Long-Acting Insulin: How It Works, Types, and What to Expect
A comprehensive breakdown of long-acting insulin, its use, mechanism, types, and what people with diabetes need to know.
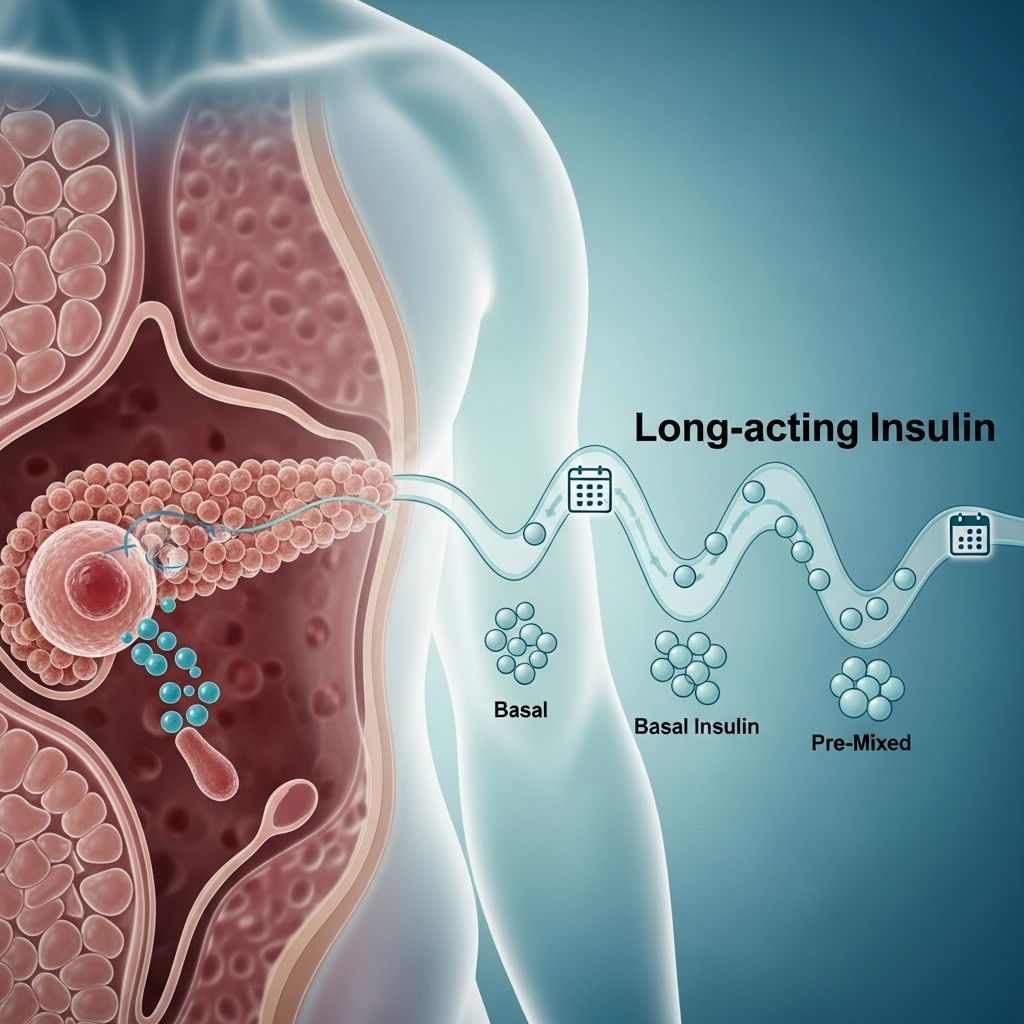
Long-acting insulin plays a crucial role in helping people with diabetes maintain stable blood sugar levels throughout the day and night. Unlike short-acting or rapid-acting insulin, which addresses blood sugar spikes at mealtimes, long-acting insulin delivers a steady, baseline amount of insulin to mimic the body’s natural background insulin production.1
What Is Insulin and Why Is It Important?
Insulin is a hormone produced by the pancreas. Its primary role is to move glucose (sugar) from your blood into cells, where it can be used for energy or stored for future use. People with diabetes either cannot produce enough insulin (type 1 diabetes) or cannot effectively use the insulin their body makes (type 2 diabetes).1
For those needing insulin therapy, different types of insulin can be used to closely replicate how a healthy pancreas functions:
- Mealtime insulin: Covers rises in blood sugar after food.
- Background or basal insulin: Maintains stable blood sugar between meals and overnight. This is where long-acting insulin plays an essential role.
Types of Insulin and How They Differ
Insulin can be categorized based on how quickly it starts to work (onset), when it is most effective (peak), and how long it remains active in the body (duration).1
| Type | Onset | Peak | Duration |
|---|---|---|---|
| Rapid-acting | ~15 min | ~1 hour | 3–5 hours |
| Short-acting | 30–60 min | 2–3 hours | 3–6 hours |
| Intermediate-acting | 2–4 hours | 8 hours | 12–16 hours |
| Long-acting | 2–4 hours | Minimal or none | Up to 24 hours (some longer) |
| Pre-mixed | Varies | Varies | Varies |
Each type serves a specific role. Long-acting insulin typically has an onset of 2 to 4 hours, does not peak, and is active for up to 24 hours or more, providing a consistent insulin level.1,2
How Does Long-Acting Insulin Work?
Long-acting insulin is designed to mimic the steady, low-level insulin release of a healthy pancreas between meals and overnight. This basal insulin helps keep your blood sugar stable when you are not eating.1,2
Unlike rapid- or short-acting insulins that have a distinct peak and wear off more quickly, long-acting insulins remain relatively flat (no peak), making them ideal for controlling baseline glucose levels over a 24-hour period or longer.2
Long-acting insulin is often referred to as basal insulin or background insulin. People with type 1 diabetes will typically use long-acting insulin as their basal insulin and add short- or rapid-acting insulins with meals for better overall control.
Why Long-Acting Insulin Is Needed
- Type 1 diabetes: The pancreas does not produce insulin, making daily (often multiple daily) injections of both long- and short-acting insulin necessary.
- Type 2 diabetes: As the disease progresses, the body may make less insulin or use it inefficiently. Some people require long-acting insulin to maintain blood sugar within target ranges, in combination with other medications.
Types of Long-Acting and Ultra-Long-Acting Insulin
Several synthetic forms of long-acting insulin are available today. Although all share a similar prolonged, steady action profile, each has slight differences regarding onset, duration, and concentration. The most commonly prescribed long-acting insulins include:1,2
- Insulin glargine (Lantus, Basaglar): Lasts up to 24 hours.
- Insulin detemir (Levemir): Lasts 18 to 23 hours.
- Insulin glargine (Toujeo): An ultra-long-acting version, lasts over 36 hours.
- Insulin degludec (Tresiba): Ultra-long-acting, lasts up to 42 hours.
Even though Lantus and Toujeo are both based on insulin glargine, they have different concentrations—so they are not interchangeable. Each requires its own prescription and dose adjustment.1
Ultra-Long-Acting Insulins
- Toujeo (insulin glargine): Lasts more than 36 hours, suited for people who need highly stable background coverage.
- Tresiba (insulin degludec): Lasts up to 42 hours, offers flexible dosing time for people with varying routines.1,2
How to Use Long-Acting Insulin
Injection and Delivery Methods
Long-acting insulin is administered through subcutaneous injections—under the skin—using a syringe, insulin pen, or, less commonly, an insulin pump.2
- Never take long-acting insulin as a pill; digestive enzymes will break it down before it becomes active.2
- Common injection sites include the abdomen, upper arms, thighs, or buttocks. Rotating sites helps prevent skin complications.
- Some people use electronic insulin pumps that can deliver both basal (long-acting) and bolus (mealtime) insulin automatically.2
When to Take Long-Acting Insulin
- Many long-acting insulins are dosed once daily, but some may require twice-daily administration depending on the insulin type and individual needs.2
- Ultra-long-acting insulins typically require only one daily injection.
- Follow your healthcare provider’s instructions on timing and dose, as this is individualized.
Dosage, Adjustments, and Monitoring
Your healthcare provider determines the starting dose based on your weight, blood sugar levels, and overall insulin requirements. Typically, a lower dose is started and then gradually adjusted upward to reach the target blood sugar, allowing the body to adapt.2
Reasons for dosage adjustments:
- Changes in diet or mealtime routines
- Physical activity increased or decreased
- Weight gain or loss
- Illness or infections
- Pregnancy or other hormonal changes
It is vital to monitor blood sugar regularly and report any significant changes to your healthcare provider. Long-acting insulin does not usually cover post-meal blood sugar spikes—if you experience high readings after meals, your provider may add or adjust rapid- or short-acting insulin.2
Side Effects and Safety Considerations
All insulins can cause side effects. Most are mild and manageable with appropriate usage:
- Low blood sugar (hypoglycemia): The most common risk of insulin therapy, especially if meals are skipped, or excess insulin is used.
- Weight gain: Some people may experience modest weight gain.
- Allergic reactions: Rare, but can occur. Signs include rash, itching, or swelling at the injection site.
- Injection site reactions: Redness, swelling, or discomfort, usually resolves with site rotation.
- Lipodystrophy: Over time, repeated injections in the same area may cause changes in the fatty tissue under your skin.3
Most side effects are mild, but severe hypoglycemia can be life-threatening. Learn to recognize symptoms of low blood sugar (shakiness, sweating, confusion, rapid heartbeat) and keep a quick source of glucose available.
Tips for Safe and Effective Use of Long-Acting Insulin
- Follow your prescribed dosing schedule closely. Do not skip or double up on doses without medical advice.
- Rotate injection sites to avoid irritation or tissue changes.
- Store insulin according to the manufacturer’s instructions—usually in a refrigerator before opening, and at room temperature after opening (for a limited time).
- Always check the appearance of your insulin before use. Do not use if it looks cloudy or contains particles (unless specified for certain insulins).
- Carry supplies with you when traveling, and avoid exposing insulin to extreme hot or cold temperatures.
Comparison of Long-Acting and Ultra-Long-Acting Insulins
| Insulin | Brand Name(s) | Duration | Peak Time | How Often Taken |
|---|---|---|---|---|
| Glargine | Lantus, Basaglar | Up to 24 hours | None or minimal | Once daily |
| Detemir | Levemir | 18–23 hours | None or minimal | Once or twice daily |
| Glargine (high-strength) | Toujeo | Over 36 hours | None or minimal | Once daily |
| Degludec | Tresiba | Up to 42 hours | None or minimal | Once daily |
Frequently Asked Questions (FAQs)
What is the main difference between long-acting and rapid-acting insulin?
Long-acting insulin has a delayed onset, no peak effect, and lasts for up to or longer than 24 hours, providing a stable background insulin level. Rapid-acting insulin works quickly and covers mealtime blood sugar rises.
Who should use long-acting insulin?
People with type 1 diabetes require long-acting insulin as part of their fundamental therapy. Some people with type 2 diabetes may also need it when other medications are insufficient to control blood glucose.
How should I store long-acting insulin?
Unopened insulin should be kept in the refrigerator. Once opened, it can usually be stored at room temperature for up to 28 days, but always follow the manufacturer’s instructions.
Can long-acting insulin be used alone?
In some cases of type 2 diabetes, yes. However, most people with type 1 diabetes or those with more advanced type 2 diabetes will also need rapid-acting insulin to control blood sugar spikes after meals.
Are different brands or forms of long-acting insulin interchangeable?
No. Even insulin products with the same base (like Lantus and Toujeo) may have different dose strengths and absorption rates, so always use the specific product and dose prescribed for you.
Key Takeaways
- Long-acting insulin is essential for stable, round-the-clock blood sugar control in diabetes.
- It must be injected or delivered via pump, never taken orally.
- Various formulations are available, each with different durations and concentrations—work with your healthcare provider to find the best regimen for your needs.
- Proper injection technique, site rotation, and adherence to storage recommendations are important for safety and effectiveness.
- Always monitor for side effects, especially hypoglycemia, and keep your provider informed of any changes in your health, diet, or activity levels.
References
- https://www.healthline.com/health/diabetes/long-acting-insulin
- https://www.medicalnewstoday.com/articles/316674
- https://diabetesjournals.org/care/article/39/Supplement_2/S172/30337/New-Long-Acting-Basal-Insulins-Does-Benefit
- https://www.healthline.com/health/type-2-diabetes/insulin-chart
- https://www.healthline.com/health/video/the-complete-guide-to-insulin-and-how-to-use-it
- https://www.ncbi.nlm.nih.gov/books/NBK557756/
- https://www.medicalnewstoday.com/articles/drugs-lantus
- https://www.mayoclinic.org/diseases-conditions/diabetes/in-depth/diabetes-treatment/art-20044084
- https://diabetes.org/health-wellness/medication/insulin-basics
Read full bio of medha deb












