Leg Pain and Heart Attack: What Your Symptoms May Really Mean
Understand the link between persistent leg pain, peripheral artery disease, and your heart health—know when to take action.
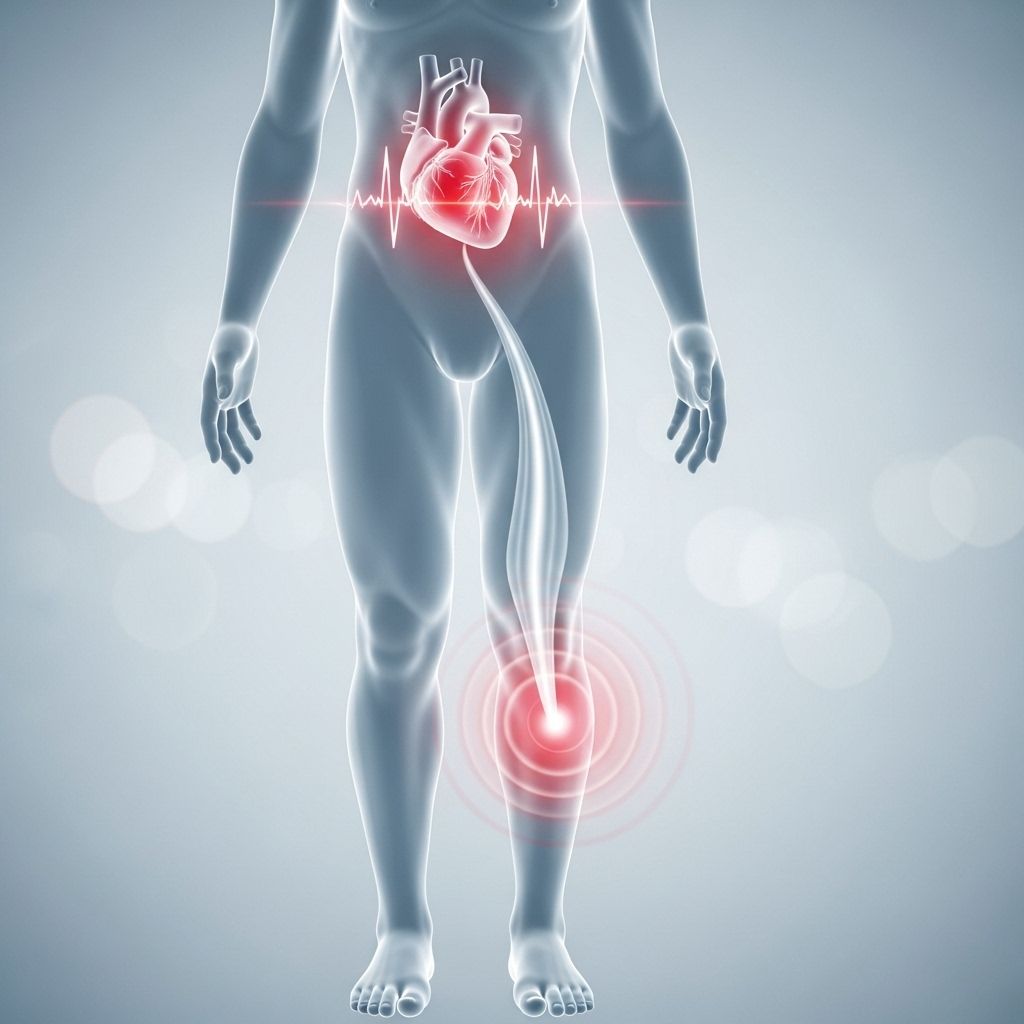
Most people associate heart attacks with classic symptoms such as intense chest pain, difficulty breathing, or discomfort radiating into the left arm or jaw. But what about pain, cramping, or weakness in your legs? Could these symptoms be a warning sign from your heart—or are they unrelated?
Is Leg Pain a Symptom of a Heart Attack?
Leg pain alone is not considered a typical early symptom of a heart attack. When a person is having an acute heart event, hallmark symptoms tend to involve the chest, upper back, arms, jaw, or neck. Nevertheless, leg pain can sometimes be a sign of underlying cardiovascular problems that may increase the risk of a heart attack in the future.
- Classic heart attack symptoms are upper-body: chest pain, pressure, shortness of breath, lightheadedness, pain in the jaw or arms.
- Leg pain is not a direct symptom of a heart attack, but may signal vascular problems affecting heart health.
- The most common vascular link is peripheral artery disease (PAD).
How Can Heart and Vascular Conditions Cause Leg Pain?
Your body’s circulatory system prioritizes blood flow to vital organs such as the brain, heart, and kidneys. The lower extremities—legs and feet—rely on healthy arteries and veins to maintain strong circulation, and any cardiovascular dysfunction can affect blood delivery and return, leading to specific symptoms in the legs.
Three main heart- and vascular-related causes of leg pain include:
- Peripheral Artery Disease (PAD): Narrowing of arteries in the legs due to plaque buildup (atherosclerosis) reduces blood flow, causing pain, especially during exertion.
- Congestive Heart Failure: Weak pumping action can lead to swelling (edema) and heaviness in the legs.
- Venous Thromboembolism (VTE): Blood clots in the legs can cause sudden pain and swelling; this may be linked to heart disease risk.
Of these, PAD is the most closely associated with incremental—often unnoticed—leg symptoms that can indicate a broader cardiovascular problem.
Understanding Peripheral Artery Disease (PAD)
Peripheral artery disease is a chronic condition caused by atherosclerosis, the gradual buildup of fatty plaques inside the arterial walls. It most commonly impairs blood flow to the legs and feet but shares the same roots as coronary artery disease (CAD), setting the stage for future heart attacks and strokes.
| PAD Symptom | Typical Manifestation |
|---|---|
| Cramping | Especially in the calves, thighs, hips during activity (walking, climbing stairs); relieved by rest. |
| Pain/Aching | Dull, persistent discomfort that increases with physical effort. |
| Fatigue or Weakness | Loss of leg strength while exercising or moving. |
| Numbness | Tingling, cold feeling, especially in feet or lower legs. |
| Slow-healing sores/ulcers | Nonhealing wounds around toes, feet, or legs. |
| Color/temp changes | Coolness, shiny or pale skin, especially compared to the other leg. |
Why Does PAD Matter for Heart Health?
PAD is not only a problem for your legs. The same atherosclerotic process that narrows leg arteries may also affect the coronary arteries that supply the heart, greatly increasing your risk of heart attack and stroke. Studies suggest:
- People with PAD are much more likely to have underlying coronary artery disease (CAD) or cerebrovascular disease.
- 46–68% of people with PAD have CAD or similar vascular conditions.
- Recognizing PAD early can motivate lifestyle changes or medical interventions that improve both leg and heart health.
Who Is at Risk for Peripheral Artery Disease?
PAD becomes more common as people age, but several risk factors raise your chances:
- Diabetes (type 1 or 2)
- Smoking (current or history)
- Obesity (BMI > 30)
- High blood pressure (hypertension)
- Age 50 or older
- Family history of heart disease or stroke
Certain populations, such as Black Americans, face a higher incidence of PAD and are less likely to be promptly diagnosed or treated due to disparities in healthcare access and awareness. This disparity can result in a higher risk of advanced symptoms and complications.
Leg Pain from Other Causes
While vascular disease is a major consideration, leg pain can originate from many sources. Common non-cardiac causes include:
- Muscle strain or overuse (after exercise or physical labor)
- Acute injury (sprains, fractures, falls)
- Chronic conditions (osteoarthritis, nerve disorders)
- Varicose veins or venous insufficiency
If your leg pain is clearly tied to a recent incident, improves with rest, and doesn’t occur with activity, it’s more likely musculoskeletal. However, persistent or unexplained symptoms warrant medical evaluation.
When Is Leg Pain a Sign of a More Serious Heart Problem?
Pain in the legs should not be a daily occurrence. Most normal discomfort stems from physical activity or identifiable minor trauma. However, chronic, worsening symptoms—especially those that come on with activity and stop with rest—may point to PAD or another circulatory problem.
- Be alert if leg pain worsens with walking and subsides with rest.
- Pay special attention if leg pain is accompanied by chest pain, shortness of breath, or faintness—these combined symptoms could indicate an acute reduction in blood flow to the heart or a pending cardiac event.
- Sudden, severe leg pain, redness, or swelling may indicate a blood clot, which is a medical emergency.
Diagnosing PAD and Related Conditions
If you or your doctor suspect PAD or other vascular problems, you may undergo several diagnostic steps:
- Physical examination of leg pulses and skin.
- Ankle-Brachial Index (ABI): Compares blood pressure in the legs vs. arms to identify flow reduction.
- Imaging tests: Ultrasound, CT angiography, or MRI may be used to visualize arteries.
- Blood tests: Identify diabetes, cholesterol issues, or clotting abnormalities.
Treatment and Prevention: What You Can Do
The most effective treatments both relieve symptoms and reduce your overall cardiac risk. Strategies include:
- Lifestyle modifications:
- Quit smoking
- Maintain a healthy weight
- Exercise regularly (walking and leg exercises can improve symptoms and circulation)
- Adopt a heart-healthy diet low in saturated fat and sodium
- Medication:
- Statins to lower cholesterol
- Blood pressure control
- Blood sugar management (for diabetes)
- Antiplatelet drugs (aspirin or others) to prevent clotting
- Procedures:
- In severe cases, angioplasty or bypass surgery to restore blood flow
- Wound care for nonhealing ulcers
Complications of Untreated PAD
If left untreated, PAD can result in significant complications:
- Critical limb ischemia (severe blockage resulting in persistent pain, tissue damage, and risk of limb loss)
- Increased risk of heart attack and stroke
- Nonhealing ulcers, infections, or gangrene
Prompt attention can significantly reduce these risks and improve both quality and length of life.
When to See a Doctor
Contact your healthcare provider if you notice:
- New, persistent, or worsening leg pain, especially with activity
- Pain accompanied by chest discomfort, shortness of breath, or faintness
- Sores, changes in skin color or temperature, or unexplained swelling in your legs or feet
- Loss of pulses or numbness in your feet or toes
Do not self-diagnose or ignore progressive symptoms. Early intervention is vital for preventing serious complications.
Frequently Asked Questions (FAQs)
Can leg pain be the only symptom of a heart attack?
No, leg pain alone is not a typical heart attack symptom. Heart attacks usually involve chest pain, pressure, or discomfort radiating to the arms, neck, or jaw. Leg pain is more linked to circulatory issues like PAD, but vascular disease increases the overall risk for heart attack.
What does PAD leg pain feel like compared to normal soreness?
Pain from PAD often starts with activity (like walking) and goes away with rest. It may feel like cramping, aching, or fatigue—especially in the calves or thighs. Regular muscle soreness usually improves with stretching or after rest, and is linked to specific activities.
How common is PAD?
PAD affects about 6.5 million Americans aged 40 and older, but it is often undiagnosed due to subtle or slow-developing symptoms. Risks rise sharply with age, smoking history, diabetes, and hypertension.
Are Black Americans at higher risk for PAD?
Yes, studies show Black Americans face a much higher risk of PAD but often have less access to timely diagnosis and care. Closing this gap relies on improving healthcare access, awareness, and screening in high-risk communities.
Can treating PAD lower my risk for heart attack?
Absolutely. Treatments for PAD—lifestyle changes, medicines, and sometimes procedures—also lower the risk of major cardiac events. Early diagnosis and ongoing care are key to protecting heart and vascular health.
Key Takeaways
- Leg pain is rarely the first sign of a heart attack but may signal underlying conditions that raise your risk for serious heart problems.
- Pain, cramping, or weakness with activity—especially in people with risk factors—could indicate PAD. PAD itself dramatically increases the risk of a future heart attack or stroke.
- Persistent, worsening, or unexplained leg pain deserves prompt medical evaluation, especially when paired with other symptoms like chest pain or shortness of breath.
- Addressing PAD and cardiovascular risk factors early can improve both leg symptoms and future heart health.
References
- https://www.healthcentral.com/condition/heart-attack/leg-pain-heart-attack
- https://www.healthline.com/health/heart-attack/leg-pain-heart-attack-symptoms
- https://www.bch.org/latest-news/2023/october/dr-john-mcneil-painful-leg-cramping-can-signal-y/
- https://www.bidmc.org/about-bidmc/wellness-insights/heart-health/2018/06/leg-pain-pad-warning-signs
- https://www.mercyheartcenter.org/heart/staying-healthy/heart-attack-symptoms/
- https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
- https://medlineplus.gov/ency/patientinstructions/000775.htm
- https://bidplymouth.org/news-stories/all-news-stories/stories/2025/02/what-does-leg-pain-have-to-do-with-the-heart
- https://ascentcardiology.com/your-leg-and-arm-pain-could-indicate-a-more-severe-heart-related-illness/
Read full bio of medha deb












