LPR vs. GERD: Understanding the Differences, Symptoms, and Treatments
Explore the crucial distinctions between LPR and GERD, their unique symptoms, causes, diagnosis, and how to manage each effectively.
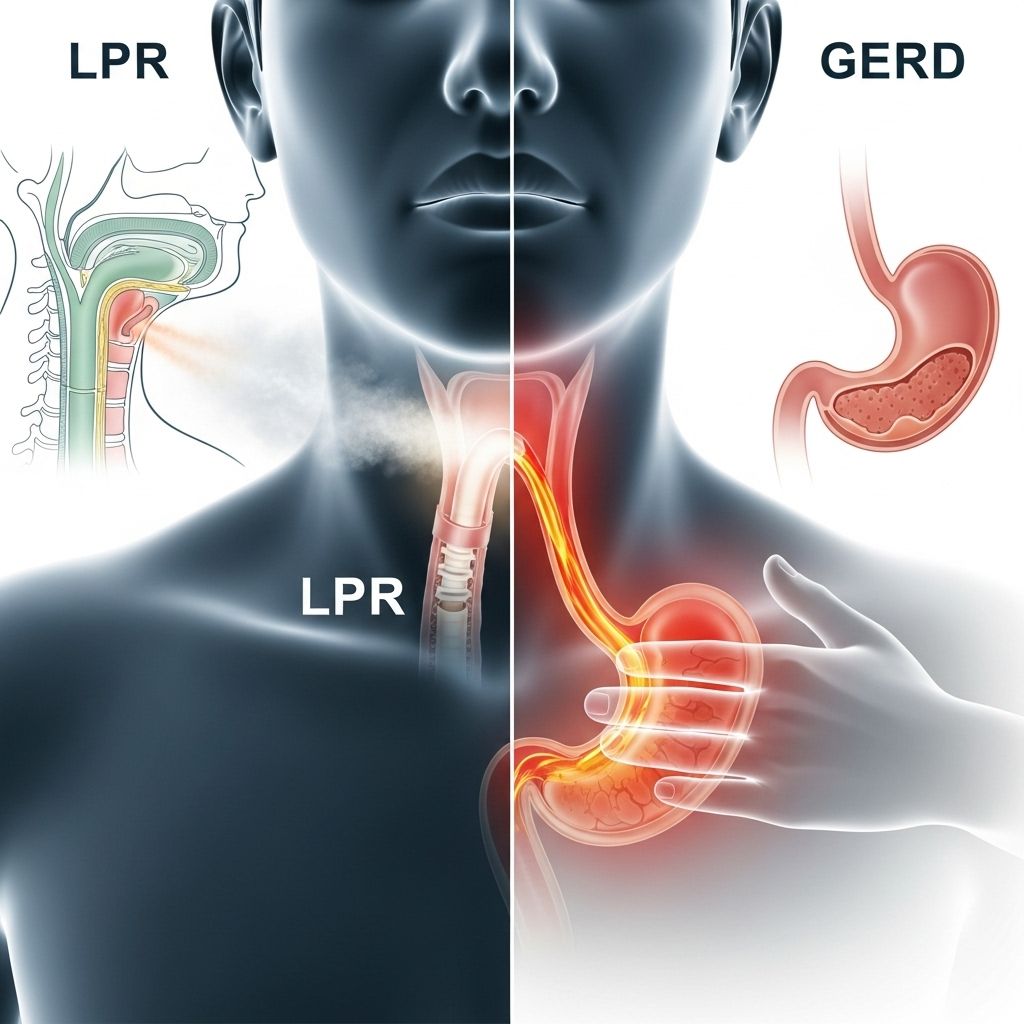
Laryngopharyngeal reflux (LPR) and gastroesophageal reflux disease (GERD) are frequently confused gastrointestinal conditions linked by the flow of acidic stomach contents, but they differ markedly in terms of symptoms, affected areas, and management strategies. This article explores their distinct symptoms, causes, diagnosis, treatments, and highlights special considerations for children and infants.
What Are LPR and GERD?
Gastroesophageal reflux disease (GERD) occurs when stomach acid regularly flows back into the esophagus, causing irritation and typical digestive symptoms such as heartburn. In contrast, laryngopharyngeal reflux (LPR) happens when stomach acid travels further up, reaching the throat (pharynx) and voice box (larynx), leading to vocal and respiratory symptoms that are often mistaken for allergies or respiratory illnesses.
- GERD mainly affects the lower esophagus and is associated with classic heartburn and chest discomfort.
- LPR, often called “silent reflux,” primarily involves the throat and voice box, causing hoarseness and cough rather than heartburn, and may be asymptomatic otherwise.
Symptoms: How GERD and LPR Differ
Although GERD and LPR share the same underlying mechanism—backflow of stomach acid—the symptoms they produce are notably different.
| GERD Symptoms | LPR Symptoms |
|---|---|
| Heartburn (burning in chest) | Chronic cough |
| Chest pain, worsened lying down | Hoarseness or voice changes |
| Burning feeling in throat | Sore or red, swollen voice box |
| Bad or acid taste in back of throat | Frequent throat clearing |
| Dysphagia (feeling food stuck lower in throat or chest) | Difficulty starting swallowing (oropharyngeal dysphagia) |
| Regurgitation of food or sour liquid | Post-nasal drip, persistent sore throat |
| Pain at night, disrupts sleep | Shortness of breath, asthma-like symptoms |
Key Point: GERD most commonly causes burning chest pain (heartburn), while LPR more often causes throat symptoms and may not cause heartburn at all, making it harder to diagnose.
Unique Symptom Patterns
- GERD frequently leads to heartburn and regurgitation after eating, especially when lying down or bending over.
- LPR is often “silent,” with symptoms such as a chronic cough, hoarseness, or the sensation of a lump in the throat (globus sensation), sometimes with minimal or no heartburn.
- LPR may mimic allergies or a persistent cold, leading to misdiagnosis as an upper respiratory issue.
Children and Infants: Differences in Pediatric Symptoms
Reflux manifests differently in infants and children, and may lead to the following symptoms:
- Feeding difficulties and frequent spitting up
- Persistent cough or wheezing
- Poor weight gain or growth delays
- Trouble breathing or noisy breathing
Special caution: Blue coloring of a child’s skin or lips (cyanosis) is a medical emergency and requires immediate attention.
Mechanisms: How Acid Reflux Occurs
Both GERD and LPR result from dysfunction of the lower esophageal sphincter (LES), a muscular valve preventing stomach contents from moving backward into the esophagus. If this sphincter weakens or relaxes inappropriately:
- GERD: Stomach acid and sometimes food regurgitate into the lower esophagus, causing esophageal irritation and heartburn.
- LPR: Acid travels further up, reaching the throat and voice box, irritating the delicate tissues and leading to vocal changes, coughing, and sore throat.
Some degree of overlap exists: all LPR involves GERD, but not all GERD progresses to LPR.
Risk Factors for GERD and LPR
Certain lifestyle and biological factors contribute to both GERD and LPR, including:
- Obesity
- Poor diet (high-fat, spicy, caffeinated, or acidic foods)
- Hiatal hernia
- Smoking or alcohol consumption
- Pregnancy
- Delayed stomach emptying
Reducing these risks can help manage symptoms and improve outcomes for both conditions.
Diagnosis: How Are GERD and LPR Identified?
Correct diagnosis is key to managing GERD and LPR. Because LPR often lacks typical heartburn, it may be misdiagnosed as a respiratory or allergic disorder such as asthma, sinusitis, or chronic post-nasal drip.
Diagnostic tools may include:
- Medical history and symptoms review: A doctor asks about frequency, nature, and timing of symptoms.
- Physical examination: May involve examining the throat and larynx with a flexible camera (laryngoscopy).
- Upper endoscopy (EGD): Visualization of the esophagus, stomach, and sometimes throat to detect inflammation or injury.
- pH monitoring: Testing acidity levels in the esophagus and throat over 24 hours can confirm abnormal acid exposure.
- Imaging (X-ray, barium swallow): To assess swallowing function or detect anatomical problems.
Treatment Options: Managing GERD and LPR
Lifestyle changes and dietary adjustments form the foundation of treatment for both conditions, but approaches may differ based on symptom patterns.
Lifestyle and Dietary Changes
- Eat smaller, more frequent meals rather than large ones.
- Avoid eating within 2–3 hours before bedtime.
- Limit high-fat, spicy, or acidic foods.
- Reduce consumption of caffeine and alcohol.
- Maintain a healthy weight.
- Avoid tight-fitting clothing that puts pressure on the stomach.
- Elevate the head of the bed to prevent nighttime symptoms.
- Quit smoking.
Medications
- Antacids: Neutralize stomach acid for quick relief.
- H2 blockers (e.g., ranitidine): Reduce acid production.
- Proton pump inhibitors (PPIs, e.g., omeprazole): More powerfully reduce acid secretion in the stomach.
- Prokinetics: Help stomach empty faster, reducing reflux risk.
Symptom improvement with medications may take 1–3 months, especially for LPR.
Surgical and Advanced Procedures
- Fundoplication: A surgical procedure to strengthen the lower esophageal sphincter and block acid reflux.
- Magnetic sphincter augmentation: A ring of magnetic beads reinforces the sphincter, preventing reflux.
- Surgery is reserved for severe or refractory cases not responding to conservative management.
Overlapping and Unique Aspects of GERD and LPR
LPR can exist on its own but is often seen in combination with GERD. It is estimated that up to 20% of people have GERD, and a further 5–30% have LPR, with some overlap.
- All LPR passes through GERD: Acid must travel through the esophagus first, so LPR always involves GERD, but not all GERD leads to LPR.
- LPR is harder to detect: Because it doesn’t cause typical digestive symptoms, it is often misdiagnosed or overlooked.
When to See a Doctor?
- If you experience recurrent or severe symptoms such as persistent heartburn, chronic cough or hoarseness, or difficulty swallowing.
- For infants and young children: any signs of breathing difficulties, feeding struggles, poor growth, or blue skin/lips (medical emergency).
- When over-the-counter remedies do not control symptoms.
FAQs: Frequently Asked Questions About LPR and GERD
What is the major difference between GERD and LPR?
GERD mainly affects the lower esophagus, causing heartburn and digestive symptoms, while LPR impacts the throat and voice box, causing hoarseness, cough, and sore throat—often without heartburn.
Can a person have both GERD and LPR?
Yes. Many people with LPR also have underlying GERD, since stomach acid must pass through the esophagus before reaching the throat. However, not all GERD patients develop LPR.
Are LPR and silent reflux the same thing?
Yes. LPR is frequently called “silent reflux” because it may lack the heartburn characteristic of GERD, making its symptoms less obvious.
Why does LPR sometimes get mistaken for allergies or respiratory illness?
Because LPR predominantly causes symptoms like cough, throat clearing, hoarseness, and sore throat, it is often misdiagnosed as allergies, sinusitis, or asthma.
How are GERD and LPR typically diagnosed?
Diagnosis is based on symptom patterns, physical examination (often with laryngoscopy), endoscopy, and pH monitoring to measure acid exposure in the esophagus and throat.
Can children and infants have LPR or GERD?
Yes, but symptoms differ. Watch for feeding difficulties, persistent cough, abnormal breathing, and failure to thrive in children. Severe cases require urgent medical care.
What is the first step if I suspect I have LPR or GERD?
Make healthy lifestyle and dietary changes, record symptoms, and consult with a healthcare provider for evaluation and appropriate testing.
Summary Table: GERD vs. LPR At a Glance
| Aspect | GERD | LPR |
|---|---|---|
| Main area affected | Lower esophagus | Throat/voice box (larynx/pharynx) |
| Common symptoms | Heartburn, chest pain, regurgitation | Chronic cough, hoarseness, sore throat |
| Swallowing issues | Difficulty lower in throat/chest | Difficulty starting to swallow |
| Misdiagnosis | Less common | Allergies, sinusitis, asthma |
| Heartburn present? | Usually | Rarely |
| Treatment | Lifestyle, antacids, PPIs, surgery | Lifestyle, antacids, PPIs, voice rest |
Takeaway
LPR and GERD both stem from stomach acid moving in the wrong direction, but their symptoms and management differ significantly. Recognizing their differences is key to effective diagnosis, treatment, and symptom control—especially in children, who may not show classic signs. If you suspect LPR or GERD, consult your healthcare provider for a personalized plan.
References
- https://www.healthline.com/health/digestive-health/lpr-vs-gerd
- https://www.bannerhealth.com/healthcareblog/teach-me/how-silent-reflux-is-different-from-acid-reflux
- https://naugatuckvalleyent.com/blog/understanding-gerd-and-lpr-key-differences-symptoms-and-solutions-for-lasting-relief-in-wolcott-ct/
- https://thefunctionalgutclinic.com/post/difference-between-lpr-and-gerd
- https://my.clevelandclinic.org/health/diseases/15024-laryngopharyngeal-reflux-lpr
- https://www.enthealth.org/conditions/gerd-and-lpr/
- https://pubmed.ncbi.nlm.nih.gov/12353431/
- https://baycareclinic.com/news-and-more/acid-reflux-gerd-and-lpr-know-the-difference/
Read full bio of Sneha Tete












