Kneecap Fractures: Symptoms, Causes, Diagnosis, and Treatment
Comprehensive guide to kneecap fractures, covering causes, symptoms, diagnosis methods, treatment options, and recovery expectations.
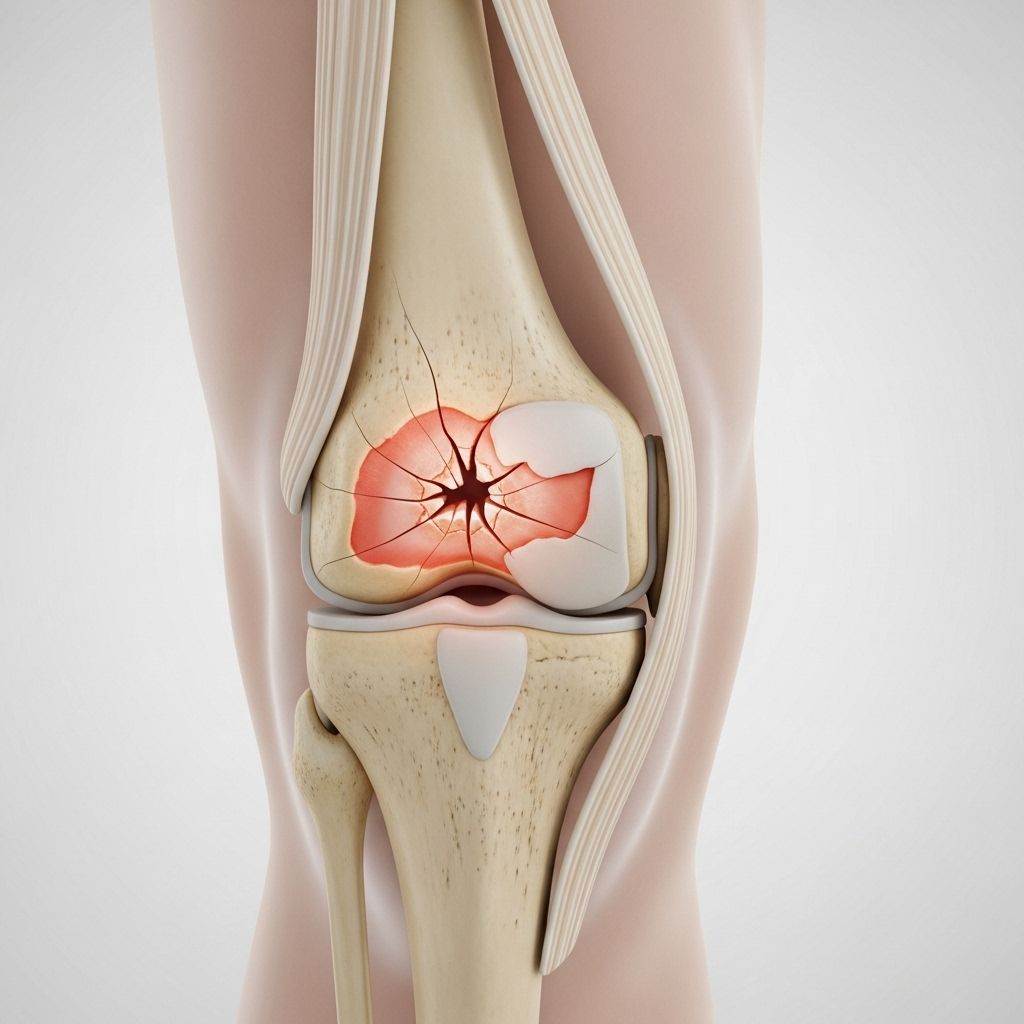
The kneecap, medically known as the patella, is a small, flat bone located at the front of the knee joint. Serving as a shield for the knee, the patella plays a vital role in protecting the joint and aiding movement. Fracture of the kneecap is a significant injury that can impair mobility, causing pain and functional loss. This comprehensive guide explores the causes, symptoms, diagnosis, and treatment of kneecap fractures, and addresses recovery expectations and frequently asked questions.
What is a Kneecap (Patellar) Fracture?
A kneecap fracture is a break in the patella, the bone situated at the front of your knee. This injury typically occurs in response to sudden trauma and can range from a simple crack to more complicated injuries involving multiple bone fragments. The patella not only acts as a shield protecting the knee joint but also makes it possible for the quadriceps muscles to extend the lower leg.
Anatomy of the Patella
- The patella sits between the femur (thighbone) and tibia (shinbone) at the front of the knee.
- The undersurface of the patella and the end of the femur are covered in articular cartilage, ensuring smooth movement during knee flexion and extension.
- Tendons and muscles attach to the patella, enabling extension of the knee.
Causes of Kneecap Fractures
Kneecap fractures are usually caused by direct trauma, but can also result from indirect forces:
- Direct Impact: Most commonly due to a fall directly onto the knee, a blow in contact sports, or hitting the knee against the dashboard in a car accident.
- Indirect Trauma: A sudden, forceful contraction of the quadriceps muscle (for instance, trying to break a fall) can also cause the patella to fracture.
Common Situations Leading to Patellar Fractures
- Falling directly onto the knee on a hard surface
- Getting hit by a fast-moving object (e.g., a helmet in football, a baseball)
- Motor vehicle collisions causing the knee to strike the dashboard
- Severe twisting injuries or sudden strong muscle contractions
Symptoms of a Kneecap Fracture
Kneecap fractures can cause a variety of symptoms, many of which severely limit normal knee function. The most common symptoms include:
- Pain and swelling at the front of the knee
- Bruising around the kneecap
- Inability to straighten or extend the knee
- Difficulty walking, standing, or bearing weight
- Tenderness to touch over the kneecap
- The knee may look deformed or “out of place”, especially if bone fragments have shifted
In some cases, there may be an open wound if the bone pierces the skin, requiring urgent medical attention.
Types of Patellar Fractures
| Type of Fracture | Description |
|---|---|
| Stable (Non-Displaced) | The bone pieces remain aligned. |
| Displaced | Bone fragments have separated and shifted. |
| Comminuted | The bone is broken into three or more pieces. |
| Open (Compound) | The bone breaks through the skin, posing an infection risk. |
| Avulsion | A fragment of the patella is pulled away by attached tendons. |
Special Note: Bipartite Patella
Some people have a bipartite patella, where the patella consists of two separate bones—this is a normal variant, not a fracture.
Diagnosis of Kneecap Fractures
Accurate diagnosis is crucial to guide the best treatment approach. The process typically includes:
Medical History and Physical Examination
- The physician reviews the injury mechanism and symptoms.
- Careful examination of the knee to feel for fractures, deformities, or open wounds.
- Evaluation for hemarthrosis—swelling caused by blood accumulating inside the joint.
- Assessment of the ability to straighten the knee and perform a straight leg raise.
Imaging Studies
- X-rays: The primary imaging test, performed from multiple angles to confirm the presence, location, and extent of the fracture.
- Comparison X-rays may be done on the opposite knee if a bipartite patella is suspected.
Treatment Options for Kneecap Fractures
Treatment of patellar fractures depends on the type of fracture, the degree of bone fragment displacement, the integrity of the surrounding soft tissues, and the patient’s overall health and activity level.
Non-Surgical Treatment
- Stable (non-displaced) fractures may be treated with a cast, splint, or brace to immobilize the knee and allow the bone to heal.
- Typically, weight bearing is limited during early healing, and crutches may be needed.
- Physical therapy may be introduced progressively to restore movement and strength.
Surgical Treatment
Surgery is typically required for fractures where the bone fragments have shifted, the joint surface is misaligned, the leg cannot be straightened, or the fracture is open or comminuted. Surgical approaches include:
- Open Reduction and Internal Fixation (ORIF): Bone fragments are repositioned and secured with hardware such as screws, pins, wires, or a tension band.
- Partial Patellectomy: Removal of a small shattered portion of the kneecap with reattachment of the tendons.
- Total Patellectomy: Rarely, complete removal of the patella may be done for non-reconstructable comminuted fractures.
- Open fracture management: Immediate surgery is needed to clean the wound, prevent infection, and stabilize the fracture.
Examples of Fixation Devices
- Screws and pins
- Tension band wiring
- Metal plates
- Wires or suture techniques for smaller fragments
Recovery and Rehabilitation
Recovery from a patellar fracture varies depending on the severity and type of treatment required. Most patients can expect a lengthy rehabilitation period focused on regaining strength, range of motion, and function.
- Initial phase: Immobilization in a cast or brace, non-weight bearing on the affected leg.
- Physical therapy: Introduced as soon as the healing bone and soft tissues allow—initially focusing on gentle range-of-motion exercises.
- Gradual weight bearing: Your doctor will advise when it is safe to put weight on the leg, typically starting with partial and progressing to full weight bearing.
- Muscle strengthening: Therapy progresses to strengthening exercises for the quadriceps and hamstrings.
- Full recovery: May take several months to a year, depending on patient-specific factors, including bone quality and complexity of the fracture.
Potential Complications of Patellar Fractures
- Stiffness and limited range of motion in the knee
- Weakness in the quadriceps muscle
- Chronic pain or discomfort, especially with kneeling
- Post-traumatic arthritis due to cartilage damage
- Delayed bone healing (non-union or malunion)
- Infection (more common with open fractures)
- Complications from hardware (irritation or need for removal)
Prevention of Patellar Fractures
- Use protective gear: for high-risk activities, such as sports or manual labor.
- Practice fall prevention: especially in older adults, by keeping walkways clear and using non-slip mats.
- Strengthen leg muscles: Regular exercises improve muscle tone, balance, and joint stability.
- Follow road safety: Always use seat belts and ensure proper positioning to minimize dashboard injuries in vehicles.
Frequently Asked Questions (FAQs)
Q: How can I tell if my kneecap is broken?
A: Common signs of a kneecap fracture include severe pain, swelling, inability to straighten or extend the knee, noticeable bruising, and difficulty walking. If you cannot perform a straight leg raise or your knee appears deformed, seek immediate medical attention.
Q: How are kneecap fractures diagnosed?
A: Diagnosis begins with a physical examination, review of your injury history, and common imaging tests, most importantly X-rays. Additional imaging may rule out other injuries or anatomical variants like bipartite patella.
Q: What happens if a kneecap fracture isn’t treated?
A: Untreated kneecap fractures can lead to chronic pain, limited range of motion, inability to straighten the leg, development of arthritis, and possibly permanent disability.
Q: Will I need surgery for a kneecap fracture?
A: Not all kneecap fractures require surgery. Stable, non-displaced fractures usually heal with immobilization. Surgery is typically reserved for displaced, open, or complex (comminuted) fractures.
Q: How long is the typical recovery period after a kneecap fracture?
A: Recovery times vary, but it can take from a few months to over a year for complete healing and rehabilitation. Commitment to physical therapy and gradual return to activity are essential for optimal recovery.
Q: Can patellar fractures cause long-term complications?
A: Yes, possible long-term issues include knee stiffness, persistent weakness, chronic pain, post-traumatic arthritis, and in some cases, the need for additional surgery to remove hardware or address poor healing.
Q: What can I do to help prevent kneecap fractures?
A: Using knee protection during high-risk activities, keeping living spaces safe from falls, and maintaining strong leg muscles reduce your risk. Safe practices while driving can also help prevent traumatic kneecap injuries.
When to See a Doctor
You should seek immediate medical evaluation if you sustain a significant knee injury associated with severe pain, swelling, inability to bear weight or extend the leg, visible deformity, or an open wound over the kneecap. Early diagnosis and prompt treatment are crucial to ensure the best outcome and minimize future complications.
References
- https://www.drjoelcampbell.com/fractures-of-the-patella-orthopedic-sports-medicine-shoulder-specialist-lubbock-tx/
- https://orthoinfo.aaos.org/en/diseases–conditions/patellar-kneecap-fractures/
- https://www.emoryhealthcare.org/conditions/orthopedics/broken-knee
- https://www.jacobcoxmd.com/patella-fracture-orthopaedic-shoulder-elbow-surgeon-ocoee-fl.html
- https://www.bmc.org/patient-care/conditions-we-treat/db/patellar-kneecap-fracture
- https://commonsclinic.com/knee-fracture/
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/f/fractured-kneecap.html
- https://os.clinic/conditions/knee-clinic/kneecap-patella-fracture/
Read full bio of Sneha Tete












