Understanding Left Ventricular Diastolic Dysfunction: Causes, Symptoms, Treatment, and Outlook
Explore the causes, symptoms, diagnosis, and management of left ventricular diastolic dysfunction, a key contributor to heart failure.
Understanding Left Ventricular Diastolic Dysfunction (LVDD)
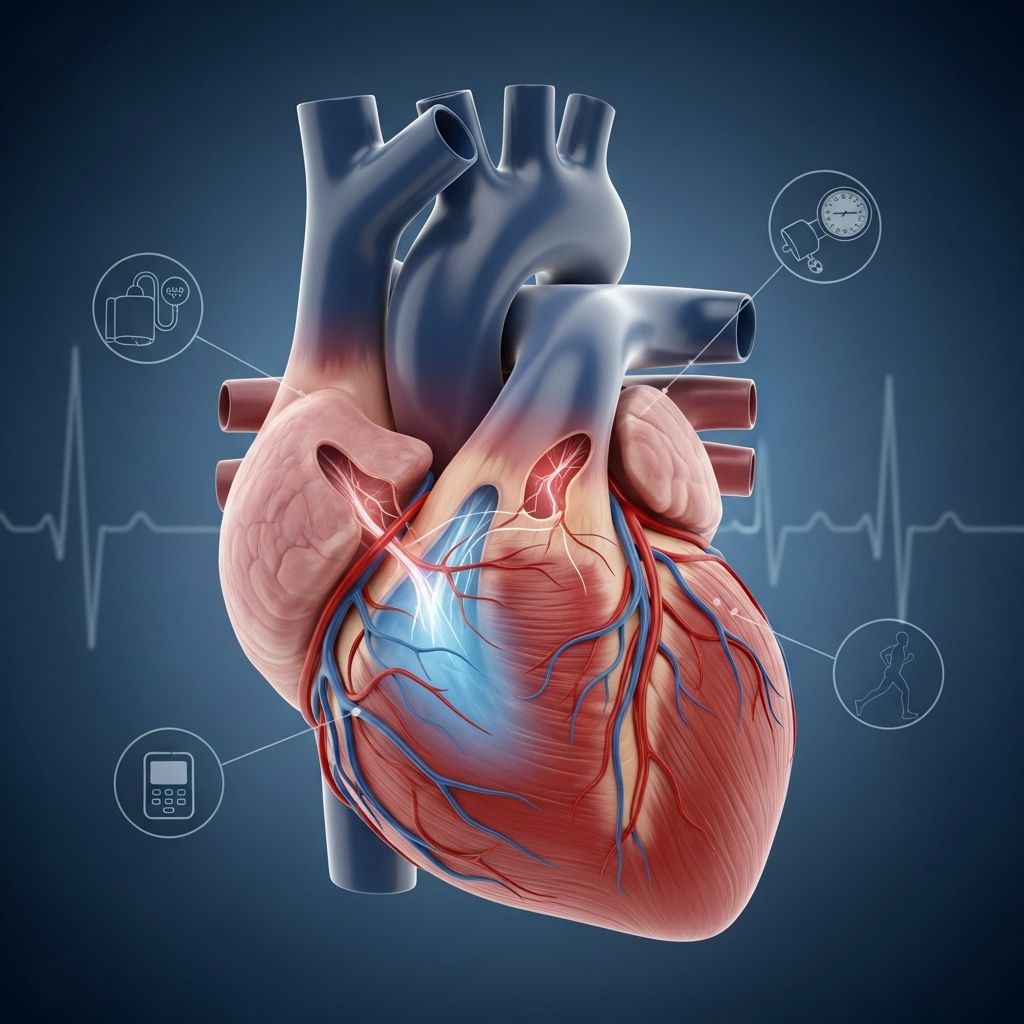
Left ventricular diastolic dysfunction (LVDD) is a heart condition marked by the left ventricle’s reduced ability to fill with blood during the heart’s relaxation phase, known as diastole. This impairment can substantially affect your heart’s function and is a significant risk factor for developing heart failure, especially heart failure with preserved ejection fraction (HFpEF).
In a healthy heart, each beat is divided into two phases: systole (the heart contracts and pumps blood) and diastole (the heart relaxes and fills with blood). When diastolic function is compromised, the ventricle cannot relax and stretch properly, resulting in less blood filling the chamber and therefore less blood being pumped out to the body during the next beat.
Causes of Left Ventricular Diastolic Dysfunction
The most common cause of LVDD is advancing age. As people get older, the heart muscle, especially the left ventricle, tends to lose elasticity, making it stiffer and less able to fill optimally.
- By middle age, the risk of developing diastolic dysfunction is estimated to be between 27% and 43%.
- For those age 85 and older, up to 88% may experience some degree of diastolic dysfunction.
Several medical conditions also increase the risk of developing LVDD, including:
- Atrial fibrillation (AFib): This irregular heart rhythm can disrupt normal blood filling of the ventricle.
- Coronary artery disease: Blockages in coronary arteries reduce blood supply to heart muscle, causing stiffening.
- Diabetes: Chronically high blood sugar damages heart muscle and increases stiffness.
- Hypertension: Long-standing high blood pressure causes the ventricle to thicken and lose flexibility.
- Obesity: Excess body weight strains the heart and increases the risk of related comorbidities.
Other less common causes may include chronic kidney disease, certain genetic conditions, and rarely, infiltrative diseases or cancer treatments.
How Does LVDD Affect the Heart?
During diastole, the heart muscle should relax and fill efficiently. In LVDD, the ventricle becomes stiff or thickened, preventing adequate filling. The heart must compensate by generating higher pressures to force blood into the stiff chamber. This leads to elevated pressures in the lungs and systemic circulation, resulting in symptoms and complications.
| Normal Heart | Heart with LVDD |
|---|---|
| Ventricle relaxes and fills easily | Ventricle is stiff and fills poorly |
| Low filling pressure | High filling pressure |
| Optimal cardiac output | Reduced cardiac output |
| Minimal risk of congestion | Fluid backs up into lungs/body |
Grading Diastolic Dysfunction
Medical professionals categorize diastolic dysfunction into grades to indicate severity:
- Grade 1 (Impaired Relaxation): The earliest stage, with mild impairment and few or no symptoms.
- Grade 2 (Pseudonormalization): Moderate dysfunction; the heart attempts to compensate, so filling appears normal but is actually abnormal on special imaging studies.
- Grade 3 (Restrictive Filling): Severe, advanced stage distinguished by markedly impaired filling and often significant symptoms. This form is often called restrictive cardiomyopathy.
Diagnosis and grading are conventionally performed via echocardiography, which assesses blood flow patterns and filling pressures in the heart chambers.
Symptoms of Left Ventricular Diastolic Dysfunction
LVDD often goes unnoticed in its early stages, as symptoms may be mild or absent. As the dysfunction advances, symptoms may resemble those of general heart failure and include:
- Shortness of breath during activity, rest, or when lying flat due to fluid buildup in the lungs.
- Fatigue or weakness, as the heart cannot meet the body’s energy demands.
- Swelling (edema) in the legs, ankles, feet, or abdomen resulting from fluid accumulation.
- Sudden weight gain due to fluid retention.
- Difficulty exercising or reduced ability to exert yourself.
- Orthopnea: Needing to sleep with extra pillows due to breathlessness when lying flat.
- Paroxysmal nocturnal dyspnea: Waking up at night short of breath.
- Trouble concentrating or memory issues because of reduced blood flow to the brain.
- Irregular or rapid heartbeat.
- Lack of appetite and nausea.
Not everyone with LVDD will experience all these symptoms, and they can be mistakenly attributed to aging or other illnesses.
Diagnosis of LVDD
Diagnosing LVDD can be challenging because symptoms are often subtle and can overlap with other conditions. Your healthcare provider will begin with a detailed health history, focusing on symptoms, risk factors, and other medical conditions.
- Physical examination: Checks for signs such as leg swelling, lung congestion, and abnormal heart sounds.
- Echocardiogram: An ultrasound test that provides detailed images and measurements of heart structure and function. Doppler studies show blood flow and filling patterns.
- Electrocardiogram (ECG): Records the heart’s electrical activity, detecting rhythm abnormalities that may contribute to LVDD.
- Laboratory tests: May include blood tests such as B-type natriuretic peptide (BNP) to confirm or rule out heart failure.
- Other tests: Cardiac MRI, chest X-ray, or, rarely, cardiac catheterization for direct pressure and flow measurement.
Early diagnosis is crucial to manage risk factors and slow disease progression.
Risk Factors for Developing LVDD
- Older age
- High blood pressure (hypertension)
- Coronary artery disease
- Obesity
- Diabetes mellitus
- Atrial fibrillation
- Chronic kidney disease
- Genetic predisposition
Controlling these risk factors can greatly reduce the chances of LVDD leading to symptomatic heart failure.
Treatment Options for Left Ventricular Diastolic Dysfunction
There is no single cure for LVDD. Instead, treatment focuses on:
- Managing underlying conditions: Tight control of blood pressure, diabetes, and other comorbidities is paramount.
- Lifestyle modifications: Diet, exercise, and maintaining a healthy weight are crucial.
- Medications:
- Diuretics to eliminate extra fluid and relieve symptoms like swelling and breathlessness.
- Blood pressure medicines (ACE inhibitors, ARBs, beta-blockers) to protect the heart and reduce workload.
- Medications to control heart rate or rhythm if there’s atrial fibrillation or arrhythmia.
- Treatment for underlying ischemic heart disease when present.
- Monitoring and regular checkups: To track disease progression and adjust therapies as needed.
For patients with sleep apnea (which can worsen LVDD), treating sleep disordered breathing with CPAP or other therapies is also recommended.
Additional Strategies
Newer research is investigating the role of:
- SGLT2 inhibitors (originally for diabetes), which have shown promise in some forms of heart failure.
- Mineralocorticoid receptor antagonists, to reduce fibrosis and improve outcomes in heart failure patients.
Outlook and Prognosis
Many people with LVDD remain asymptomatic for years, especially when the condition is detected early and risk factors are well managed. However, because LVDD is a progressive condition, the chance of progressing to overt heart failure increases over time in the presence of ongoing risk factors.
Important points about prognosis include:
- People with well-controlled risk factors can have a good quality of life and often avoid heart failure symptoms for many years.
- When LVDD leads to heart failure, particularly heart failure with preserved ejection fraction (HFpEF), the outlook can be variable, but advances in heart failure therapy have improved patient survival and quality of life.
- Regular follow-up and active risk factor control are essential for the best prognosis.
Frequently Asked Questions (FAQs)
Q: How does diastolic dysfunction differ from systolic dysfunction?
A: Systolic dysfunction occurs when the heart can’t contract well (pumping problem), often resulting in a low ejection fraction. Diastolic dysfunction is a filling problem— the heart can contract normally, but is stiff and doesn’t fill with blood effectively. Ejection fraction is often normal in LVDD.
Q: Who is most at risk for LVDD?
A: Older adults, individuals with long-standing high blood pressure, diabetes, obesity, atrial fibrillation, or coronary artery disease are at the highest risk.
Q: Can left ventricular diastolic dysfunction be reversed?
A: While the stiffening of the ventricle is usually not fully reversible, controlling risk factors and treating related health conditions can improve symptoms, slow the progression, and possibly prevent heart failure.
Q: What lifestyle changes help control LVDD?
A: Eating a heart-healthy diet (low in salt and saturated fats), regular physical activity, weight control, good blood sugar and blood pressure management, not smoking, and avoiding excessive alcohol can all help.
Q: Is LVDD dangerous if I don’t have symptoms?
A: Even without symptoms, LVDD may progress over years, especially with uncontrolled risk factors. Regular checkups are important for monitoring and intervention.
Takeaway: Key Points About Left Ventricular Diastolic Dysfunction
- LVDD is a common age-related condition impacting the heart’s ability to relax and fill.
- It frequently coexists with hypertension, diabetes, obesity, and atrial fibrillation.
- Symptoms can range from subtle to severe and may resemble those of classic heart failure.
- Diagnosis is best achieved via echocardiogram and supportive tests.
- Management focuses on risk factor control, lifestyle changes, and treating related medical conditions.
- Early detection and proactive care may help prevent progression to symptomatic heart failure and preserve quality of life.
References
- https://www.healthline.com/health/heart-failure/left-ventricular-diastolic-dysfunction
- https://hightowerclinical.com/blogs/chronic-diastolic-heart-failure/
- https://www.upmc.com/services/pulmonology/conditions/diastolic-dysfunction
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3748656/
- https://www.baptisthealth.com/care-services/conditions-treatments/diastolic-heart-failure
- https://my.clevelandclinic.org/health/diseases/22950-diastolic-heart-failure
- https://www.mayoclinic.org/diseases-conditions/heart-failure/symptoms-causes/syc-20373142
- https://www.webmd.com/heart-disease/heart-failure/what-is-diastolic-heart-failure
Read full bio of Sneha Tete












