Leukemia Stages: Understanding Classification and Disease Progression
Learn how leukemia is staged, why staging matters, and how it guides treatment choices and outlook.

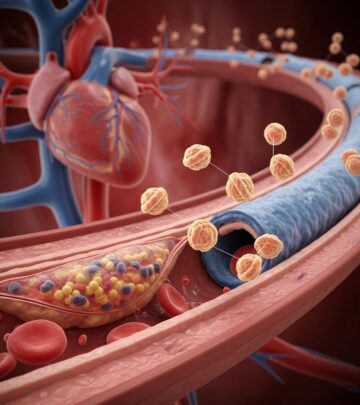
Leukemia is a complex blood cancer that arises in the bone marrow and blood. Unlike many solid tumors, leukemia does not form a single mass, so its staging and classification are uniquely based on blood cell counts, lab results, and disease spread. This article explores how leukemia is staged, why staging matters, the systems used for various subtypes, and the implications for treatment and prognosis.
What Is Leukemia?
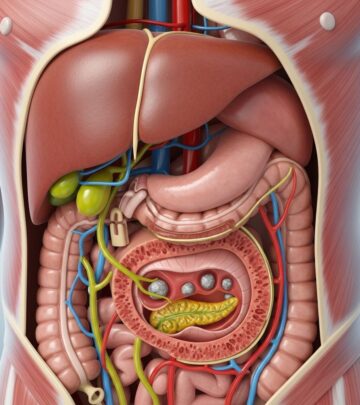
Leukemia is a cancer of the blood-forming tissues, including the bone marrow and lymphatic system. It leads to abnormal white blood cell production, which can crowd out normal blood cells and disrupt essential body functions. Leukemia is broadly classified by how fast it progresses (acute or chronic) and the type of blood cell affected (lymphoid or myeloid).
- Acute leukemia: Develops quickly, often requiring urgent treatment.
- Chronic leukemia: Develops slowly and may not cause symptoms for years.
- Lymphocytic leukemia: Affects lymphoid cells.
- Myeloid leukemia: Affects myeloid cells.
How Is Leukemia Staged?
Staging describes the extent or progression of leukemia at diagnosis. For most cancers, staging is based on tumor size and spread (such as the TNM system), but because leukemia doesn’t form solid tumors, other features are assessed:
- Numbers and types of abnormal blood cells
- Involvement of organs such as lymph nodes, liver, and spleen
- Bone marrow findings and genetic abnormalities
Staging helps doctors:
- Guide treatment decisions
- Estimate prognosis
- Track disease progression or remission over time
Why Staging in Leukemia Differs from Other Cancers
Leukemia cells originate in the bone marrow and then spill into the bloodstream, circulating throughout the body. Therefore, at diagnosis, leukemia is essentially already considered a systemic disease. As a result, the critical determinants for staging and prognosis are:
- Blood and bone marrow findings (cell counts, cell types, genetic changes)
- Presence or absence of symptoms (anemia, frequent infections, bleeding)
- Enlargement of lymph nodes, spleen, or liver
Most types of leukemia have unique classification and staging systems based on their biological behaviors.
Staging and Classification by Leukemia Type
There are four main types of leukemia, and each is staged or classified differently:
- Chronic Lymphocytic Leukemia (CLL)
- Acute Lymphoblastic Leukemia (ALL)
- Acute Myeloid Leukemia (AML)
- Chronic Myeloid Leukemia (CML)
- Rare subtypes: B-cell and T-cell Prolymphocytic Leukemia (B-PLL, T-PLL)
Chronic Lymphocytic Leukemia (CLL) Staging
CLL is one of the few leukemias with well-defined staging systems. The two main systems are the Rai system (primarily used in the United States) and the Binet system (commonly used in Europe and Australia).
The Rai Staging System (U.S.)
| Stage | Description | Key Features |
|---|---|---|
| Stage 0 | Early stage, high white blood cell count | No physical symptoms |
| Stage I | High white blood cell count with lymph node swelling | No anemia or low platelets |
| Stage II | Enlarged spleen or liver, may have swollen lymph nodes | No anemia or low platelets |
| Stage III | Anemia develops (low red blood cell count) | May have lymph node, spleen, or liver enlargement |
| Stage IV | Low platelet count (thrombocytopenia), increased bleeding risk | Other features may be present |
The Binet Staging System (Europe, Australia)
| Stage | Description |
|---|---|
| Stage A | Less than three areas of enlarged lymph tissue; normal red cell and platelet counts |
| Stage B | Three or more areas of enlarged lymph tissue; normal red cell and platelet counts |
| Stage C | Any number of lymph areas; low red cell count and/or low platelet count |
Both the Rai and Binet systems help doctors determine prognosis and guide the timing and type of treatment. Earlier stages (Rai 0–II, Binet A–B) often require only monitoring, while advanced stages (Rai III–IV, Binet C) usually need treatment.
Acute Lymphoblastic Leukemia (ALL) Classification
ALL is an aggressive, rapidly progressing leukemia mainly affecting children and young adults. It does not have a traditional staging system. Instead, the disease is classified by:
- Type of lymphocyte affected (B-cell or T-cell)
- Genetic mutations or chromosomal abnormalities
- Extent of disease spread (such as to the central nervous system)
For practical treatment purposes, ALL is often described in phases:
- Untreated: Newly diagnosed with leukemia cells in blood or marrow and symptoms present.
- In remission: Leukemia cells undetectable after treatment, normal blood counts restored. Small amounts of disease may still remain (minimal residual disease).
- Relapsed: Disease returns after period of remission with leukemia cells reappearing in blood, marrow, or other organs.
Factors affecting prognosis and treatment include age, white blood cell count at diagnosis, and specific chromosomal or genetic changes.
Acute Myeloid Leukemia (AML) Classification
Like ALL, AML is classified, not staged, since it is aggressive and typically already systemic at diagnosis. The French-American-British (FAB) classification and genetic/molecular features are commonly used. Physicians assess:
- Number of healthy blood cells
- Subtype of myeloid cell affected
- Presence of genetic mutations (such as FLT3-ITD, NPM1)
- Response to induction therapy (untreated, in remission, relapsed)
Prognosis and treatment options depend heavily on these cellular and molecular characteristics.
Chronic Myeloid Leukemia (CML) Phases
Instead of stages, CML is classified by phases based on disease progression:
- Chronic phase: Most patients are diagnosed here; few symptoms, elevated white blood count, best prognosis.
- Accelerated phase: Disease worsens, blood counts become more abnormal, symptoms may increase.
- Blast phase (blast crisis): CML behaves like an acute leukemia, white blood cell precursors (blasts) rise dramatically, symptoms worsen, prognosis is poorer.
The presence of the Philadelphia (Ph) chromosome, a genetic translocation, is key to diagnosis and targeted therapy decisions.
Rare Subtypes: B-cell and T-cell Prolymphocytic Leukemia (B-PLL, T-PLL)
These are rare, aggressive leukemias that do not have formal staging systems. Classification is based on:
- Type (B-cell or T-cell)
- Blood cell counts
- Presence or absence of organ enlargement (spleen, liver, lymph nodes)
B-PLL and T-PLL usually require prompt treatment due to rapid disease progression.
Factors Affecting Leukemia Progression
Besides cell counts and presence in organs, several factors influence how leukemia will behave:
- Patient age: Younger patients often have better outcomes.
- Cytogenetic and molecular findings: Certain mutations or chromosomal abnormalities (such as the Philadelphia chromosome in CML) affect prognosis and therapy choices.
- Presence of symptoms: Symptoms like anemia, infections, bleeding, or organ enlargement typically indicate more advanced disease.
- Response to treatment: Achieving and maintaining remission improves long-term survival chances.
Leukemia Staging and Treatment Decisions
Staging and classification directly inform treatment:
- Early-stage or favorable-risk: Some patients, particularly with CLL, may not need immediate treatment and undergo active monitoring.
- More advanced or higher-risk: Most acute leukemias and advanced stage CLL/CML require immediate intervention.
Treatment options may include:
- Chemotherapy
- Targeted therapy (such as tyrosine kinase inhibitors for CML)
- Biologic therapy
- Radiation therapy (for CNS involvement or specific cases)
- Stem cell transplantation
- Surgery (such as spleen removal in select cases)
The goal is to eliminate leukemia cells, restore healthy blood production, and achieve remission.
Monitoring Leukemia and Minimal Residual Disease
Even after remission, minimal residual disease (MRD) may remain. Sensitive laboratory techniques are used to detect low levels of leukemia cells that could lead to relapse. Ongoing monitoring with blood tests and, sometimes, bone marrow biopsies is critical for long-term management.
Prognosis and Survival by Stage or Classification
Prognosis is closely tied to:
- Leukemia subtype and stage or phase at diagnosis
- Age and general health
- Cytogenetics and molecular markers
- Early response to treatment
Generally, earlier stages and favorable genetic features are linked to better outcomes, but individual prognoses vary widely.
Frequently Asked Questions (FAQs)
How is leukemia different from other cancers when it comes to staging?
Leukemia does not form solid tumors—cancerous cells usually circulate in the blood and bone marrow, so staging is based on lab findings and organ involvement rather than tumor size and metastatic sites.
Why do some types of leukemia have formal stages and others don’t?
Chronic forms like CLL have a slower course and defined stages (Rai and Binet) that correlate with symptoms and cell counts. Acute leukemias (ALL, AML) are so aggressive and systemic at diagnosis that traditional staging is less useful, so classification focuses on cell types and genetic markers instead.
How does staging affect treatment plans?
Staging helps determine whether “watchful waiting” is appropriate (early CLL), if urgent chemotherapy is needed (acute leukemia), or whether other advanced therapies (like stem cell transplant) should be considered.
What are the main factors used in leukemia classifications?
Doctors consider the type of leukemia cell, blood and bone marrow counts, chromosomal and genetic changes, and the involvement of organs such as lymph nodes, spleen, or liver.
Can leukemia be cured?
The outlook depends on leukemia type, stage, genetics, response to treatment, and overall health. Some forms, such as certain pediatric ALL cases and many with successful stem cell transplantation, can be cured, while others may be controlled long-term as a chronic disease.
Key Takeaways
- Leukemia staging and classification are critical in guiding treatment and predicting prognosis.
- Chronic types like CLL have formal staging systems (Rai, Binet); acute types rely on cell-type classification and treatment response.
- Diagnosis, treatment plans, and long-term monitoring depend on a mix of laboratory findings, genetic markers, and patient health factors.
References
- https://bloodcancerunited.org/resources/blog/stages-leukemia-understanding-classification-and-progression
- https://www.moffitt.org/cancers/leukemia/diagnosis/stages/
- https://www.cancer.org.au/cancer-information/types-of-cancer/leukaemia
- https://www.uchealth.org/diseases-conditions/leukemia/
- https://my.clevelandclinic.org/health/diseases/4365-leukemia
- https://www.mayoclinic.org/diseases-conditions/leukemia/symptoms-causes/syc-20374373
- https://www.cancercenter.com/cancer-types/leukemia/stages
- https://www.nyp.org/cancer/blood-cancer/leukemia/symptoms
- https://www.pennmedicine.org/conditions/leukemia
- https://www.pfizer.com/disease-and-conditions/leukemia
Read full bio of Sneha Tete