Knee Injections: Types, Benefits, Risks & What to Expect
Comprehensive guide to knee injections for pain relief, including types, benefits, risks, and recovery insights.
Knee pain affects millions of people and can stem from various causes, most commonly osteoarthritis and inflammatory conditions. When medications, physical therapy, and lifestyle changes don’t provide sufficient relief, knee injections may be recommended. These targeted therapies deliver medication directly into the knee joint, offering pain relief and improved mobility without surgery. This guide explores the different types of knee injections, indications, procedure details, benefits, risks, and what to expect before and after treatment.
What Are Knee Injections?
Knee injections are minimally invasive procedures in which medication or other therapeutic agents are injected directly into the knee joint. These injections are primarily performed to:
- Relieve pain and inflammation
- Improve joint mobility and function
- Delay or avoid surgical intervention, such as knee replacement
Knee injections are especially beneficial for patients with:
- Osteoarthritis (OA)
- Rheumatoid arthritis
- Gout
- Persistent knee pain not responding to first-line treatments
Types of Knee Injection Therapies
Several kinds of knee injections exist, each with its own mechanism and indication. The most common are:
Corticosteroid Injections
Corticosteroids are powerful anti-inflammatory medications. When injected into the knee, they rapidly reduce inflammation and pain. These are often used for osteoarthritis, rheumatoid arthritis, and other inflammatory joint diseases.
- Quick pain relief that may last from a few days to several months
- Often used for acute flare-ups or when other approaches have failed
- Can be administered in a clinic or hospital setting
Potential Side Effects of Corticosteroids
- Temporary flare of pain and swelling (“post-injection flare”)
- Skin lightening or thinning at the injection site
- Nerve damage (rare)
- Elevated blood sugar, especially in diabetic patients
- Osteoporosis or bone weakening with repeated injections
Hyaluronic Acid (Viscosupplementation) Injections
Hyaluronic acid (HA) is a natural component of joint fluid, providing lubrication and shock absorption. In osteoarthritis, the quality and quantity of HA decrease.
- HA injections aim to restore lubrication in arthritic knees
- May reduce pain and improve joint movement in some patients
- Pain relief can take several weeks to develop
- The effect, when positive, may last for several months
Not all studies agree on the effectiveness of HA injections; benefit varies between individuals, and they are typically tried after other nonsurgical interventions have been exhausted.
Potential Side Effects of Hyaluronic Acid
- Pain, redness, and swelling at the injection site
- Bleeding and bruising around the joint
- Blistering, rash, or itching
- Rarely, joint infection or allergic reaction
Platelet-Rich Plasma (PRP) Injections
Platelet-rich plasma (PRP) injections use a concentrated solution of a patient’s own blood platelets. The growth factors in PRP are thought to promote tissue repair and reduce inflammation.
- Still considered experimental but increasingly popular for knee osteoarthritis and injuries
- Most widely used when other injection types have failed
- Minimal risk of allergic reaction, since the injection uses the patient’s own blood
Potential Side Effects of PRP
- Temporary pain or swelling at the injection site
- Infection (rare)
Other Injection Types
- Arthrocentesis (joint aspiration): Involves removing excess joint fluid using a needle, often followed by medication injection to relieve pain and swelling.
- Local anesthetics: Sometimes used together with steroids to reduce pain during the procedure.
When Are Knee Injections Recommended?
Knee injections are typically advised for individuals who:
- Have persistent knee pain due to conditions like arthritis
- Have not experienced sufficient relief from oral medications, physical therapy, or other conservative treatments
- Want to postpone knee replacement surgery or are not good candidates for surgery
Injections are not usually the first line of therapy. They are offered when standard measures—such as rest, weight loss, anti-inflammatory drugs, and physical therapy—do not adequately resolve pain and stiffness.
Preparation for a Knee Injection
Generally, little preparation is required for knee injections:
- You may need to inform your doctor about any allergies (especially to medications or latex), current medications, and significant health conditions.
- Blood-thinning medications or certain supplements may need to be paused under medical advice prior to injection.
- No fasting or sedation is typically necessary.
It is recommended to arrange transport home after the injection, particularly if discomfort is anticipated.
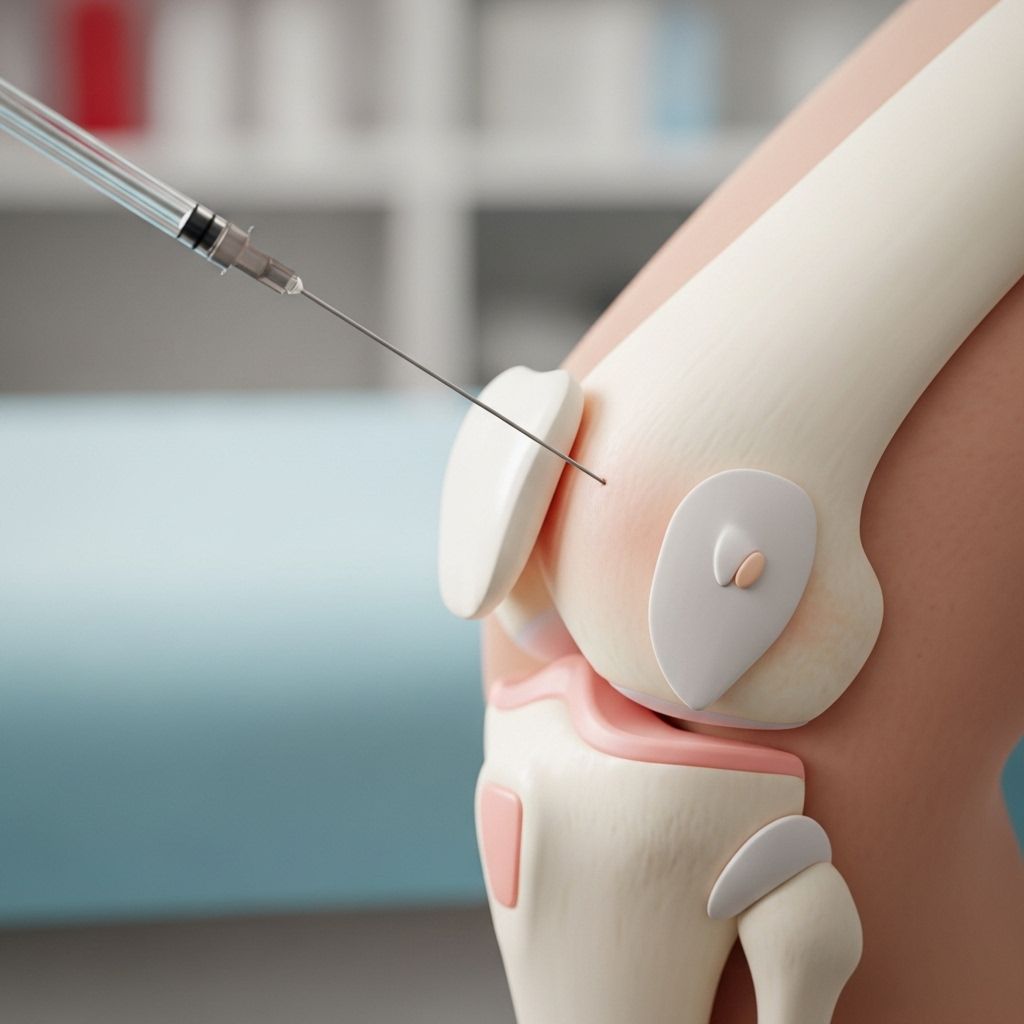
How Are Knee Injections Performed?
The procedure for knee injection is usually quick and performed in an outpatient clinic setting.
- You will sit or lie comfortably with your knee exposed.
- The skin over the injection site is sterilized.
- A local anesthetic may be applied to reduce discomfort.
- A thin needle is gently inserted into the joint space, sometimes with ultrasound guidance for accuracy.
- If there is excess joint fluid, some may be aspirated (removed) before the medicine is injected.
- The chosen medication (steroid, HA, PRP, etc.) is injected.
- The needle is withdrawn, and a small dressing is placed over the site.
Duration of the Procedure
The injection typically takes about 10 to 20 minutes from start to finish.
Aftercare and What to Expect
After the knee injection, you may notice:
- Mild discomfort or soreness at the injection site for up to 48 hours
- Swelling or bruising (which should resolve within a few days)
- A “post-injection flare,” or temporary increase in pain, possible after corticosteroid shots
Most patients can resume gentle daily activities immediately but should:
- Avoid strenuous exercise and weightbearing activities for 1–2 days
- Apply ice to the area to minimize swelling
- Use over-the-counter pain relievers if needed, unless contraindicated
- Contact their doctor if they develop fever, redness, persistent pain, or signs of infection
| Aspect | Key Points |
|---|---|
| Pain Relief | Varies by type: can be immediate (steroids) or require weeks (HA, PRP) |
| Return to Activity | Usually within 24–48 hours for most non-strenuous activities |
| Repeat Injections | Possible with some types (e.g., HA every 6 months); frequency limited for steroids |
Benefits of Knee Injections
- Effective for reducing pain and inflammation in many patients
- Minimally invasive alternative to surgery
- Can delay or prevent the need for total knee replacement
- Short recovery time
Risks and Complications
Knee injections are generally safe. However, as with any procedure, risks and side effects exist:
- Pain or swelling at injection site
- Temporary flare-up of pain or inflammation
- Bleeding or bruising
- Allergic reactions
- Joint infection (rare but serious)
- Nerve or tissue injury (rare)
- Repeated corticosteroid injections may increase risks of cartilage or bone damage
Who Should Not Get Knee Injections?
- Individuals with joint infection or surrounding skin infection
- People with uncontrolled bleeding disorders
- Patients with known allergy to injection components
- Those who have not adequately responded to previous injections
Alternative and Adjunct Treatments
If knee injections are not appropriate or not sufficient, other options may be considered, including:
- Weight management for joint load reduction
- Physical therapy to improve strength and function
- Oral or topical medications for pain relief
- Knee bracing or assistive devices
- Surgical options in advanced cases (such as partial or total knee replacement)
Frequently Asked Questions (FAQs)
How long does it take for a knee injection to work?
Relief from corticosteroid injections may start within 24–48 hours. Hyaluronic acid or PRP injections can take several weeks for effects to become apparent.
How often can I get knee injections?
Frequency depends on injection type. Corticosteroid injections are typically limited to a few times per year to minimize joint and tissue risk. Hyaluronic acid injections may be repeated every 6 months if effective. PRP injections vary based on individual protocol and response.
Are knee injections painful?
Most patients experience only brief discomfort during the injection. A local anesthetic is often used to numb the skin; post-injection soreness usually resolves within a day or two.
Who is a candidate for knee injections?
Patients with knee pain due to arthritis or other joint disorders who have not responded to conservative treatments (like physical therapy, medications, or weight loss) may be candidates.
What should I watch for after a knee injection?
Signs of infection such as fever, redness, warmth, or severe pain require prompt medical attention. Mild swelling and soreness are normal but should improve within 48 hours.
Key Takeaways
- Knee injections are a valuable tool for managing pain and preserving knee function, especially in osteoarthritis and inflammatory conditions.
- A range of injection therapies is available, including corticosteroids, hyaluronic acid, and PRP.
- Risks are generally low, but repeated or inappropriately administered injections may cause harm.
- These procedures are best considered as part of a broader pain management strategy that includes physical therapy, lifestyle changes, and, if needed, surgical intervention.
References
- https://www.volkortho.com/intraarticluar-knee-injection-orthopaedic-sports-medicine-specialist-germantown-maryland/
- https://www.medicalnewstoday.com/articles/310606
- https://www.hopkinsrheumatology.org/2017/02/joint-injections-101/
- https://www.hopkinsarthritis.org/patient-corner/drug-information/hyaluronate-synvisc-hyalgan/
- https://www.hopkinsarthritis.org/arthritis-news/clinical-trials-of-hyaluronic-acid-reflect-significant-publication-bias/
- https://www.youtube.com/watch?v=ApZgaGYfCH4
Read full bio of Sneha Tete












