Understanding Latent Autoimmune Diabetes in Adults (LADA)
LADA is a slow-progressing form of autoimmune diabetes, often misdiagnosed as type 2, requiring special awareness for diagnosis and management.
Latent autoimmune diabetes in adults (LADA) represents a unique, slow-progressing form of autoimmune diabetes that often presents diagnostic challenges due to its overlap with both type 1 and type 2 diabetes. Sometimes referred to as “type 1.5 diabetes,” LADA typically affects adults and is frequently misdiagnosed, resulting in delayed optimal treatment. This article offers an in-depth look at LADA, exploring its features, diagnosis, treatment, and why awareness is essential for patients and healthcare providers alike.
What is LADA?
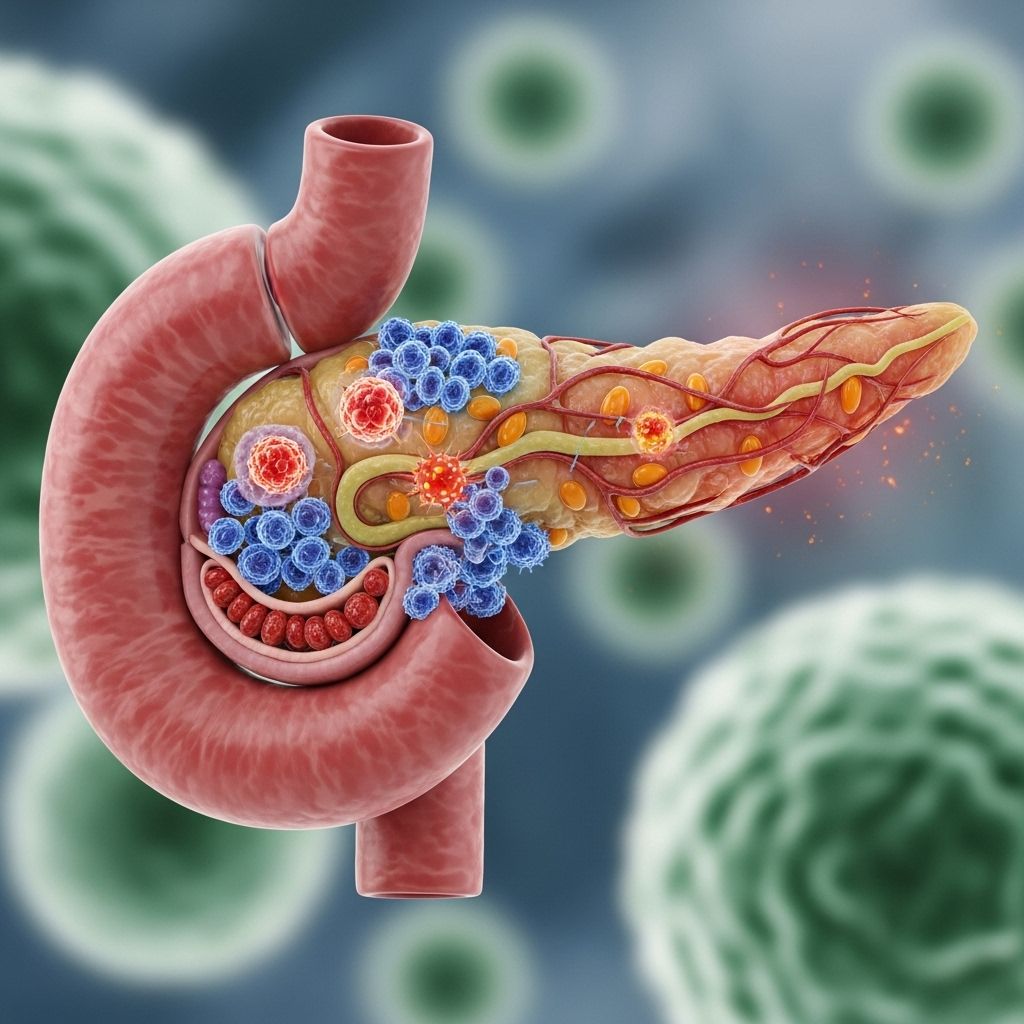
LADA stands for latent autoimmune diabetes in adults. It is a subtype of diabetes in which the body’s immune system slowly destroys the insulin-producing cells of the pancreas, much like in type 1 diabetes. However, in LADA, this autoimmune process progresses more gradually, allowing affected individuals to initially maintain some degree of insulin production, sometimes for months or even years after diagnosis .
- LADA is typically diagnosed in people over 30 years old.
- The onset is slower than classic type 1 diabetes but leads to complete insulin deficiency eventually.
- It may share some clinical features with type 2 diabetes, such as initial responsiveness to oral medication and lifestyle interventions.
- Over time, most with LADA will require insulin therapy as their own insulin production declines.
Understanding the characteristics and challenges of LADA is crucial, as the misdiagnosis can lead to improper treatment and increased risks of complications.
Is LADA Different from Type 1 or Type 2 Diabetes?
LADA is often called “type 1.5 diabetes” because it encompasses characteristics of both type 1 diabetes (T1D) and type 2 diabetes (T2D).
| Feature | Type 1 Diabetes | Type 2 Diabetes | LADA |
|---|---|---|---|
| Typical Age of Onset | Childhood or adolescence | Usually adults (but also some children) | Adults (over 30) |
| Cause | Autoimmune destruction of beta cells | Insulin resistance +/- reduced insulin production | Autoimmune, slow beta cell destruction |
| Initial Treatment | Insulin | Diet, exercise, oral meds; may progress to insulin | Diet, exercise, possibly oral meds, eventually insulin |
| Autoantibodies Present | Yes | No | Yes |
| Rate of Beta Cell Loss | Rapid | Variable, slow | Intermediate; gradual (months to years) |
| Insulin Dependence | Immediate | May occur after years | Delayed but inevitable |
Because of its clinical overlap, many healthcare professionals view diabetes on a continuum, with LADA bridging the gap between type 1 and type 2 diabetes. This can result in initial misdiagnosis, most frequently as type 2 diabetes, especially in adults who do not fit the typical profile of type 1 diabetes .
Who Gets LADA?
LADA develops most often in adults older than age 30. It is relatively uncommon in children and young teenagers. While there is a genetic predisposition—those with a family history of autoimmune diseases may be more prone—LADA can affect adults of any demographic background and body type.
- About 4% to 14% of adults initially diagnosed with type 2 diabetes may, in reality, have LADA .
- LADA can affect adults who are lean or physically active, as well as those who are overweight or inactive .
- Many people with LADA have no obvious risk factors aside from age and autoimmune predisposition.
Due to the later age of onset, some may initially overlook autoimmune diabetes as a possible diagnosis, increasing the likelihood of confusion and suboptimal treatment in early stages.
What Causes LADA?
The underlying cause of LADA is an autoimmune attack on the beta cells of the pancreas. Scientists believe that, like classic type 1 diabetes, LADA occurs when the immune system mistakenly targets insulin-producing cells, gradually reducing the body’s insulin reserves.
- The exact trigger is not entirely understood, though genetic and environmental factors likely play a role .
- Unlike typical type 2 diabetes, there is no evidence that insulin resistance is the primary cause of LADA, although some overlap can occur.
- The progression of cell destruction is typically slower than in type 1 diabetes.
- Currently, there are no confirmed methods to prevent LADA, as the autoimmune process is not under conscious control .
This chronic autoimmune process ultimately results in the need for insulin therapy as natural insulin production wanes.
How Is LADA Diagnosed?
LADA is often misdiagnosed as type 2 diabetes due to similarities in presentation and the age of affected individuals. Accurate diagnosis requires specialized testing and a high index of suspicion, especially in adults who do not fit the classic profile for type 2 diabetes.
- Diagnosis is typically considered in adults with diabetes who are non-obese, physically active, or have lost weight without explanation and whose blood sugar remains difficult to control despite oral medications .
- If you have symptoms such as excessive thirst, frequent urination, or unexplained weight loss, especially if you are over 30 and newly diagnosed with diabetes, ask your doctor about testing for LADA.
Key Diagnostic Tests for LADA:
- Glutamic Acid Decarboxylase (GAD) Antibodies: The most commonly used test, it detects the presence of antibodies that attack pancreatic beta cells.
- Islet Cell Antibodies (ICA): Presence of these autoantibodies further supports an autoimmune cause.
- C-peptide Test: Measures how much insulin the pancreas is producing. Low or declining C-peptide levels indicate declining beta-cell function, typical in LADA .
People with high GAD antibody levels and lower C-peptide are more likely to need insulin sooner. Comprehensive diagnosis may require a combination of clinical presentation, laboratory results, and monitoring of response to therapies.
How Does LADA Progress?
LADA typically progresses as a slowly unfolding process. Unlike the near-total and rapid insulin dependence seen in classic type 1 diabetes, people with LADA often maintain some pancreatic function for months or even years after initial diagnosis .
- At first, blood sugar may be managed with diet, exercise, and oral medications (such as metformin).
- Because the autoimmune attack continues, insulin production steadily declines over time.
- Eventually, most people with LADA will require insulin injections, often within months or years after diagnosis, depending on the progression rate.
The variability in the rate of progression underscores the need for close monitoring by healthcare providers to adjust therapy appropriately and avoid complications.
How Is LADA Managed?
Effective management of LADA requires an individualized approach that balances initial non-insulin therapies with a timely transition to insulin as needed. Early and accurate diagnosis is critical, as continuing non-insulin interventions alone in someone whose body is losing its ability to make insulin can cause persistent high blood sugars and long-term complications.
Typical Management Plan:
- Lifestyle Interventions: Healthy eating, maintaining an active lifestyle, and weight management (if appropriate) are foundational for all types of diabetes management.
- Oral Medications: Some people manage blood sugar with oral diabetes medications for a time, particularly early in LADA.
- Insulin Therapy: As endogenous insulin production declines, insulin injections become necessary.
- GLP-1 Receptor Agonists: Medications in this category (such as dulaglutide, liraglutide, semaglutide) have shown benefits in some people with LADA unless C-peptide levels are already very low .
- Regular Monitoring: Frequent check-ups allow timely adjustments in therapy and screening for diabetes-related complications.
Working closely with a healthcare provider—or ideally, a diabetes care team—is essential for managing the changing needs associated with the condition. Early introduction of insulin is sometimes debated, but delayed insulin therapy after significant beta-cell loss can contribute to poor glycemic control and complications. Personalized care, based on antibody levels, C-peptide measurement, age, and other factors, is recommended .
Complications and Risks Associated with LADA
If LADA is not recognized and managed appropriately, the following complications may occur:
- Persistent Hyperglycemia: Chronically high blood sugars elevate the risk for complications.
- Diabetes Ketoacidosis (DKA): In rare cases, particularly if insulin is delayed or omitted when it becomes necessary, DKA can occur, which is a medical emergency .
- Long-Term Complications: The risk for eye, kidney, nerve, and vascular complications rises with poor glycemic control, similar to other forms of diabetes.
Early recognition and treatment—and not hesitating to transition from oral medications to insulin in appropriate cases—helps reduce the risk of these complications.
Can LADA Be Prevented?
LADA is not currently preventable because it is driven by autoimmune factors that cannot be modified by lifestyle choices. Currently, there are no proven ways to stop or delay the immune attacks on pancreatic cells once they have begun. Early diagnosis and prompt management are the best strategies to reduce risk of complications .
Living Well with LADA
Receiving a diagnosis of LADA can be confusing and emotionally challenging, especially when initial therapies prove less effective over time. However, many people go on to live full, active lives by focusing on self-care, education, and open communication with their healthcare team.
- Stay informed about your type of diabetes and its changing needs.
- Regularly attend medical appointments and report any new or changing symptoms.
- Work with your healthcare provider to create flexible and responsive management plans.
- Make use of support resources, such as diabetes education classes or support groups.
Frequently Asked Questions (FAQs)
What are the main symptoms of LADA?
Typical symptoms include increased thirst, frequent urination, unexplained weight loss, and fatigue. LADA tends to develop more gradually than type 1 diabetes, so people may not notice symptoms until blood sugar is significantly elevated.
Why is LADA often misdiagnosed?
Because LADA develops in adults and initially responds to oral diabetes medications, it is commonly mistaken for type 2 diabetes. Hallmarks of LADA, such as a lack of typical risk factors for type 2 diabetes (like obesity or family history), may be overlooked.
How is LADA diagnosed?
Diagnosis involves testing for pancreatic autoantibodies (such as GAD or ICA) and measuring C-peptide levels to assess residual insulin production. These tests help differentiate LADA from type 2 diabetes.
Is insulin always needed right away in LADA?
Not always. Many with LADA can manage with diet, exercise, and oral medications initially. However, as insulin production declines, most individuals will eventually need insulin therapy.
What should I do if I suspect I have LADA instead of type 2 diabetes?
Contact your healthcare provider and discuss your concerns. Ask about antibody and C-peptide testing, particularly if you are lean, active, or not responding to standard type 2 treatments.
Can LADA be prevented?
Currently, there is no way to prevent LADA since it is caused by autoimmune factors. Early detection and appropriate management remain the best options to reduce complications.
Summary Table: LADA vs. Type 1 and Type 2 Diabetes
| Feature | Type 1 Diabetes | Type 2 Diabetes | LADA |
|---|---|---|---|
| Age at Onset | Childhood/Adolescence | Adult (any age) | Adult (> 30 years) |
| Insulin at Diagnosis | Required | Not initially | Not initially, but within months/years |
| Autoimmune Nature | Yes | No | Yes |
| Rate of Progression | Rapid | Slow | Intermediate |
| Response to Oral Agents | No | Yes | Yes, initially |
If you or a loved one has recently been diagnosed with diabetes and the condition does not seem to respond as expected to standard treatments, discuss the possibility of LADA with your healthcare team. Early diagnosis, individualized management, and ongoing support can help minimize complications and promote long-term well-being.
References
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/faqs/latent-autoimmune-diabetes-in-adults-lada-what-is-it
- https://my.clevelandclinic.org/health/diseases/lada-diabetes
- https://ce.mayo.edu/online-education/content/pharmacy-podcast-episode-182-whole-lada-mystery-uncovering-latent-autoimmune-diabetes-adults
- https://www.youtube.com/watch?v=Txqe_CAD43c
- https://www.augustahealth.com/answer/latent-autoimmune-diabetes-in-adults-lada-what-is-it/
- https://www.webmd.com/diabetes/mody-lada-diabetes-symptoms-treatment
- https://www.adcesconnect.org/blogs/lourdes-cross1/2021/11/29/management-of-latent-autoimmune-diabetes-in-adults
Read full bio of medha deb












