Leukemia After COVID-19: Exploring Possible Connections and Risks
Investigating the complex relationship between COVID-19 and leukemia risk, outcomes, and what current research shows.
Leukemia After COVID-19: Is There a Connection?
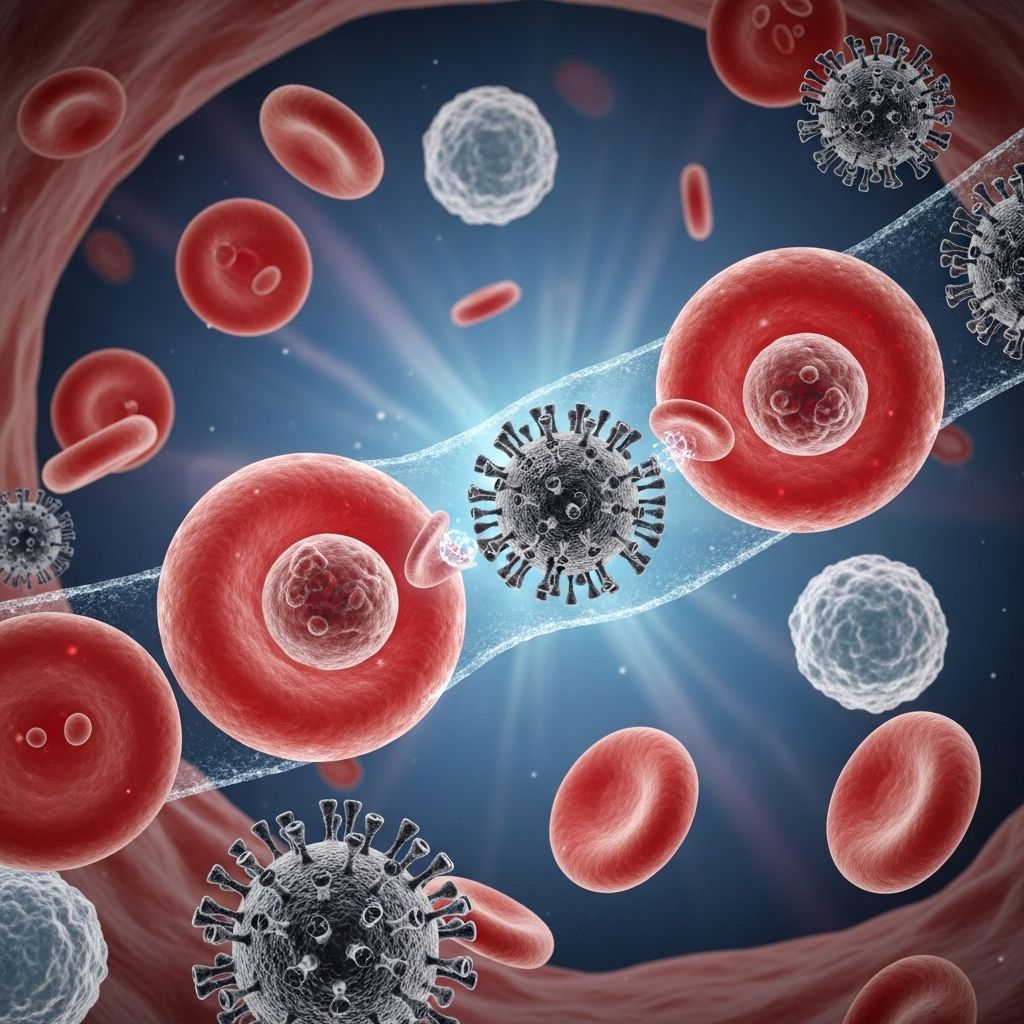
Since the global spread of COVID-19, researchers have worked tirelessly to understand its impact not only as a respiratory illness, but also its broader effects on immune and blood systems. One pressing question is whether a COVID-19 infection may increase the risk of developing leukemia or affect outcomes in those with existing blood cancers.
Understanding Leukemia and COVID-19
Leukemia is a type of cancer that starts in blood-forming tissues, usually the bone marrow, causing the body to produce abnormal blood cells. There are multiple subtypes, including:
- Acute myeloid leukemia (AML)
- Chronic lymphocytic leukemia (CLL)
- Acute lymphoblastic leukemia (ALL)
- Chronic myeloid leukemia (CML)
Since early 2020, COVID-19 has been observed to have significant implications for people with these and other blood cancers, especially in terms of infection risk and disease severity. However, questions remain regarding its potential role in initiating or accelerating the development of leukemia itself.
COVID-19 and Leukemia: What Does the Research Say?
Approximately over 500 million people worldwide have contracted COVID-19. For most, the disease is mild, but those living with leukemia face heightened risks. A 2021 study presented at the American Society of Hematology Annual Meeting reported that people with blood cancer had a 17% chance of mortality from COVID-19 infection, which is significantly higher than in the general population.
While the evidence is strong that people with leukemia are more vulnerable to severe COVID-19, the data is much less clear about the virus as a possible cause or contributor to new leukemia cases. Some scientists have suggested mechanisms by which COVID-19 could, in theory, influence oncogenesis (the formation of cancer), but robust proof is still lacking.
Key Points on COVID-19 and Leukemia Risk
- Some researchers propose COVID-19 may play a role in leukemia formation, especially in combination with other risk factors, but no direct link is proven yet.
- Case studies have described acute or chronic leukemia manifesting shortly after a COVID-19 infection, but these instances remain rare.
- Theoretical frameworks suggest COVID-19’s effect on the immune system or genetic mutations could be contributory, though data remain preliminary.
- Other viruses have established links to blood cancers, lending plausibility to COVID-19 as a potential, albeit unproven, contributor.
Potential Mechanisms: How Could COVID-19 Contribute to Leukemia?
Current hypotheses rest on two main mechanisms:
- Abnormal Immune Response to Viral Infection: An intense or dysregulated immune reaction during viral illnesses, including COVID-19, can potentially trigger genetic mutations or create microenvironments in bone marrow that favor cancer cell growth.
- Interaction with Renin-Angiotensin System: The virus responsible for COVID-19 (SARS-CoV-2) interacts with the renin-angiotensin system—a hormone system that regulates blood pressure and fluid balance—which may have indirect effects on the development of blood cancers.
What Have Case Reports Shown?
Clinical evidence remains limited to case reports, which cannot establish causation but may highlight possible associations.
- Case 1: Acute Myeloid Leukemia (AML) – A 61-year-old man developed AML 40 days after COVID-19 infection. Researchers did not conclusively determine whether the infection caused leukemia, as the link may be coincidental. The patient’s leukemia notably entered remission without conventional therapy, a phenomenon previously observed but rare.
- Case 2: Chronic Lymphocytic Leukemia (CLL) – Another report featured a man whose first sign of CLL appeared shortly after recovering from COVID-19. In this case, lymphocyte counts doubled in just four weeks.
While intriguing, experts caution that these reports are not sufficient to suggest every COVID-19 survivor is at greater risk for leukemia, but they do warrant further investigation.
Comparison: COVID-19 and Other Viruses in Blood Cancer Development
The connection between viral infection and blood cancer is not unprecedented. Several other pathogens have welle stablished associations with leukemia or lymphoma:
| Virus/Pathogen | Associated Cancer | Mode of Transmission |
|---|---|---|
| Human T-cell leukemia virus type 1 (HTLV-1) | T-cell leukemia | Bodily fluids (e.g., blood, breast milk) |
| Epstein-Barr virus (EBV) | Lymphoma, nasopharyngeal carcinoma | Saliva, close contact |
| Hepatitis C virus | Lymphoma | Blood, sexual contact |
| Plasmodium falciparum (malaria parasite) | Lymphoma | Mosquito bites |
| Helicobacter pylori (bacterium) | Lymphoma (MALT type) | Oral ingestion (contaminated food/water) |
Given these precedents, it is plausible that severe or persistent immune stimulation from viral illness, such as COVID-19, could play a contributing role in rare cases.
Risk Factors and Prognosis for People with Leukemia and Prior COVID-19 Infection
Those already diagnosed with a blood cancer are known to face higher risks from COVID-19 complications. Important findings include:
- Patients with active leukemia or myelodysplastic syndromes (MDS) at COVID-19 diagnosis are more likely to experience severe illness or require intensive care.
- Neutropenia, a low white blood cell count common in leukemia, is associated with more severe outcomes from COVID-19.
- Being in remission at the time of COVID-19 diagnosis tends to offer a better prognosis.
- Receiving ongoing cancer treatment does not significantly increase risk of death from COVID-19 for these patients, according to registry data.
Impact of COVID-19 Vaccination
The ability of people with leukemia or other blood cancers to develop immunity after COVID-19 vaccination is another area of concern:
- Roughly 15% of people with blood cancers failed to generate detectable antibodies after vaccination in observational studies.
- Those with lymphoma or undergoing active cancer therapy are least likely to mount a strong immune response post-vaccine.
- It may be advisable to vaccinate or give booster doses before starting intensive therapy, whenever possible.
- Continued precautions such as masking and social distancing may be recommended even after vaccination for immunocompromised individuals.
Summary Table: COVID-19, Leukemia, and Outcomes
| Factor | Effect on COVID-19 Severity | Leukemia Risk/Development |
|---|---|---|
| Existing Leukemia (untreated or active) | Significantly increases risk of severe COVID-19 | – |
| COVID-19 infection | Severe if pre-existing blood cancer present | Theoretical, unproven risk in rare cases |
| COVID-19 vaccination | Reduces severity and mortality risk | No evidence of increased leukemia risk |
| Neutropenia at COVID-19 diagnosis | Higher risk of ICU-level care required | – |
| History of other viral infections | Varies by virus | Established risk for some viruses (e.g., HTLV-1, EBV) |
Frequently Asked Questions (FAQs)
Can COVID-19 directly cause leukemia?
There is no direct evidence that COVID-19 causes leukemia. However, a few case reports describe new leukemia diagnoses following a COVID-19 infection. Most experts believe a direct causal link remains unproven, and such cases may be coincidental.
Are people with leukemia more at risk from COVID-19?
Yes. Individuals with blood cancers such as leukemia are at significantly higher risk for severe COVID-19 illness, intensive care admissions, and mortality compared with the general population.
Is it safe for people with leukemia to get the COVID-19 vaccine?
Vaccination is strongly recommended for people with leukemia, but they may have reduced immune responses. Approximately 15% of people with blood cancers did not develop detectable antibodies after vaccination, so continued protective measures are advised.
Should cancer treatment be delayed for vaccination?
Some experts suggest that if possible, cancer treatment (such as chemotherapy) could be delayed to allow time for COVID-19 vaccination or booster shots to improve immune response, but any decision should be individualized and discussed with a hematologist.
Which other viruses are linked to blood cancers?
Several, including human T-cell leukemia virus type 1 (HTLV-1), Epstein-Barr virus (EBV), hepatitis C, and Plasmodium falciparum (malaria parasite), have established relationships with various leukemias and lymphomas.
Key Takeaways
- There is no definitive evidence that COVID-19 infection causes leukemia, although research is ongoing and some rare cases have prompted scientific inquiry.
- People with leukemia or blood cancers are at higher risk of severe COVID-19 and should follow expert recommendations for prevention and vaccination.
- Talk to a hematologist or oncologist if you have concerns about new symptoms after COVID-19 or about timing COVID-19 vaccination with cancer treatment.
- Ongoing studies are needed; updates to clinical guidance will follow as research clarifies these complex relationships.
References
- https://www.hematology.org/newsroom/press-releases/2021/covid-19-takes-a-toll-on-people-with-blood-cancers-and-disorders
- https://www.healthline.com/health/leukemia/leukemia-after-covid
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8366460/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9367547/
- https://www.healthline.com/health-news/blood-cancers-a-look-at-the-latest-treatments-and-their-promise
- https://www.nature.com/articles/s41375-023-01893-1
Read full bio of Sneha Tete












