Laser Treatment for Diabetic Retinopathy: A Comprehensive Guide
Essential information on laser therapy for diabetic retinopathy, including what to expect, risks, success, and frequently asked questions.
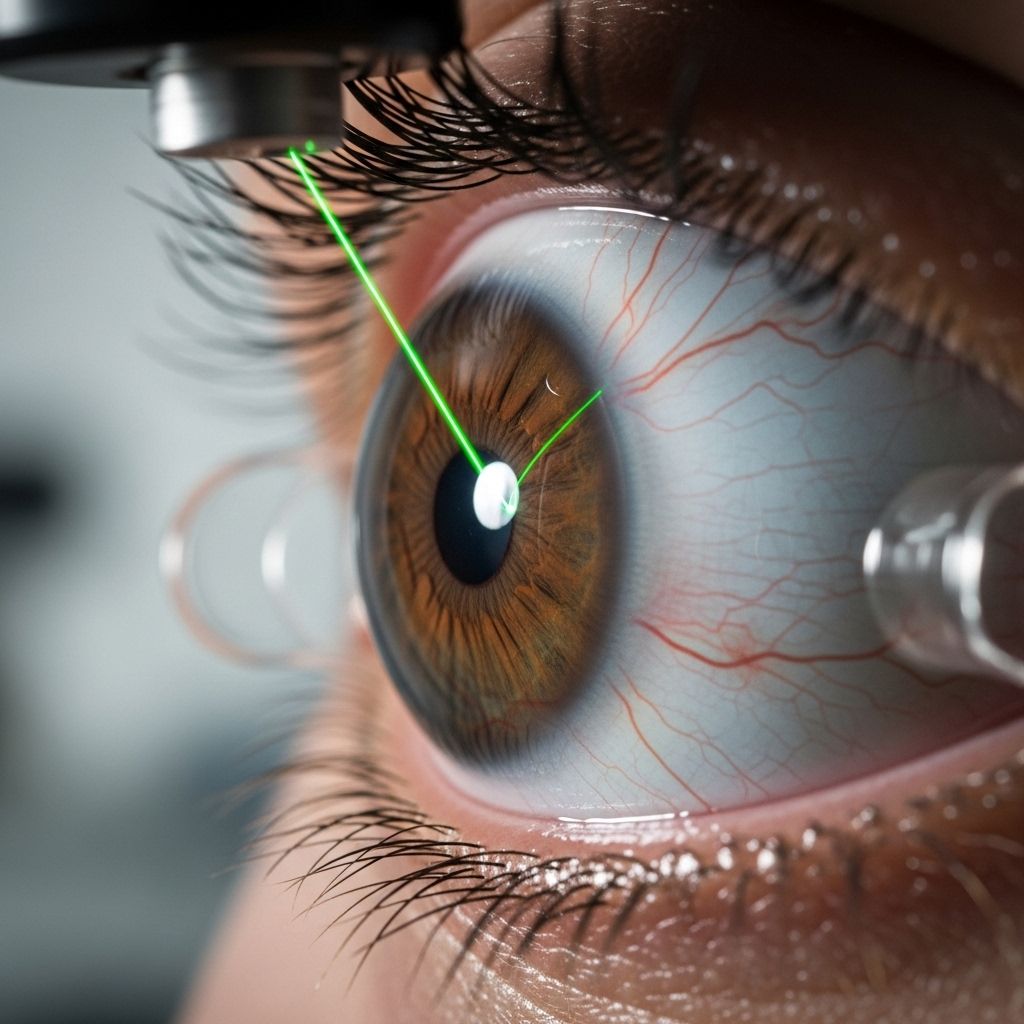
Laser Treatment for Diabetic Retinopathy: What to Expect
Laser therapy has become a crucial intervention in the management of diabetic retinopathy, a complication that affects the blood vessels in the retina of people with diabetes. As a cornerstone of modern ophthalmic care, laser treatment can help arrest or slow retinal damage, helping preserve vision and prevent severe complications. This article offers an in-depth examination of laser therapy’s types, what to expect during and after treatment, the risks involved, typical outcomes, and answers to common questions.
What Is Laser Treatment for Diabetic Retinopathy?
Diabetic retinopathy occurs when high blood sugar damages the small blood vessels of the retina, leading to leakage, abnormal vessel growth, edema (swelling), and in severe cases, vision loss. While there is no cure, laser treatment can significantly reduce progression and vision-threatening complications.
- Prevalence: Over 30% of people with diabetes develop a degree of diabetic retinopathy over their lifetime.
- Main purpose: Laser therapy is aimed at slowing or halting the progression of the disease by selectively treating affected retinal areas.
Types of Laser Therapy
- Photocoagulation Laser Therapy (also called focal or grid laser):
- Targets specific leaking blood vessels or areas of swelling.
- Commonly used for diabetic macular edema (DME), which is swelling at the center of the retina.
- Works by creating tiny burns to stop or slow the leakage and resorb excess fluid.
In addition to laser therapy, it's important to consider other medical treatments available for diabetic retinopathy. Discover the latest developments in management options by visiting our resource on diabetic retinopathy medication treatments, addressing innovative techniques and frequently asked questions that could enhance your understanding and care. - Scatter (Panretinal) Photocoagulation (PRP):
- Applies hundreds of small laser burns across the peripheral retina (away from the macula).
- The goal is to shrink abnormal new blood vessels (neovascularization) seen in advanced stages (proliferative diabetic retinopathy).
- Helps stabilize retina and prevent severe complications like vitreous hemorrhage and retinal detachment.
Both techniques aim to prevent worsening vision, not to restore vision that’s already been irreversibly lost.
Who Is a Candidate for Laser Treatment?
- Typically recommended for people with non-proliferative diabetic retinopathy with significant leakage (focal therapy), or proliferative diabetic retinopathy with abnormal new vessels (PRP).
- Some people may benefit from early intervention if leakage is detected before symptoms appear.
- Criteria for candidacy often include retinal imaging findings (such as fluorescein angiography) that show leakage, swelling, or neovascularization.
What to Expect: Before, During & After Laser Treatment
Before the Procedure
- The treatment typically takes place in an ophthalmologist’s clinic or outpatient setting.
- No general anesthesia is required; you will remain awake throughout the procedure.
- Numbing (anesthetic) eye drops are applied to reduce discomfort.
- The doctor may dilate your pupils to better visualize the retina.
During the Procedure
- You will sit at a slit lamp (an ophthalmic microscope) while the doctor uses a laser attached to the device.
- A special contact lens may be placed on your eye to help focus the laser light.
- When the laser fires, you may perceive bright flashes or short pulses of light.
- Laser sessions usually last 20-40 minutes.
- Multiple sessions may be required depending on the extent of retinal damage and the type of laser therapy.
- Most patients describe the sensation as brief, moderate stinging or discomfort rather than pain.
After the Procedure
- Your vision may be blurry, and eyes may feel sensitive to light or mildly sore for several hours.
- Full recovery can take several days to a week.
- You should avoid driving immediately after the procedure due to blurred vision from dilation and possible glare.
- Most people can return to regular activity within a day, barring individual differences in reaction.
Sometimes additional treatments, such as injections (anti-VEGF or steroids), may be combined with laser therapy to optimize results.
Is Laser Treatment Painful?
- The majority of patients do not find the procedure painful due to the use of numbing drops.
- Some report slight stinging, pressure, or burning that lasts only for moments.
- The sensation is often more uncomfortable than unbearable, and the anticipation may be worse than the experience itself.
The type of laser, treatment intensity, location, and number of burns required influence the level of discomfort.
Risks and Side Effects
While laser treatment is generally safe, several potential risks and side effects should be considered:
- Temporary vision changes: Blurriness, light sensitivity, and mild discomfort are common immediately after the procedure.
- Permanent effects: Some people may experience reduced night vision or peripheral (side) vision, especially after scatter (panretinal) photocoagulation, due to the number of burns applied.
- Macular edema: Swelling of the retina may briefly worsen after laser therapy before improving.
- Rare complications:
- Bleeding inside the eye
- Inadvertent damage to the central retina (macula)
- Formation of scar tissue
- Infection (very rare)
The physician will discuss specific risks with each patient based on findings and overall health status.
Effectiveness and Success Rates
Over decades of study, laser therapy has been consistently shown to reduce the risk of severe vision loss from diabetic retinopathy.
- Large clinical trials have estimated a reduction in risk of vision loss by over 50% in advanced retinopathy treated with laser.
- For macular edema, laser can help stabilize vision and sometimes helps recover some acuity, especially when started early.
- Panretinal photocoagulation is particularly effective in preventing serious complications of proliferative retinopathy, such as retinal detachment and hemorrhage.
However, laser does not restore lost vision, but rather helps maintain current sight and prevent further decline. Outcomes depend on the stage at which treatment is initiated, coexisting eye conditions, and blood sugar control.
Cost and Insurance Coverage
The exact cost of laser treatment for diabetic retinopathy varies based on region, treatment facility, number of sessions, and insurance plan.
- Laser procedures are routinely covered by major insurance companies and public health insurance if medically indicated.
- Out-of-pocket costs can range from several hundred to several thousand dollars per session for uninsured patients.
- Additional costs may include examination fees, imaging, and medications.
- Consult your eye care provider and insurer regarding pre-authorization and financial policies.
Summary and Key Takeaways
- Laser treatment is the standard for halting or slowing progression of diabetic retinopathy, especially in advanced or leaking disease.
- The procedures are generally safe, non-invasive, and cause minimal, brief discomfort due to numbing drops.
- Laser does not improve existing vision loss but protects against further and more severe complications.
- Success is maximized with early intervention, regular screening, and good diabetes management.
- Talk to a qualified eye care specialist to determine if and when laser therapy is right for you.
Frequently Asked Questions (FAQs)
How do I know if I need laser treatment?
Your eye specialist decides based on retinal imaging and the stage of your diabetic retinopathy. Regular eye screening is necessary for all people with diabetes, as vision-threatening changes can occur before symptoms arise.
How long does the procedure take?
Each laser session typically lasts 20 to 40 minutes, though complex cases may require multiple appointments.
Will laser treatment restore my vision?
No. The primary goal is to prevent further vision loss. Vision already lost to severe retinal damage cannot usually be restored with laser.
What happens if I don’t get treated?
Untreated diabetic retinopathy can progress to significant vision loss or blindness. Early intervention greatly improves long-term outcomes.
Is laser the only treatment available?
No. Other options include intravitreal injections (e.g., anti-VEGF drugs), vitrectomy surgery (for advanced cases), and aggressive control of blood sugar and blood pressure. Laser often works best in combination with these strategies.
Are there any lifestyle changes I should make?
Strict blood sugar control, blood pressure management, cholesterol control, regular exercise, and routine eye examinations are all essential for managing diabetic retinopathy before and after laser treatments.
Further Reading and Support
- Schedule regular diabetic eye exams with a retinal specialist or ophthalmologist.
- Ask your healthcare provider about new advances in diabetic retinopathy management, such as anti-VEGF therapy and imaging techniques.
- Contact diabetes support organizations for additional resources.
References
- https://www.healthline.com/health/diabetes/laser-treatment-for-diabetic-retinopathy
- https://joslin.org/services/eye-care-surgery/diabetes-retinopathy-care
- https://www.nei.nih.gov/about/news-and-events/news/laser-treatment-highly-effective-treating-diabetic-retinopathy
- https://www.ccjm.org/content/91/8/503
- https://www.healthline.com/health/surgery-for-diabetic-retinopathy
- https://www.medicalnewstoday.com/articles/diabetic-retinopathy-treatment-cost
- https://www.nei.nih.gov/about/news-and-events/news/laser-treatment-effective-diabetic-retinopathy
- https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.laser-photocoagulation-for-diabetic-retinopathy.tf4075
Read full bio of Sneha Tete












