conditions: Hiatal hernia, delayed stomach emptying, or connective tissue disorders.
Potential Health Risks and Complications
- Esophagitis: Chronic inflammation or erosion of the esophageal lining in GERD.
- Barrett’s esophagus: Pre-cancerous changes that may develop with untreated GERD.
- Chronic laryngitis: Prolonged hoarseness, sore throat, and voice loss from LPR.
- Respiratory problems: LPR can exacerbate asthma, bronchitis, or even cause recurring pneumonia.
- Growth delays: In infants, poor feeding and chronic reflux can lead to insufficient growth.
How Are LPR and GERD Treated?
Both GERD and LPR respond to lifestyle changes as the first line of treatment. Medications or surgery may be considered for persistent or severe cases.
Lifestyle and Dietary Adjustments
- Eat smaller, more frequent meals instead of large or late-night meals.
- Avoid trigger foods like spicy dishes, citrus fruits, caffeinated drinks, chocolate, alcohol, and fatty foods.
- Lose excess weight and wear loose-fitting clothing to ease abdominal pressure.
- Elevate the head of your bed by 6–8 inches to minimize nighttime reflux.
- Quit smoking and limit alcohol as both weaken the esophageal sphincter.
- Avoid eating 2–3 hours before bedtime to reduce reflux risk at night.
Medications
- Antacids: Fast relief for occasional, minor symptoms by neutralizing stomach acid.
- H2 blockers: Reduce acid production in the stomach (e.g., ranitidine, famotidine).
- Proton pump inhibitors (PPIs): Stronger acid suppressors for more severe cases (e.g., omeprazole, esomeprazole).
- Result times can vary: it may take 1–3 months for significant symptom relief, especially for LPR.
Advanced Interventions
- Endoscopic or surgical procedures may be considered if lifestyle and medications do not adequately control symptoms.
- Fundoplication: The most common surgery—tightens or reinforces the lower esophageal sphincter to prevent reflux.
- Magnetic beads (LINX device): A minimally invasive option to strengthen the LES.
Always follow medical advice and consult specialists such as gastroenterologists or ENT doctors for persistent or unusual symptoms.
Preventing Recurrence and Managing Both Conditions Long-Term
- Maintain a healthy weight with regular physical activity.
- Monitor foods and habits that trigger your symptoms. Keeping a food diary can help.
- Upright posture: Stay upright for at least 30 minutes after eating.
- Routine follow-ups: Regular visits with your healthcare provider can detect and address emerging complications early.
Frequently Asked Questions (FAQs)
Can I have both GERD and LPR at the same time?
Yes. Many individuals experience both conditions, with one often more prominent than the other. They may require a combination of treatments depending on symptoms and severity.
Is heartburn always present in acid reflux?
No. LPR, sometimes called “silent reflux,” often occurs without obvious heartburn. Instead, you may notice cough, sore throat, or voice changes.
How can I tell if my child’s reflux symptoms are serious?
If your child experiences significant trouble feeding, poor growth, breathing difficulties, or any episode where they have a blue tinge to their skin, seek medical care immediately. Mild symptoms should be evaluated by a pediatrician or pediatric ENT specialist.
How quickly will my symptoms improve after starting treatment?
For both LPR and GERD, symptom relief with medication or lifestyle changes may take several weeks to months. LPR, in particular, often requires a longer period for noticeable improvement. Consistency in following lifestyle advice is key.
Will I always need medication for LPR or GERD?
Many people find long-term relief through lifestyle adjustments alone, especially when symptoms are mild. However, if symptoms persist or worsen, medications or even surgical interventions may be necessary for effective control.
Are there any long-term risks if LPR or GERD are left untreated?
Yes. Untreated reflux can lead to serious health complications such as esophageal ulcers, Barrett’s esophagus, chronic laryngitis, recurring pneumonia, or increased risk of esophageal cancer. Early detection and intervention are crucial.
Key Takeaways
- LPR and GERD are both forms of acid reflux but affect different parts of the body and can have unique symptoms.
- GERD is often associated with heartburn and chest symptoms; LPR is more likely to cause throat irritation, cough, and voice changes.
- Diagnosis relies on a combination of history, examination, and tests like endoscopy or pH monitoring.
- Lifestyle modifications, dietary changes, and medication are the backbone of treatment for both conditions.
- If left untreated, both can result in significant complications—seek medical help for persistent or severe symptoms, especially in children.
When in doubt, always discuss your symptoms with a qualified healthcare provider to establish an accurate diagnosis and effective, personalized treatment plan.
References
- https://www.healthline.com/health/digestive-health/lpr-vs-gerd
- https://www.bannerhealth.com/healthcareblog/teach-me/how-silent-reflux-is-different-from-acid-reflux
- https://alpineent.com/the-difference-between-gerd-lpr/
- https://naugatuckvalleyent.com/blog/understanding-gerd-and-lpr-key-differences-symptoms-and-solutions-for-lasting-relief-in-wolcott-ct/
- https://thefunctionalgutclinic.com/post/difference-between-lpr-and-gerd
- https://my.clevelandclinic.org/health/diseases/15024-laryngopharyngeal-reflux-lpr
- https://www.enthealth.org/conditions/gerd-and-lpr/
- https://pubmed.ncbi.nlm.nih.gov/12353431/
Read full bio of Sneha Tete












