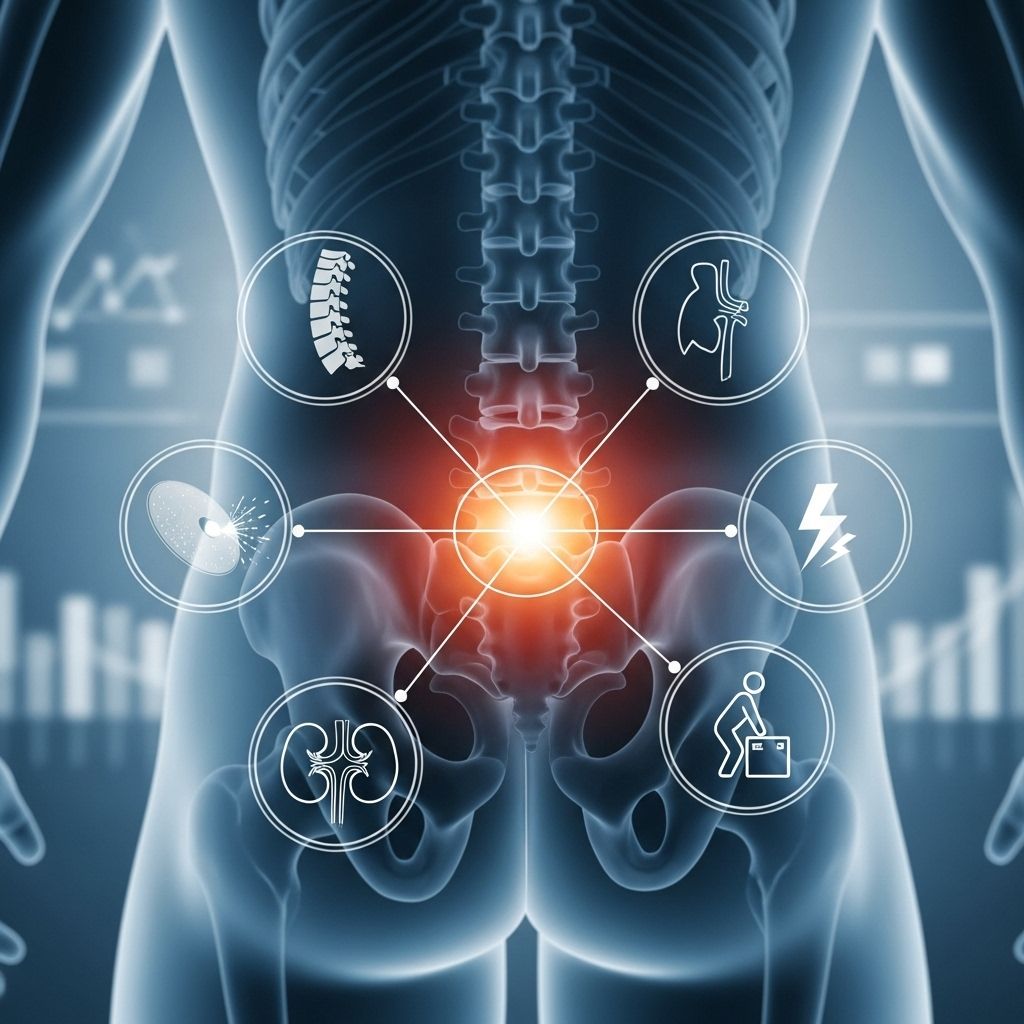
Lower Back Pain: What Could It Be?
Explore the numerous causes, symptoms, and management strategies for lower back pain, helping you better understand this common condition.
Lower back pain remains one of the most frequent reasons for physician visits and missed workdays worldwide. The lower back, or lumbar region, bears the weight of the upper body and is subject to a broad range of physical stresses. While some causes are acute and resolve with self-care, others may be chronic and require targeted treatments or even surgical interventions. Understanding the diverse causes, symptoms, and management strategies is crucial for effective relief and prevention.
Understanding Lower Back Pain
The lower back, or lumbar spine, serves as a structural support for most of the body’s upper weight and is a complex matrix comprised of bones, muscles, ligaments, joints, nerves, and intervertebral discs. Its core functions include flexibility, mobility, and protection for delicate neural structures.
- Bones: Vertebrae create the spinal structure and house the spinal cord.
- Discs: Cushion-like pads between vertebrae that absorb shock.
- Muscles and ligaments: Provide stability and movement.
- Nerves: Emerge from the spine and control movements and sensations in the lower body.
Given its complex anatomy and multiple functions, the lower back is especially vulnerable to a variety of pain types and injuries.
Common Causes of Lower Back Pain
Lower back pain can result from multiple sources, often categorized by the specific tissues or conditions involved. Here are the most prevalent causes:
- Muscle or Ligament Strains: Overstretching or microscopic tears during heavy lifting, sudden movements, or poor posture commonly lead to acute back pain. Typical in younger adults and those performing physical labor.
- Bulging or Herniated Discs: When a spinal disc’s radial fibers weaken or rupture, the soft interior can protrude and press on nearby nerves, resulting in localized pain or pain radiating down the leg (sciatica). Most disc problems occur in the lower lumbar area.
- Arthritis and Degenerative Changes: Osteoarthritis and degenerative disc disease lead to wear and tear of the spinal joints and discs over time, often resulting in stiffness, decreased mobility, and sometimes nerve compression due to bone spurs or narrowing of the spinal canal (spinal stenosis).
- Sacroiliac Joint Dysfunction: Inflammation or abnormal movement of the joint connecting the sacrum to the pelvis can cause pain that mimics lumbar spine disorders.
- Spinal Instability or Spondylolisthesis: Slippage of one vertebra over another, typically due to age, arthritis, or congenital conditions, can provoke both pain and nerve symptoms.
- Fractures: Vertebral fractures are often due to osteoporosis in older adults, but can also result from trauma.
- Other Medical Conditions: Infections, tumors, or diseases such as inflammatory arthritis may also cause lower back pain, though less commonly.
| Cause | Typical Symptoms | Common Risk Groups |
|---|---|---|
| Muscle or Ligament Strain | Achy, localized pain; worsens with movement | Young adults, physical laborers |
| Herniated Disc | Shooting pain; may radiate down leg; numbness/tingling | Adults 30–50, prior back injury |
| Arthritis/Spinal Stenosis | Stiffness, pain, sometimes nerve symptoms | Older adults (50+) |
| Sacroiliac Joint Issues | Pain in buttocks/lower back; worsens with standing/walking | Postpartum women, those with leg length differences |
| Fractures | Sharp pain, sudden onset, worsened with movement | Older adults, osteoporosis patients |
Symptoms and Types of Lower Back Pain
Lower back pain symptoms can vary widely in intensity, duration, and character. Categorizing the pain helps guide both diagnosis and treatment.
- Acute Pain: Lasts less than 6 weeks, typically from injury or strain.
- Subacute Pain: Persists for 6 to 12 weeks; may result from ongoing tissue healing or a moderate injury.
- Chronic Pain: Continues beyond 12 weeks, frequently due to degenerative changes, nerve issues, or less identifiable factors.
The character of the pain often offers clues to the underlying cause:
- Muscle and Ligament Pain: Achy, sore, tight, sometimes with muscle spasms. Often relieved by rest, heat, or massage.
- Bone Pain: Frequently described as stiff, deep, and achy. Associated with arthritis, fractures, or bone disorders.
- Nerve Pain: Burning, shooting, electrical sensations. May include numbness, tingling, or weakness radiating down the leg—typical of sciatica or nerve root compression.
- Centralized Pain: Diffuse aching not clearly linked to a single anatomic structure; may reflect nervous system changes or amplification.
Distinguishing Features: Sciatica vs. Typical Low Back Pain
Sciatica is a specific type of lower back pain that involves irritation or compression of the sciatic nerve, often by a herniated disc or a bone spur. It is characterized by:
- Pain radiating from the lower back through the buttock and down one leg, sometimes extending below the knee
- Numbness, tingling, or muscle weakness along the leg
- Symptoms aggravated by prolonged sitting, sneezing, or coughing
Typical low back pain, on the other hand, is often localized to the lumbar area and may be associated with stiffness or soreness rather than radiating sharp pain.
Risk Factors and Predisposing Conditions
Several factors can predispose individuals to develop lower back pain, either by increasing physical strain or by promoting degenerative changes in the spine:
- Age: Degenerative changes become more common after age 30.
- Obesity: Excess weight places added stress on the lumbar spine.
- Poor Posture and Sedentary Lifestyle: Weak core muscles and prolonged sitting increase the risk for injury and strain.
- Occupational Factors: Jobs requiring heavy lifting, bending, twisting, or repetitive movements contribute to higher rates of back pain.
- Smoking: Reduces blood flow to spinal tissues and hampers healing.
- Genetics: Family history can play a role in specific spinal conditions, including degenerative disc disease.
When to See a Doctor
Most episodes of lower back pain improve with conservative measures. However, it is important to seek medical attention if you experience:
- Pain persisting beyond a few weeks without improvement
- Severe pain unresponsive to rest or medications
- Bladder or bowel dysfunction (incontinence or retention)
- Progressive leg weakness or numbness
- History of trauma resulting in back pain (e.g., fall, accident)
- Unexplained weight loss, fever, or history of cancer
Diagnosis: How Is Lower Back Pain Evaluated?
Diagnosis typically starts with a detailed history and physical examination, focusing on pain characteristics, physical function, neurological symptoms, and risk factors. Your physician may perform:
- Observation and palpation of the back and surrounding structures
- Range of motion and neurological testing
- Assessment for localized tenderness, muscle spasms, or reflex changes
Imaging studies or specialized tests may be required if:
- Severe, persistent, or worsening symptoms are present
- There is suspicion of nerve root involvement or serious underlying pathology
- Initial treatments have not improved the condition within 4–6 weeks
Common diagnostic tests include:
- X-rays: Helpful for evaluating bone injury, fractures, or structural abnormalities.
- MRI or CT scan: Provide detailed images of discs, nerves, and soft tissues; used for suspected nerve compression, cancer, or infection.
- Blood tests: Rule out underlying infection or inflammatory conditions.
Treatment Options for Lower Back Pain
Treatment depends on the underlying cause, severity, and duration of symptoms. The majority of lower back pain cases improve without invasive procedures. Approaches include:
- Self-Care Measures:
- Short-term rest and gradual return to activity
- Use of ice or heat therapy
- Gentle stretching and core-strengthening exercises
- Medications:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and inflammation
- Muscle relaxants for spasm relief
- Rarely, short courses of stronger pain relievers if other measures fail
- Physical Therapy:
- Supervised exercises to improve flexibility, posture, and strength
- Manual therapy, massage, or other modalities as needed
- Injections:
- Epidural steroid injections for severe nerve-related pain (e.g., sciatica)
- Facet or sacroiliac joint injections for joint-related pain
- Surgery: Reserved for rare cases with significant structural issues, such as herniated discs causing progressive weakness, impaired bladder/bowel control, or spinal instability/crushing fractures.
Prevention of Lower Back Pain
While not all causes of lower back pain are preventable, the following strategies can reduce risk and limit recurrence:
- Maintain regular physical activity and core-strengthening exercises
- Use proper ergonomics at work and home
- Avoid heavy lifting or learn proper lifting techniques
- Maintain a healthy weight
- Quit smoking to support tissue healing and disc health
- Monitor and treat underlying medical conditions, such as osteoporosis
Frequently Asked Questions (FAQs)
What is the most common cause of lower back pain?
The most frequent cause of lower back pain is muscle or ligament strain due to overuse, improper lifting, or sudden awkward movements. Chronic cases often stem from degenerative changes such as osteoarthritis or disc disease.
How can I tell if my lower back pain is serious?
Warning signs that require prompt evaluation include severe or worsening pain, nerve symptoms (numbness, tingling, weakness), bowel or bladder control problems, unexplained weight loss, or back pain following trauma.
Can lower back pain be prevented?
While not all cases can be prevented, regular exercise, ergonomic adjustments, proper lifting, weight management, and avoidance of smoking greatly reduce risk.
What are first-line treatments for acute lower back pain?
First-line measures include gentle activity, ice or heat therapy, short-term NSAIDs, stretching, and gradual reconditioning. Bed rest is generally discouraged.
When is surgery necessary for lower back pain?
Surgery is reserved for cases involving progressive neurologic loss, significant spinal instability, or persistent pain that does not improve with conservative approaches.
Does age affect my risk for lower back pain?
Yes, age increases the likelihood of degenerative spinal changes due to year-over-year wear and tear on discs and joints, making pain and stiffness more common with advancing age.
Key Takeaways
- Lower back pain is extremely common and usually due to muscle, ligament, disc, or joint issues.
- Most cases improve with conservative treatments such as rest, exercise, and medications.
- See a healthcare provider if pain persists, is severe, involves nerve symptoms, or follows trauma.
- Healthy movement habits and proactive strategies help reduce the risk and recurrence of pain.
If you have questions or persistent symptoms, consult a healthcare professional for a tailored diagnosis and treatment plan.
References
- https://striverehab.com/what-causes-lower-back-pain/
- https://www.youtube.com/watch?v=TE14fB8ppO8
- https://www.youtube.com/watch?v=QRwCzu0T4Q4
- https://pure.johnshopkins.edu/en/publications/persistent-back-pain-and-sciatica-in-the-united-states-patient-ch-3
- https://www.youtube.com/watch?v=eOcgOWCsXVY
- https://pure.johnshopkins.edu/en/publications/spine-pain
Read full bio of medha deb












