Learning to Live with Wet Age-Related Macular Degeneration
Strategies, treatments, and everyday adjustments to successfully manage life with wet age-related macular degeneration.
Introduction
Wet age-related macular degeneration (wet AMD) is a leading cause of vision loss among older adults, characterized by rapid deterioration of central vision. While there is currently no cure, advancements in treatments and practical lifestyle strategies can help those diagnosed with wet AMD maintain independence and quality of life. This article explores symptoms, diagnosis, treatment options, daily living adaptations, and supportive resources for people learning to live with wet AMD.
Understanding Wet AMD
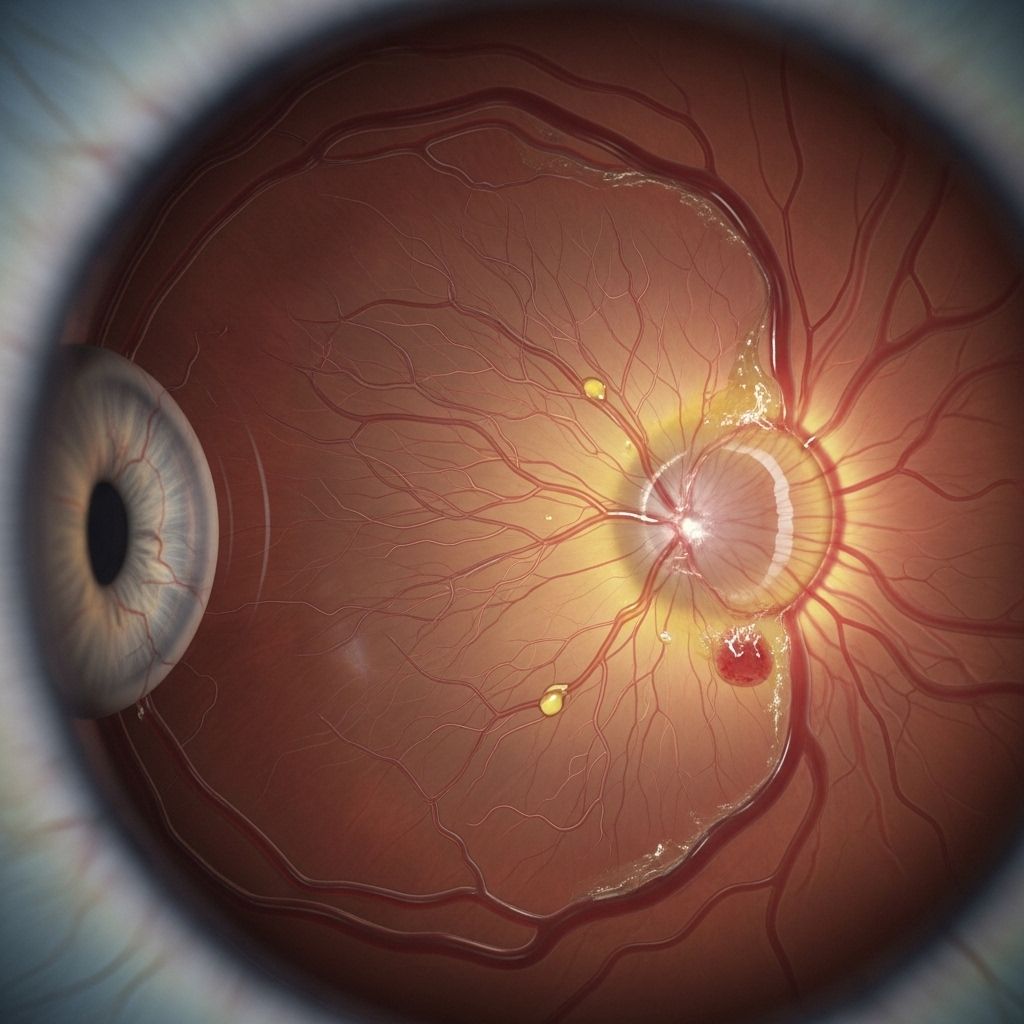
Wet AMD is distinguished from dry AMD by the abnormal growth and leaking of blood vessels beneath the retina, specifically under the macula—the region responsible for sharp, central vision. The leakage of blood and fluid into the retinal tissue promptly damages this critical area, resulting in more rapid vision loss compared to the slow progression typical of dry AMD.
What Is the Difference Between Dry and Wet AMD?
| Feature | Dry AMD | Wet AMD |
|---|---|---|
| Progression Speed | Gradual (years) | Rapid (weeks/months) |
| Main Cause | Macula atrophy | Abnormal blood vessels |
| Central Vision Loss | Slow decline | Sudden & severe |
| Treatment Focus | Lifestyle, supplements | Medical, injection & laser therapy |
Symptoms and Early Detection of Wet AMD
The symptoms of wet AMD can appear suddenly and progress quickly. Early identification is crucial to minimizing permanent vision loss and maximizing outcomes from available treatments. Recognizing the warning signs and knowing how to monitor changes is an essential first step.
- Blurry or blank spot in central vision: Appears like a gray, black, or red spot where faces and details become hard to recognize.
- Distorted images: Straight lines, door frames, or text appear bent or wavy.
- Color and shape changes: Objects may seem smaller, larger, duller or darker than before.
- Sensitivity to light: Difficulty adjusting between dark and bright environments.
- Visual hallucinations (Charles Bonnet syndrome): Sometimes, the brain creates images, such as patterns or animals, in response to lost vision. These are not a sign of mental illness but may occur as the mind compensates.
- Difficulty with low-light vision: Reduced ability to see or discern objects in dim lighting.
The Importance of Early Eye Exams
Those over 55 are advised to have regular, annual dilated eye exams. This is because subtle changes in vision, such as the initial stages of dry AMD, often precede wet AMD and can be missed without professional examination.
How to Self-Monitor with the Amsler Grid
One practical tool for early detection and ongoing monitoring is the Amsler grid:
- Hold the grid at a comfortable reading distance, using reading glasses if necessary.
- Cover one eye and focus on the dot in the center.
- Check if straight lines look wavy, blurry, or missing.
- If any distortion or blank spots appear, contact your ophthalmologist promptly.
Treatment Options for Wet AMD
While there is currently no cure for wet AMD, modern medicine offers several avenues to slow or manage its progression. The primary goal of treatment is to stabilize vision and prevent further damage to the macula.
Common Treatments
- Anti-VEGF Injections: The leading therapy, these medications (such as ranibizumab, aflibercept, and bevacizumab) are injected directly into the eye. They work by blocking vascular endothelial growth factor—preventing the growth and leakage of abnormal blood vessels.
- Laser Therapy: High-energy lasers may be used to seal abnormal blood vessels, preventing further leaking. This option is less common than anti-VEGF injections and may be used selectively.
- Photodynamic Therapy: This involves the use of a light-activated drug injected into the bloodstream, which is then activated in the eye using a specific wavelength of laser light. This targets and destroys abnormal blood vessels beneath the retina.
- Gene and Stem Cell Therapies: Clinical trials and ongoing research are assessing long-term solutions that could repair retinal tissue or reduce the frequency of treatments, potentially reducing the burden of injections.
Risks and Side Effects
Anti-VEGF injections are generally considered safe but may carry risks such as eye discomfort, infections (endophthalmitis), or increased eye pressure. Discuss all treatment options and potential risks thoroughly with your retina specialist.
Lifestyle and Home Approaches
- Dietary Support: Eating a nutrient-rich diet, particularly foods high in antioxidants (leafy greens, fruits, fish high in omega-3 fatty acids), may help support overall eye health.
- AREDS Supplements: The AREDS and AREDS2 studies have shown that specific vitamins and minerals—especially for those with dry AMD—may slow progression. While their effect is less pronounced in wet AMD, supplementation can still benefit overall macular health.
- Smoking cessation: Smoking accelerates AMD progression and increases risk for vision loss. Quitting can have a measurable impact.
Adapting Daily Life for Wet AMD
Living with central vision loss requires creative adaptation. With practical modifications and modern low vision devices, many people continue to manage daily tasks, maintain independence, and enjoy life.
Tips for Everyday Living
- Improved Lighting: Use adjustable lamps, task lighting, and daylight bulbs to increase facility when reading, cooking, or navigating spaces.
- Contrast and Color: Choose home items with high color contrast (for example, dark mugs on white countertops) to improve depth perception and identification.
- Large Print Materials: Utilize books, magazines, and digital displays with large, readable font sizes.
- Magnifying Devices: Employ handheld or electronic magnifiers for reading, hobbies, and detail work.
- Technology Adaptations: Personal devices and computers often offer accessibility settings (text-to-speech, screen magnification, voice commands).
- Labeling and Organization: Use tactile labels and keep essential items in consistent locations.
- Mobility Training: Orientation and mobility specialists can teach techniques for safely navigating public spaces and crossing streets.
- Supportive Services: Consider vision rehabilitation, occupational therapy, and local low vision organizations for personalized guidance.
Addressing Emotional and Mental Health
- Emotional Impact: Rapid changes in vision can lead to feelings of loss, frustration, or isolation. Support groups, counseling, and peer networks offer practical and emotional support.
- Charles Bonnet Syndrome: Visual hallucinations caused by the brain’s response to vision loss can be unsettling. Recognizing these as normal parts of reduced vision—and talking openly with a care provider—can help reduce anxiety.
Maintaining Independence
With the right combination of medical management, adaptive strategies, and community resources, people with wet AMD can continue to pursue hobbies, travel, and social engagement. Regular collaboration with eye care professionals is essential to timely intervention and maximizing vision preservation.
Frequently Asked Questions (FAQs)
What is the main difference between wet and dry AMD?
Wet AMD is caused by the abnormal growth of leaky blood vessels in the macula, leading to rapid central vision loss. Dry AMD occurs due to gradual atrophy of retinal cells and causes slower vision changes.
How quickly can symptoms develop?
Symptoms of wet AMD can appear suddenly, sometimes within days, and rapidly worsen if not treated. Immediate medical attention is advised if new blind spots, distortions, or color changes occur.
Can wet AMD be cured?
Currently, wet AMD cannot be cured. Treatments can slow vision loss, stabilize vision, and sometimes even improve it, with regular anti-VEGF injections being most effective.
Is it still possible to read and perform daily tasks after diagnosis?
Yes. With visual aids, enhanced lighting, and adaptive strategies, many people continue to read, cook, and maintain independence, even with central vision loss.
Are hallucinations with vision loss a sign of mental illness?
No. Visual hallucinations in the context of vision loss (Charles Bonnet syndrome) are a normal response of the brain to reduced visual input and not indicative of psychiatric illness.
Resources and Support for Living Well
The journey with wet AMD is best managed with a holistic approach, combining medical care, technology, social support, and personal adaptation. Consider these additional resources:
- Low Vision Centers: Specialized clinics provide assessment, training, and device recommendations.
- National and Local Organizations: Groups such as the Macular Society, BrightFocus Foundation, and local blindness support networks offer information, assistance, and peer connections.
- Access Technology: Smartphone apps, screen readers, and wearable AI devices continue to expand possibilities for independent living.
- Transportation Services: Many cities have public and volunteer transport programs to assist those with visual impairments.
Conclusion
While wet AMD poses significant challenges, early diagnosis, adherence to treatment, and adoption of adaptive strategies enable people to live full, active lives. Continuing collaboration with eye care professionals, openness to assistive technologies, and engagement with supportive communities provide the tools needed to sustain independence and well-being even in the face of central vision loss.
References
- https://www.healthline.com/health/eye-health/wet-amd-treatments-outlook-and-more
- https://www.brightfocus.org/resource/symptoms-of-wet-age-related-macular-degeneration/
- https://www.medicalnewstoday.com/articles/wet-macular-degeneration-treatment
- https://www.medicalnewstoday.com/articles/symptoms-of-wet-amd-progression
- https://www.novartis.com/news/media-releases/new-novartis-analysis-shows-wet-amd-patients-achieved-sustained-fluid-control-faster-beovu-versus-aflibercept
- https://www.healthline.com/health/macular-degeneration
- https://medlineplus.gov/maculardegeneration.html
- https://www.ncbi.nlm.nih.gov/books/NBK572147/
Read full bio of Sneha Tete












